- Perspective
- General Pediatrics
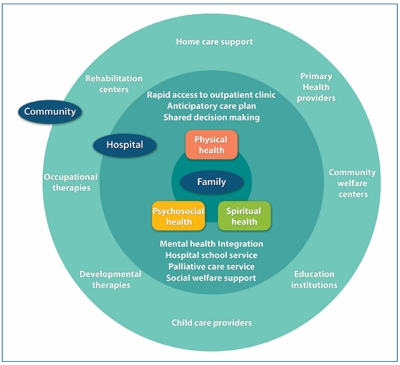
- Integrative care for children with medical complexity
- Jung Lee, Min Sun Kim, Hee Young Shin
- Clin Exp Pediatr. 2020;63(2):32-33. Published online November 14, 2019
-
- Systematic review and meta-analysis
- Genetics and Metabolism
- Global prevalence of classic phenylketonuria based on Neonatal Screening Program Data: systematic review and meta-analysis
- Hamid Reza Shoraka, Ali Akbar Haghdoost, Mohammad Reza Baneshi, Zohre Bagherinezhad, Farzaneh Zolala
- Clin Exp Pediatr. 2020;63(2):34-43. Published online February 6, 2020
-

Question: What is the global prevalence of classic phenylketonuria based on Neonatal Screening Program Data?
Finding: The overall worldwide prevalence of the disease is 6.002 per 100,000 neonates. The highest prevalence (38.13) was reported in Turkey, while the lowest (0.3) in Thailand.
Meaning: This difference in the prevalence may be due to differences in the number of consanguineous marriages among the different regions, phenylalanine cutoff points, and sample sizes.
- Editorials
- Pulmonology
- Are alternative antibiotics needed for antibiotic-nonresponsive Mycoplasma pneumoniae pneumonia?
- Eun-Ae Yang, Kyung-Yil Lee
- Clin Exp Pediatr. 2020;63(2):44-45. Published online February 15, 2020
-
- Gastroenterology
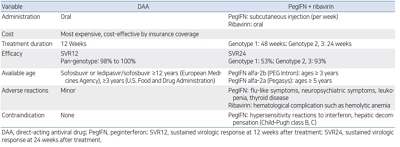
- Strategies for treating and managing chronic hepatitis C in children in the direct-acting antiviral era
- Suk-Jin Hong, Byung-Ho Choe
- Clin Exp Pediatr. 2020;63(2):46-47. Published online February 6, 2020
-
- Original Articles
- Neonatology (Perinatology)
- Placental histopathology in late preterm infants: clinical implications
- Kristina Ericksen, Joshua Fogel, Rita P. Verma
- Clin Exp Pediatr. 2020;63(2):48-51. Published online August 19, 2019
-
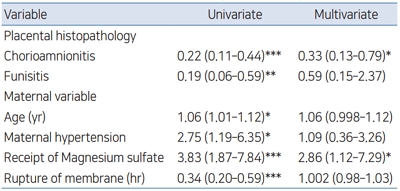
Question: Placental histopathology and its clinical implications in late preterm infants.
Finding: Placental vascular anomalies are more, and placental inflammation less common in late preterm infants compared to term. Higher maternal age, magnesium sulfate therapy and hypertension are clinical risk factors associated with late preterm delivery.
Meaning: Prevention and aggressive management of hypertension, and conception before 30 years of age might be effective in preventing late preterm births.
- Gastroenterology
- Thyroid disturbances in children treated with combined pegylated interferon-alpha and ribavirin for chronic hepatitis C
- Yasser K. Rashed, Fatma A. Khalaf, Sobhy E. Kotb
- Clin Exp Pediatr. 2020;63(2):52-55. Published online September 27, 2019
-
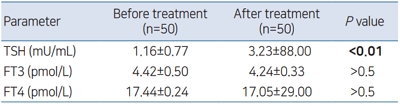
Background: Immunomodulatory properties of interferon (IFN) have been documented. It may induce autoimmune diseases such as autoimmune thyroiditis with hypo- or hyperthyroidism. In addition, it may impair thyroid hormone synthesis through affecting iodide organification in thyroid gland.
Purpose: The aim of this study was to describe thyroid function tests disturbances in children with chronic hepatitis C (CHC) receiving pegylated interferon-alpha (PEG...
- Neonatology (Perinatology)
- Effect of red blood cell transfusion on short-term outcomes in very low birth weight infants
- Eui Young Lee, Sung Shin Kim, Ga Young Park, Sun Hyang Lee
- Clin Exp Pediatr. 2020;63(2):56-62. Published online February 6, 2020
-
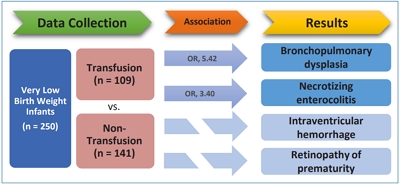
Question: Does RBC transfusion affect the short-term outcomes of VLBW infants?
Finding: The results showed that RBC transfusion was significantly related to the incidence of BPD (OR, 5.42; P<0.001) and NEC (OR, 3.40; P=0.009).
Meaning: Careful consideration of the patient’s clinical condition and appropriate guidelines is required before administering RBC transfusions.
- Letter to the Editor
- Neonatology (Perinatology)
- Risk factors for BiPAP failure as an initial management approach in moderate to late preterm infants with respiratory distress
- Heekwon Son, Eui Kyung Choi, Kyu Hee Park, Jeong Hee Shin, Byung Min Choi
- Clin Exp Pediatr. 2020;63(2):63-65. Published online February 15, 2020
-

Question: Which factors can predict BiPAP failure as the initial management approach for moderate to late preterm infants with respiratory distress?
Finding: RDS aggravation and increased oxygen and frequency requirements during BiPAP support were associated with BiPAP failure.
Meaning: Early changes to invasive ventilator care should be considered for moderate to late preterm infants showing RDS aggravation and increased oxygen and frequency requirements during BiPAP support.