Pneumonia is among the leading causes of death among younger children worldwide [1] and the major cause of death among the general population of Korea [2]. Recent Korean statistics indicate that pneumonia and respiratory diseases are no longer leading causes of death among children [2]. This may be due to improvements in hygiene, successful vaccination programs, and pediatrician effort and dedication.
Selecting appropriate chemotherapeutic agents for the pathogen and providing good conservative care are fundamental to pneumonia management. Nevertheless, for patients with community-acquired pneumonia (CAP), especially those who are not hospitalized, empirical treatment without identifying the causative microorganism is favored. As most affected patients are immunocompetent, this method is generally effective. Indeed, since 2015, the Korea Centers for Disease Control and Prevention has provided surveillance data on respiratory infection pathogens to aid the timely control of infections [3].
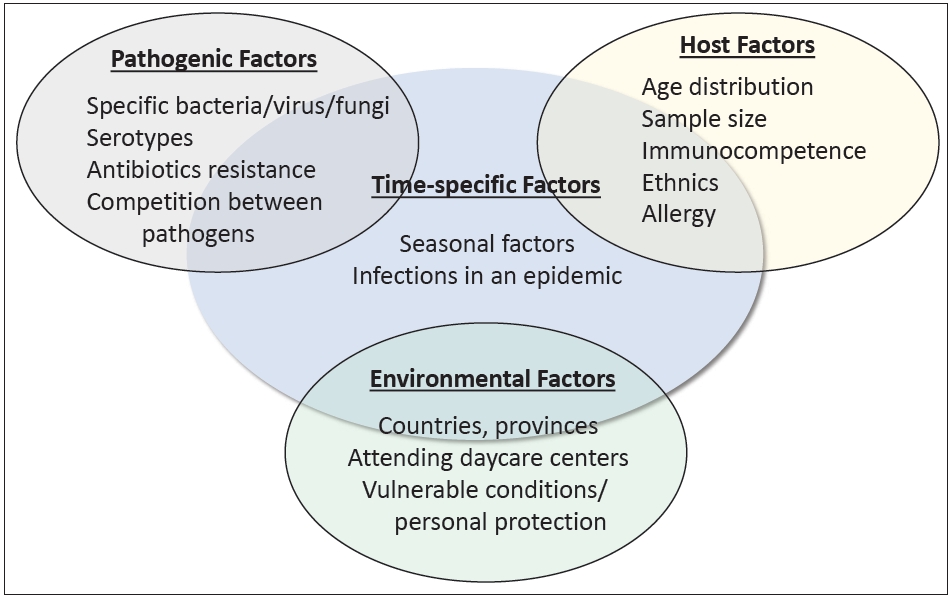
Although choosing treatments based on previously archived information is simple and intuitive, several factors must be considered before applying this knowledge to a particular circumstance (Fig. 1). This is comparable to the so-called distributional shift, an algorithm trained with artificial intelligence that, while accurate and efficient in the same setting in which it was trained, produces startlingly inaccurate results when directly applied to clinical practice outside the training environment [4]. In this context, although epidemiological information about pathogens is important, it is important to understand how the information was collected.
The review introduced in this issue organized by Roh et al. [5] provides essential information for determining the appropriate treatment strategies for CAP. The authors published an original study of respiratory samples and clinical data regarding the characteristics of patients with CAP and causative pathogens among Korean children [6]. Since it included as many as 1,023 children who met the CAP criteria from 27 secondary and tertiary medical institutions spread across 6 metropolitan areas, it should be considered to provide more relevant Korean data than any other previous report. On the other hand, it also provides a comprehensive summary of all available reports on pneumonia in Korean children [5]. In particular, the summary presented in Table 2 has great value because it describes common pathogen profiles and additional data such as age, region, collection period, and target group. Physicians exploring the optimal empirical treatment for their patients are likely to refer to these data as a guide.
Furthermore, this review is outstanding because the authors investigated situational factors that require consideration when interpreting epidemiological data. A good example is the serotypes and names of prevalent bacteria as well as their alterations according to the implementation of the Korean national immunization program. The article also clarifies several limitations that readers may encounter when analyzing archived data. For instance, no one can guarantee that an identified pathogen is a causal agent of CAP and not a mere bystander. Similarly, bacterial pneumonia cannot be excluded simply because no microorganisms grow in the culture medium. Recent studies utilizing gene sequencing to identify bacterial pathogens confirmed the latter hypothesis [7].
Finally, other factors should be considered. Etiologies that are currently epidemics are particularly important. For a specific virus, such as the pandemic influenza A (H1N1) virus in 2010 [8] or SARS-CoV-2 in 2022 [9], CAP cases caused by other viruses will inevitably decrease proportionally. Furthermore, mycoplasma epidemics occur every 3 to 4 years [10] that complicate statistics when we CAP a seasonal disease.
In conclusion, the epidemiological data of CAP have become complex to interpret. Significant changes have occurred over the past 2 years that require the division of cases into 2 categories: pre-coronavirus disease (pre-COVID-19) and post-COVID-19. Accordingly, we must reexamine how we would interpret pre-pandemic data and seek reasonable ways to apply this knowledge to postpandemic CAP cases. Additional research is required to reflect the postpandemic effects of social isolation, personal hygiene, and health improvement on the management of children with CAP.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


