Article Contents
| Clin Exp Pediatr > Volume 58(9); 2015 |
|
Abstract
Purpose
In addition to regulating calcium and phosphorus homeostasis and bone metabolism, vitamin D is known as an immune modulator. Recently, there has been increased worldwide interest in the association between low levels of vitamin D and allergic diseases. The purpose of this study was to assess the relationship between serum vitamin D levels and allergic/vasomotor rhinitis (AR/VR) in children.
Methods
This study included 164 patients. The sample included 59 patients with AR, 42 patients with VR, and 63 controls. Their ages ranged from 0 to 16 years. We examined the levels of 25-hydroxyvitamin D, Immunoglobulin E, specific IgE, and eosinophil cationic protein; peripheral blood eosinophil count; and the results of a skin prick test.
Results
Serum 25-hydroxyvitamin D levels were 19.0±8.5 ng/mL in the AR group, 25.5±10.9 ng/mL in the VR group, and 26.9±10.7 ng/mL in the control group. After adjustment for body mass index and season at the time of blood sampling, vitamin D levels in the AR group were lower than those of the VR group (P=0.003) and control group (P<0.001). Vitamin D levels were inversely correlated with Immunoglobulin E levels (r=-0.317, P<0.001). AR patients with food allergy or atopic dermatitis did not have lower levels of 25-hydroxyvitamin D than AR patients without these diseases.
In recent years, the prevalence of allergic diseases has continued to rise. Allergic rhinitis (AR) is one of the most common allergic conditions. Although, AR is not a life-threatening condition, it affects the quality of life, academic achievement, and work performance. Also, it imposes a substantial economic burden on the society1).
In addition to the role of vitamin D in calcium homeostasis and bone mineralization, many published reports suggest the role of vitamin D as an immune modulator2). Since the last five decades, medical experts have investigated the relationship between vitamin D deficiency and occurrence of allergic disease, but the studies have shown inconsistent results. Therefore, the current study aimed to assess the relation between serum vitamin D level and AR in Korean children.
This study included 164 patients (106 males and 58 females) who were visiting the outpatient Department of Pediatrics in the Kyungpook National University Children's Hospital from March 2013 to May 2014. The subjects included 59 AR patients, 42 vasomotor rhinitis (VR) patients, and 63 controls.
Diagnosis of AR was made according to the Allergic Rhinitis and its Impact on Asthma 2008 criteria3). AR patients reported one or more typical symptoms of chronic rhinitis (rhinorrhea, nasal obstruction, sneezing, and nasal itching), and showed positive result to at least one aeroallergen in the multiple allergen simultaneous test, or uniCAP or allergy skin test. VR patients were defined as those who reported typical symptoms of chronic rhinitis, and had negative allergy tests for aeroallergens. Control group were composed of subjects who did blood tests including serum 25-hydroxyvitamin D level in outpatient department and did not show chronic rhinitis symptoms and history. Patients with asthma and acute infectious disease were excluded in all groups.
We measured patients' height and weight, and calculated body mass index (BMI). Blood sampling date was also classified into season.
Blood samples were collected and serum levels of 25-hydroxy-vitamin D were assessed using Vitamin D Total Assay (Roche Diagnostics, Basel, Switzerland). Peripheral blood total eosinophil counts (TEC) were checked by using an automated system. Eosinophil cationic protein (ECP) and Immunoglobulin E (CAP system, Pharmacia-Upjohn, Uppsala, Sweden) were measured in accordance with the manufacturer's instructions.
The multiple allergen simultaneous test (AdvanSureAlloscan, LG Life Sciences, Daejeon, Korea) was performed in 83 subjects. The inhalant panel contains 41 kinds of allergens, and results were interpreted as class 0-6. Class ≥2 was interpreted as positive.
Specific IgE testing for Dermatophagoides farina, Dermatophagoides pteronyssinus, cat epithelia, dog epithelia, Alternaria, and Aspergillus was performed in 52 patients using UniCAP (Pharmacia, Uppsala, Sweden). A specific IgE level >0.35 IU/mL was considered as positive. Allergy skin test for 17 common allergens (Der f, Der p, Acarussiro, Tyrophagus putrescentiae, cat epithelia, dog epithelia, Alternaria, Aspergillus, birch, alder, hazel, pine, bermuda, timothy, orchard, ragweed, and mugwort) was performed in 57 subjects. Saline and 0.5% histamine HCl were used as a negative and positive control, respectively. After 15 minutes, wheal diameter greater than 3 mm was considered positive.
Analysis of variance was used for comparing the AR, VR, and control groups and an adjusted analysis of covariance was used for BMI adjustment. Pearson correlation test was used for assessing the relationship between variables. A P value <0.05 was considered statistically significant. All data were analysed with PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
Of the 164 patients, 106 (65%) were males and 58 (35%) were females. The age of subjects ranged from 0 to 16 years (mean age, 5.9±3.8 years). Mean serum 25-hydroxyvitamin D level was 19.0±8.5 ng/mL in the AR group, 25.5±10.9 ng/mL in the VR group, and 26.9±10.7 ng/mL in the control group. Immunoglobulin E level was 466.2±609.9 IU/mL in the AR group, 63.3±86.3 IU/mL in the VR group, and 158.2±330.6 IU/mL in the control group (Table 1).
After adjustment for BMI and season at blood sampling, the AR group showed lower serum 25-hydroxyvitamin D level (19.0±8.5 ng/mL) than the VR group (25.5±10.9 ng/mL, P=0.003) and the control group (26.9±10.7 ng/mL, P<0.001) (Fig. 1).
The 25-hydroxyvitamin D level had a negative correlation with Immunoglobulin E level in total subjects (r=-0.317, P<0.001) (Fig. 2). ECP, TEC, number of sensitized allergens, and specific IgE levels to Der. f and Der. p did not show any correlation with the 25-hydroxyvitamin D level (data not shown).
In our study, AR patients showed lower serum vitamin D levels than VR patients and controls. Jung et al.4) reported that there was potential relation between vitamin D deficiency and AR prevalence in Korean adults. A study performed in 2012 reported that vitamin D deficiency occurs more often in AR patients than in the normal population5). A cohort study reported by Mai et al.6) in Norwegian adults showed that lower vitamin D levels were related to increased prevalence of AR among men. They also showed that lower vitamin D levels were related with reduction in the prevalence of AR in premenopausal women. However in our study, there was no difference in the serum vitamin D level and incidence of AR between male and female. That is because may be subjects on our study are mostly comprised of preadolescent age.
In contrast, some studies reported that a high vitamin D level is a risk factor for occurrence of allergic diseases. A prospective study showed that excessive vitamin D intake during infancy was significantly related to atopic signs, like atopic dermatitis, allergy rhinitis, or asthma, up to six years of age7). Other studies have proposed that both high and low 25-hydroxyvitamin D levels were associated with morbidity and mortality of thedisease8,9). However, it is still not confirmed that a U-shaped relationship existed between overdose and under-dose of vitamin D.
Vitamin D modulates innate immunity and adaptive immunity2,10). Most of the cells belonging to the innate immune system, such as macrophages and dendritic cells (DCs), have receptors for vitamin D. In macrophages and DCs of the innate immune system, 25-hydroxyvitamin D undergoes hydroxylation by CYP27B1. The active form of vitamin D, 1,25-hydroxyvitamin D, induces inhibition of DC maturation and suppression of antigen presentation. Also, activated vitamin D modulates helper T-cell action.
Vitamin D interferes with T-cell proliferation by suppressing Th1 cytokine secretion. The effect of vitamin D on Th2 cells is still under debate. However, there is one study which demonstrates that vitamin D leads to an increase in interleukin (IL)-10 expression and a decrease in IL-2 expression followed by hypoergia in regulatory T cells, which is associated with a harmful immune response11,12,13). Also, vitamin D decreases IL-12 production; thus it can reduce the differentiation of Th1 cells and increase the differentiation Th2 cells, which are responsible for allergic reactions. Vitamin D also modulates the secretion of IgE by interrupting the proliferation of B-lymphocytes14,15,16).
Human being can obtain vitamin D by consuming fish, cod liver oil, egg yolk, and fortified foods, and exposing their skin to sunlight. Through a series of processes, the active form of vitamin D is biosynthesized10). There are many variables that can affect the vitamin D level. Important factors are outdoor physical activities, intake of calcium and fortified foods, and applying sunscreen. Reduction in the exposure to sunlight can induce low vitamin D levels. Therefore, it can be difficult to identify the causal relationship between vitamin D level and development of disease. Also, because vitamin D is a group of fat-soluble vitamins and is stored in the adipose tissue10). Therefore, BMI can affect as a concerned factor for vitamin D deficiency10). Nevertheless, after adjustment for BMI and season at blood sampling, the difference in the serum 25-hydroxyvitamin D level was still statistically significant.
In this study, mean age for groups were not concordant. However, reference range of 25-hydroxyvitamin D is not differ by age17) and some studies that reported different vitamin D levels by age also showed conflict data. Mansbach et al.18) reported children ages 6-11 years had lower levels of 25-hydroxyvitamin D compared to children ages 1-5 years. Flores et al.19) reported 25-hydroxyvitamin D were lower in preschool children than in school-aged children. Therefore, it's hard to say definite relationship between age and vitamin D.
This study showed a reverse relationship between Immunoglobulin E and serum vitamin D levels in all of the patients. A study on asthma demonstrated that the serum IgE level and the serum 25-hydroxyvitamin D level are negatively correlated in children, but not in adults20). Hartmann et al.21) indicated that targeting the vitamin D receptor (VDR) hinders the B cell-dependent allergic immune reaction. In VDR knockout mice, the serum IgE levels are elevated. In vitro, 1, 25-dihydroxyvitamin D, as a natural VDR agonist, directly interferes with the IgE production of educated B-lymphocytes.
In conclusion, the effect of vitamin D on allergic diseases remains in conclusive despite performing many systematic studies. The present study suggests a possible correlation between vitamin D deficiency and AR in Korean children. Further studies are required to confirm the relationship between AR and vitamin D level, and to explore the underlying mechanisms.
Conflicts of interest
Conflicts of interest:
No potential conflict of interest relevant to this article was reported.
References
1. Meltzer EO. The prevalence and medical and economic impact of allergic rhinitis in the United States. J Allergy Clin Immunol 1997;99(6 Pt 2): S805–S828.

2. Christakos S, Hewison M, Gardner DG, Wagner CL, Sergeev IN, Rutten E, et al. Vitamin D: beyond bone. Ann N Y Acad Sci 2013;1287:45–58.



3. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 2008;63(Suppl 86): 8–160.


4. Jung JW, Kim JY, Cho SH, Choi BW, Min KU, Kang HR. Allergic rhinitis and serum 25-hydroxyvitamin D level in Korean adults. Ann Allergy Asthma Immunol 2013;111:352–357.


5. Arshi S, Ghalehbaghi B, Kamrava SK, Aminlou M. Vitamin D serum levels in allergic rhinitis: any difference from normal population? Asia Pac Allergy 2012;2:45–48.



6. Mai XM, Chen Y, Camargo CA Jr, Langhammer A. Serum 25-hydroxyvitamin D levels and self-reported allergic rhinitis in Norwegian adults: The HUNT Study. Allergy 2014;69:488–493.


7. Back O, Blomquist HK, Hernell O, Stenberg B. Does vitamin D intake during infancy promote the development of atopic allergy? Acta Derm Venereol 2009;89:28–32.


8. Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med 2008;168:1629–1637.



9. Heaney RP. Vitamin D: how much do we need, and how much is too much? Osteoporos Int 2000;11:553–555.


10. Vlaykov A, Vicheva D, Stoyanov V. The role of vitamin D in the pathogenesis of allergic rhinitis and atopy. Turk Arch Otolaryngol 2013;51:63–66.

11. Searing DA, Leung DY. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am 2010;30:397–409.



12. Hewison M, Freeman L, Hughes SV, Evans KN, Bland R, Eliopoulos AG, et al. Differential regulation of vitamin D receptor and its ligand in human monocyte-derived dendritic cells. J Immunol 2003;170:5382–5390.


13. Gorman S, Kuritzky LA, Judge MA, Dixon KM, McGlade JP, Mason RS, et al. Topically applied 1,25-dihydroxyvitamin D3 enhances the suppressive activity of CD4+CD25+ cells in the draining lymph nodes. J Immunol 2007;179:6273–6283.


14. Mahon BD, Wittke A, Weaver V, Cantorna MT. The targets of vitamin D depend on the differentiation and activation status of CD4 positive T cells. J Cell Biochem 2003;89:922–932.


15. Reinholz M, Ruzicka T, Schauber J. Vitamin D and its role in allergic disease. Clin Exp Allergy 2012;42:817–826.


16. Cheng HM, Kim S, Park GH, Chang SE, Bang S, Won CH, et al. Low vitamin D levels are associated with atopic dermatitis, but not allergic rhinitis, asthma, or IgE sensitization, in the adult Korean population. J Allergy Clin Immunol 2014;133:1048–1055.


17. Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Drug and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics 2008;122:398–417.


18. Mansbach JM, Ginde AA, Camargo CA Jr. Serum 25-hydroxyvitamin D levels among US children aged 1 to 11 years: do children need more vitamin D? Pediatrics 2009;124:1404–1410.



19. Flores M, Macias N, Lozada A, Sanchez LM, Diaz E, Barquera S. Serum 25-hydroxyvitamin D levels among Mexican children ages 2 y to 12 y: a national survey. Nutrition 2013;29:802–804.


Fig. 1
Comparison of vitamin D levels between the allergic rhinitis (AR), vasomotor rhinitis (VR), and control groups. The vitamin D level in the AR group was significantly lower than that in the VR group (P=0.003) and control group (P<0.001) after adjustment for body mass index and season at the time of blood sampling.
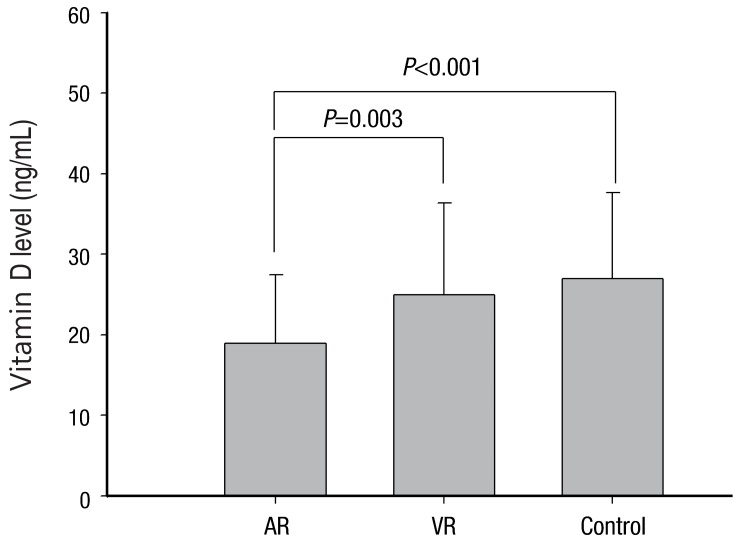
Fig. 2
Correlation between serum IgE and vitamin D levels. Vitamin D level was negatively correlated with IgE levels (r=-0.317, P<0.001).
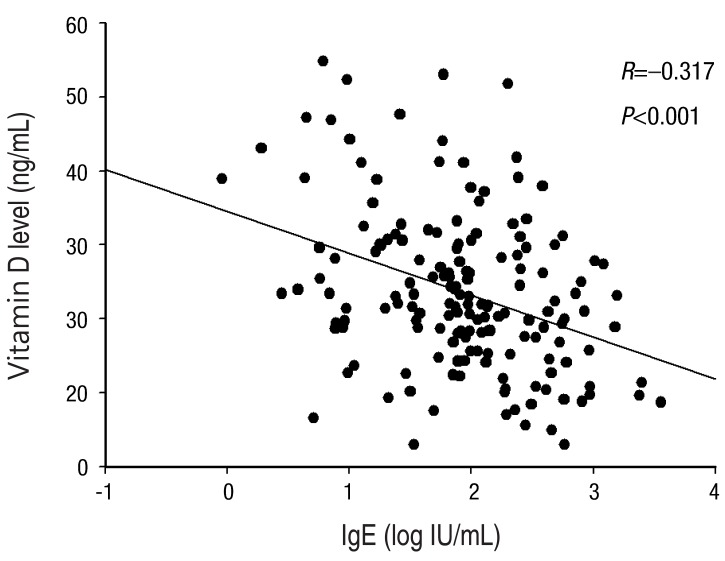
Table 1
Demographics compared between allergic rhinitis, vasomotor rhinitis, and control subjects
Values are presented as mean±standard deviation unless otherwise indicated.
AR, allergic rhinitis; VR, vasomotor rhinitis; ECP, eosinophil cationic protein; TEC, peripheral blood total eosinophil count; BMI, body mass index; NS, nonspecific.
*Comparison between AR and VR groups. †Comparison between AR and control groups.



 PDF Links
PDF Links PubReader
PubReader PubMed
PubMed Download Citation
Download Citation


