Article Contents
| Clin Exp Pediatr > Volume 67(4); 2024 |
|
Abstract
Background
Findings are conflicting regarding the effect of zinc supplementation on disease severity in children with acute gastroenteritis.
Purpose
To examine the effects of probiotics and zinc on the clinical outcomes of infants and children with acute infectious diarrhea.
Methods
In this randomized controlled trial, children with mild or moderate to severe acute gastroenteritis in the Kurdistan Region from November 2021 to June 2022 were diagnosed clinically and randomly assigned to the experimental or control group. The experimental group (n=50) received probiotics and zinc, whereas the control group (n=51) received probiotics alone for 1 week. The product contained live Bifidobacterium infantis, Lactobacillus paracasei, and Lactobacillus rhamnosus (10×106 colony-forming units/day for 7 days). Zinc syrup was administered to the probiotic plus zinc group. Each 5 mL of syrup contained 15 mg of zinc sulfate. Dehydration and disease severity in both groups were measured using the Clinical Dehydration Scale and the Modified Vesikari Scale, respectively. An illness episode was defined as an episode of gastroenteritis with a total score of ≥9 on the Modified Vesikari Scale (range, 0–20).
Results
The probiotic and probiotic plus zinc groups were similar in age (1.79 years vs. 1.69 years, respectively; P= 0.645), sex (male/female ratio: 1.43 and 1.0, respectively; P=0.373), and medical characteristics. The groups had similar mean dehydration and disease severity scores and a similar incidence of dehydration recovery (some dehydration, 3.92% and 4.00%, respectively; P=1.000), and recovery from mild gastroenteritis (0.0% and 2.0%, respectively; P=0.495) at 2 weeks. Significant decreases in mean dehydration severity and disease severity score (1.80 to 0 and 6.66 to 0, respectively; P<0.001) and the development of dehydration (some dehydration, from 94.0% to 4.0%; P<0.001) from baseline to 2 weeks were noted in the probiotics plus zinc group. The probiotics group responded similarly. The development of mild gastroenteritis was significantly reduced from baseline to 2 weeks (90.2% to 0% and 78.0% to 2.0% in the probiotics and probiotics plus zinc groups, respectively; P<0.0001). The probiotics plus zinc group had a shorter mean recovery time (1.34 days vs. 2.00 days, respectively; P<0.001).
Acute gastroenteritis is a condition where the gastrointestinal tract becomes infected, often by a virus. It typically results in symptoms such as diarrhea, vomiting, nausea, fever, and abdominal pain, which come on quickly. The severity and duration of symptoms can vary depending on the cause of the infection and the individual's health. While most cases of acute gastroenteritis resolve on their own within a few days to a week, some cases may require medical attention, especially in certain populations [1]. The signs and symptoms of gastroenteritis among children can be nonspecific [2]. Diarrhea is defined as the frequent episodes of unformed liquid stools [3]. Acute gastroenteritis is a leading responsible factor of mortality among children under 5 years old. Acute gastroenteritis is a main cause of morbidity in deprived areas worldwide [4]. Also, acute gastroenteritis is responsible for a high incidence rate of hospitalization and it is related to the economic burden on healthcare systems [5].
The main approach for managing acute gastroenteritis involves ensuring that individuals consume enough fluids to prevent dehydration. This is especially important because symptoms such as diarrhea and vomiting can cause significant fluid loss. In addition to this, the World Health Organization (WHO) has recommended the use of oral zinc as a treatment for acute gastroenteritis. Zinc is a micronutrient that is important for the immune system and can help reduce the duration and severity of diarrhea. The WHO suggests that children with acute gastroenteritis be given oral zinc for 10 to 14 days, while also continuing to receive fluids and nourishment [6,7] and the United Nations Children's Fund. A systematic review included 33 studies that included 10,841 children aged 1 month to 5 years with acute or persistent diarrhea, including dysentery. They included clinical studies that examined oral zinc supplementation with a placebo. They reported that it is sufficient from well-performed randomized controlled trials (RCTs) for the effectiveness of zinc in reducing mortality and hospitalization rates among children with acute diarrhea. The zinc supplementation may shorten the average diarrhea duration by close to half a day in children aged older than 6 months (-11.46; 95% confidence interval [CI], -19.72 to -3.19 hours) and reduce the number of children with persistent diarrhea until day 7 (risk ratio [RR], 0.73; 95% CI, 0.61–0.88). The effect may be greater in patients with signs of malnutrition close to 1 day of diarrhea duration (26.39 hours; 95% CI, -36.54 to -16.23). However, these effects may not include children younger than 6 months in terms of diarrhea duration and some children with diarrhea. The zinc may shorten the diarrhea duration in patients with persistent diarrhea by 16 hours (95% CI, -25.43 to -6.24) [8].
The study analyzed data from 28 RCTs and found that zinc supplementation was associated with a significant decrease in the risk of all-cause mortality among children. Specifically, the study reported that zinc supplementation reduced the risk of all-cause mortality by 16%. This is an important finding, as it suggests that zinc supplementation may be an effective intervention for reducing mortality rates in children under 5. However, it's worth noting that more research may be needed to fully understand the mechanisms by which zinc supplementation exerts its protective effects and to determine the optimal dosages and durations of zinc supplementation in this population (standardized RR [SRR], 0.84; 95% CI, 0.74–0.96); including the risk of mortality by diarrhea by 15% (SRR, 0.85; 95% CI, 0.70–1.03) [9]. But this review did cover all causes-mortality among children under 5 years. In addition, these studies have not included children older than 6 years older. Zinc supplementation may be beneficial for treating acute gastroenteritis and diarrhea in malnourished children, particularly in developing countries [10].
Therefore, we need more robust and high-quality RCTs to further examine the effectiveness of zinc supplementation on acute gastroenteritis among children. Given controversial reports in the studies of the effectiveness of zinc supplementations on gastroenteritis, we aimed to examine the effectiveness of zinc supplementation on clinical outcomes in infants and children with acute infectious diarrhea. In this regard, we hypothesized that the patients who receive the Lactobacillus rhamnosus GG plus zinc will have less duration of diarrhea and vomiting compared to the patients who received the probiotic Lactobacillus rhamnosus GG only.
The children in the study were randomly assigned to either the experimental group (n=50) or the control group (n=51). The experimental group received a combination of probiotics and zinc syrup, along with rehydration therapy, for 7 days. This group was referred to as the "probiotics plus zinc" group. The control group received probiotics treatment and rehydration therapy but did not receive zinc syrup. This group was referred to as the "probiotics" group.
The patients in both study groups were followed-up for 2 weeks to document the frequency and duration of diarrhea and committing and possible adverse events. The healing duration of the patients in each group was recorded by the second author as well. The diagnosis of gastroenteritis was performed by the third author, a pediatrician with five years of experience in diagnosing and treating pediatric patients. The patients were followed up by the second author for documentation of the outcomes of both study groups. The patients were recruited from both Heevi Teaching Public Hospital and the private clinic of the third author in Duhok city in Kurdistan Region of Iraq. The patients were included in this study between November 2021 and June 2022.
The clinical diagnosis of acute gastroenteritis was established based on symptoms. Relevant details were gathered regarding recent contact with children experiencing similar symptoms, characteristics and frequency of stool and vomit, fluid consumption, urine output, travel history, and use of medications. In cases where children exhibited high fever, persistent symptoms, or indications of a potential surgical issue (such as intense abdominal pain, bilious vomiting, or the presence of an abdominal mass), doubts regarding the laboratory diagnosis prompted further investigations. These involved general stool analysis, stool culture, blood tests, imaging studies, and other relevant examinations [11].
A pre-generated random number was generated by the IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA). As a default, 100 patients were randomly assigned into 2 groups. The groups were randomly assigned either into the probiotic or the probiotic plus zinc group through a lottery technique. The clinician was trained on how to recruit the patients either in the probiotics or probiotics plus zinc study groups. The clinician of the study followed the pregenerated random list for the recruitment of the study. The randomization list was generated by the first author to avoid allocation bias.
The male and female outpatients’ children and infants who were diagnosed with mild or moderate-severe acute gastroenteritis were included in this study. These criteria were applied to all patients without any exceptions. In addition, the patients diagnosed with systemic diseases, hospitalized patients, and surgical causes, those who received antibiotics, probiotics or any other antidiarrheal in the previous 24 hours. were eligible for the exclusion criteria. Further, the patients with diarrhea for more than 48 hours, patients who have blood in their stool, and parents of patients not willing to participate were not included in the study.
The patients in the probiotics plus zinc group received live combined probiotics (10×106 CFU/day for 7 days). The product contained probiotic microorganism of Bifidobacterium infantis, Lactobacillus paracasei, and Lactobacillus rhamnosus. The zinc syrup was received by probiotics plus zinc group. Each 5 mL of syrup contained 15-mg zinc (as sulfate). The zinc was alcohol-free. The treatment was given to the patients in both study groups by the same physician, therefore, we would not expect the significant heterogeneity of medicines between groups. The control group received combined probiotics and the experimental group received the combined probiotics along with zinc supplementation.
The following outcomes were recorded as 2 weeks of the following by the second author; 1. frequency of diarrhea; 2. duration of diarrhea (time to 2 consecutive soft or formed stools or no stool for 12 consecutive hours); 3. duration of vomiting; 4. length of hospital stay; and 5. adverse events.
To avoid measurement and allocation bias, the randomization list was generated by the first author. The interventions of both study groups were implemented by the third author. But the documentation of the outcomes was performed by the second author. Also, to avoid allocation concealment, the clinician allowed the children to enter the clinic one by one. In this regard, 2 children in one family with gastroenteritis were not included in this study. Lastly, the statistical calculation was performed by the first author. The second author followed up with all children by 2 weeks.
The patients in both study groups were blind to each other since we followed the principles of allocation concealment. In this regard, the patients visited the doctor one by one to protect the allocation concealment. In addition, we had 2 patients in one family infected by gastroenteritis, but they were not included in this study. In addition, the patients were completely blind to the probiotics intervention. The Health Ethics Committee of this region permitted us to not tell anything about the probiotics because no risk has been reported in terms of the probiotic that we used for our patients. However, the parents of the children signed a written consent form for allowing us to follow up with their children.
The dehydration of the children in both study groups was measured by the Clinical Dehydration Scale (CDS). The CDS measures the general appearance, eye, mucous membrane, and tears. The characteristics of the children based on this scale are measured from 0 to 2 as follows. (a) General appearance (0: normal; thirsty, restless, lethargic, but irritable when touched); 2: drowsy, limp, cool or sweaty; comatose or not); (b) eye (0: normal; 1: slightly sunken; 2: very sunken); (c) mucous membranes (0: moist; 1: sticky; 2: dry), and (d) tears (0: tears; 1: decreased; 2: absent). In this scale, the scores are added together to obtain the total score of the dehydration. The scores are defined as no dehydration (zero), some dehydration (scores 1–4), and moderate-to-severe dehydration (scores 5–8) [12].
To assess the severity of gastroenteritis in the study participants, the researchers used a measurement tool called the Modified Vesikari Scale. This scale assigns a score to each participant based on several components, including the duration of diarrhea, the maximum number of watery stools per day, the duration and frequency of vomiting, the maximum recorded temporal temperature, whether the patient required an unscheduled healthcare visit, and the treatment received. Each component is rated on a scale from 0 to 3 points, with higher scores indicating more severe symptoms.
In this study, an illness episode was defined as an episode of gastroenteritis with a total score of 9 or higher on the Modified Vesikari Scale, which ranges from 0 to 20. The Vesikari Scale is a validated tool used to assess the severity of gastroenteritis among pediatric patients. By using this scale, the researchers were able to quantify the severity of gastroenteritis symptoms and compare them between the experimental and control groups. Further details about the components of the Modified Vesikari Scale can be found in the main reference of the study [13].
No adverse events were reported by the children in both probiotics and probiotics with zinc who were included in this study.
The study utilized various statistical tests to analyze the data. The general characteristics of the probiotics and probiotics plus zinc groups were presented in mean and standard deviation or number and percentage.The homogeneity between the groups was assessed using an independent t test or a Pearson chi-square test. The differences in dehydration and disease severity between the 2 groups at baseline and after 2 weeks were analyzed using independent t tests or Pearson chi-square tests. The differences in dehydration characteristics and disease severity components between the groups at 2 weeks and before and after treatment within each group were analyzed using Fisher exact test, paired t tests, and McNemar tests. Other outcome comparisons were assessed using independent t tests or Pearson chi-square tests. The incidence of outcomes and watery episodes was reported in numbers and percentages. The RR and 95% CI were used to determine the effectiveness of one intervention over another, and a P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using JMP Pro 14.3.0 software (https://www.jmp.com/en_us/home.html).
The study obtained scientific and ethical approval from the College of Nursing at the University of Duhok and the local Health Ethics Committee of the Duhok General Directorate of Health, respectively. Written consent forms were obtained from the parents of the children in accordance with the Modified Declaration of Helsinki, and patient confidentiality was protected. The probiotics used in the study, Lactobacillus rhamnosus GG, were reported to have no adverse events based on the literature, and their administration was approved by the Health Ethics Committee. The study protocol was registered with a reference number of 15092021-9-2 on September 15th, 2021.
The children of probiotics and probiotics plus zinc were similar in age (1.79 years vs. 1.69 years, P=0.645), sex (P=0.373), comorbidity (P=0.118), treatment for acute gastroenteritis (P=0.513), maximum recorded temperature (P=0.067), receipt of antibiotics in previous 14 days (P=0.7409), and duration of symptoms before 48-hour visit (51.71 vs. 38.60, P=0.5724) (Table 1).
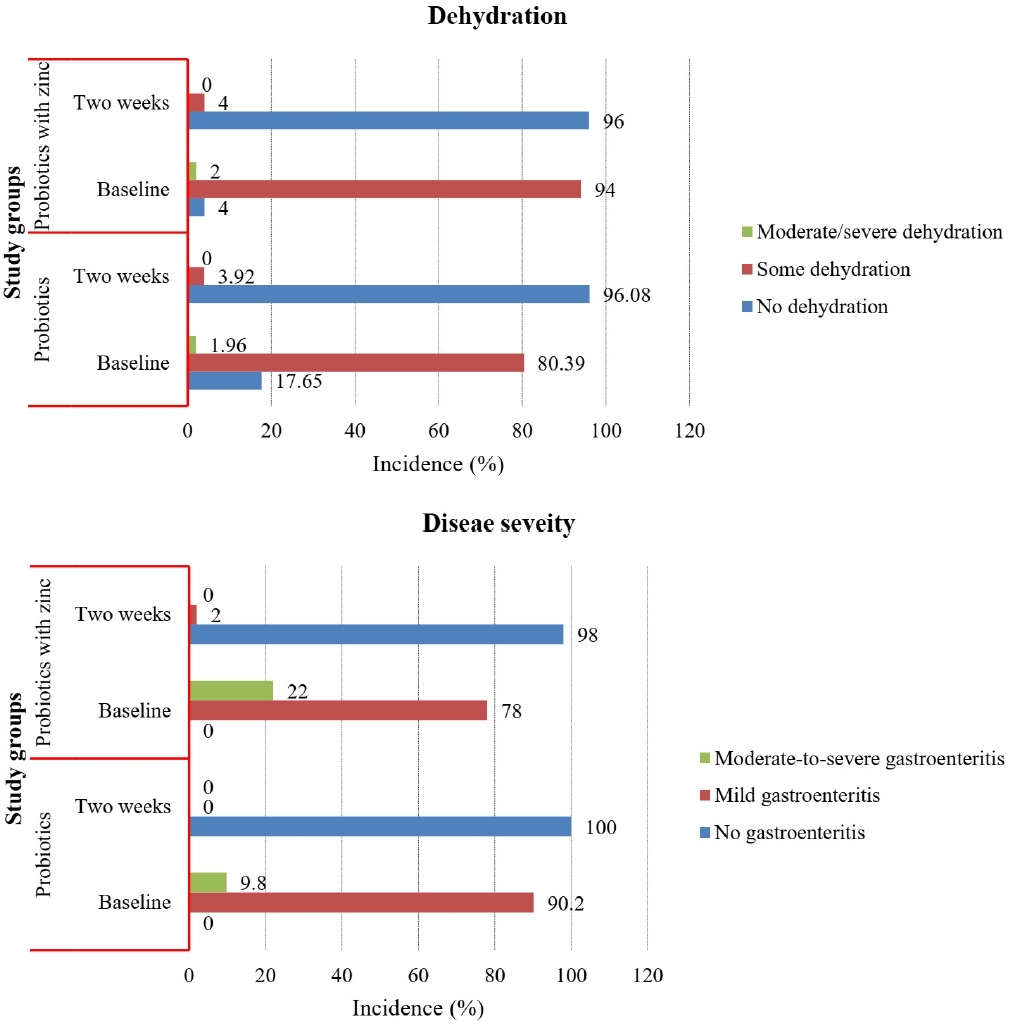
The children of probiotics and probiotics plus zinc were similar in dehydration score (1.53 vs. 1.80, P=0.131) and disease severity (6.12 vs. 6.66, P=0.216). In addition, the children of probiotics and probiotics plus zinc were similar in the prevalence of dehydration (some dehydration of 80.39% and 94.00%; P=0.088) and the prevalence of disease severity (mild gastroenteritis of 90.20% and 78.00%; P=0.109) at baseline, respectively. The children of probiotics and probiotics plus zinc were the same in the mean value of dehydration score and disease severity (zero in both study groups) at 2 weeks.In addition,the incidence of dehydration recovery was similar in probiotics and probiotics plus zinc was similar (some dehydration of 3.92% and 4.00%, P=1.000), and the incidence of gastroenteritis recovery (mild gastroenteritis of 0.0% and 2.0%, P=0.495) at 2 weeks, respectively (Table 2).
The study showed that the children of probiotics and probiotics plus zinc were similar in general appearance (P=1.000), eyes (P=0.618), mucous membranes (P=1.000), and tears (P=0.495). In addition, the patients of both study groups were similar in the duration of diarrhea (P=0.495), maximum number of watery stools per 24 hours (P=0.495), duration of vomiting (hour) (P=0.495), maximum number of vomiting episodes per 24 hours (P=0.495), and maximum recorded rectal temperature (°C) (P=0.495) at 2 weeks. Also, they were the same at unscheduled health care visits and treatment at 2 weeks (Table 3).
The study showed that mean dehydration severity and disease severity significantly decreased from baseline to 2 weeks among probiotics children (from 1.53 to 0 and from 6.12 to 0, P<0.001), respectively.In addition, the incidence of dehydration was significantly decreased in probiotics from baseline to 2 weeks (some dehydration, 80.39%–3.92%, P<0.001). The incidence of gastroenteritis was significantly reduced from baseline to 2 weeks (mild gastroenteritis, 90.20%–0.00%; P<0.001). A similar pattern was found among probiotics plus zinc group. The dehydration and disease severity decreased from baseline to 2 weeks (from 1.0 to 0 and from 6.66 to 0, P<0.001), respectively. Also, the incidence of dehydration was significantly decreased from baseline to 2 weeks in probiotics plus zinc children ([incidence of some dehydration, 94.00%–4.00%; P<0.001] and [incidence of mild gastroenteritis, 78.00%–2.00%; P<0.001]) (Table 4, Fig. 1).
The study showed that both probiotics and probiotics plus zinc were similar in the receiving the incidence of intravenous fluids (1.96% vs.0%, P=1.000), hospital admission (1.96% vs. 0%, P=1.000), and repetition of Emergency Department visit (0% vs. 2.00%, P=0.495). But the children in the probiotics plus zinc group had significantly shorter healing duration compared to the children in the probiotics group, 1.34 versus 2.00 days (P<0.001). The study showed that 88.00% of the children recovered from the disease within 1–2 days in the probiotics with zinc compared to 70.59% in the probiotics children (P=0.031) (Table 5).
This study showed that taking probiotics with zinc in children diagnosed with gastroenteritis has no effect on dehydration and disease severity and dehydration recovery and disease severity compared to children who received probiotics only at 2 weeks. But, the children who received the probiotics with zinc recovered from gastroenteritis in a shorter time compared to the children who received probiotics only. There is limited information on the effectiveness of receiving probiotics plus zinc on clinical outcomes in children with diarrhea. One of these trials investigated the impact of probiotics and zinc supplementation on the duration and frequency of acute diarrhea in children aged 6 months to 2 years. The participants were split into 3 groups, including a group receiving zinc supplements, a group receiving probiotics, and a control group receiving only supportive care. The study found that all children in the probiotic group experienced diarrhea until the third day of admission, while 76.1% of children in the zinc group still had diarrhea at that point (RR, 1.31). Furthermore, the incidence of diarrhea was 80% in the probiotic group until the fourth day of admission, while it was significantly lower at 47.8% in the zinc group (RR, 36.4 times). The incidence of complications was also lower in the zinc group compared to the probiotic group [14].
Another double-blind RCT examined the effect of zinc and probiotic supplementation on reducing the frequency and duration of acute diarrhea in children under 5 years. The study reported that significant effects of zinc and probiotics supplementation on a decrease in the frequency and duration of acute diarrhea under 5 years compared to the patients who received only probiotics or placebo at 1 week. They reported that the mean frequency of acute diarrhea in children under 5 before treatment was 4.94 times/day, and after the supplementation was 0.62 times/day (standard deviation [SD], 1.14; 95% CI, 0.24–1.02). The mean duration of acute diarrhea before supplementation was 1.28 days (30.85 hours) and after supplementation changed to 1.51 days (36.34 hours).
Other trial shave focused the effects of zinc supplementation compared to the placebo in children and infants. The effectiveness of zinc on clinical outcomes in children with acute diarrhea has been examined versus placebo in the literature. The updated systematic review included 33 RCTs [8] reported that the mean duration of diarrhea among children who received zinc was close to 13 hours shorter than those children who received placebo (mean difference [MD], -13.42; 95% CI, -20.52 to -6.31). But there was substantial statistical heterogeneity between studies. The benefit was for the children aged over 6 months of age (MD,-11.46hours; 95% CI,-19.72 to -3.19 hours) and those who included all age groups (MD, -22.18 hours; 95% CI, -32.57 to -11.78 hours). No effect was found among trials that included children aged less than 6 months of age. In addition, the treatment with zinc supplementation led to fewer children with persistent diarrhea at day 3 (RR, 0.77; 95% CI, 0.69–0.86), at day 5 (RR, 0.76; 95% CI, 0.64–0.91), and at day 7 (RR, 0.82; 95% CI, 0.72–0.94). There was a similar pattern at day 7 as well. But there was a statistically significant difference in heterogeneity between clinical trials. In the study, in terms of duration of diarrhea, the average of the effect was 24.76 (95% CI, 15.9–33.6 hours), diarrhea lasting ≥4 days (95% CI, 0.41–0.32), and stool frequency on day 2 was 0.80 (95% CI, 0.45–1.14). In terms of stool frequency, the review did not report a significant benefit of zinc supplementation on decreasing stool frequency (RR, -0.10; 95% CI, -0.25 to 0.04). There were no consistent results on the effect of zinc supplementation on stool output, while its effect on hospitalization and mortality rate was positive among children [8]. However, there is very low certainty evidence of the effectiveness of zinc supplementation on a number of deaths and hospitalization during acute diarrhea from well-performed clinical trials. These effects may depend on the local risk of zinc deficiency and population characteristics such as malnutrition degree and breastfeeding habits [8].
Zinc is an essential micronutrient in human nutrition and plays a critical role in cellular functions such as protein synthesis, cell growth, and differentiation [15]. The exact mechanism by which zinc treats diarrhea is not completely understood. However, it is suggested that zinc may play a role in various intestinal functions, including the regulation of intestinal fluid transport and mucosal integrity, as well as the modulation of genes that encode important zinc-dependent enzymes like cytokines. These enzymes are involved in the immune system and the regulation of oxidative stress [15,16]. The effects of using a combination of probiotics with zinc on early recover in children with acute diarrhea has been reported by another RCT within 5 days after receiving the therapy compared to the probiotics alone group. The duration of diarrhea in the combination group was 27.63 (SD, 14.22 hours) compared to 38.86 (SD, 20.70 hours) in the probiotics only group [17].
The probiotics maintain intestinal flora and prevent digestive complications like diarrhea associated with antibiotic therapy, inflammatory bowel disease, childhood diarrhea, traveler's diarrhea, lactose intolerance, Helicobacter pylori infection, irritable bowel syndrome, and bowel disease caused by Clostridium difficile [18,19]. The patients lose 20% of the microbial flora after antibiotic treatment. Probiotics are effective in the treatment and prevention of diarrhea such as rotavirus in children [20]. The rotavirus in the main cause of the gastroenteritis. The administration of water and oral electrolytes which is the considered the most common therapy, does not decrease the disease duration. Intake the probiotics decreases the diarrhea duration, especially, at the first signs of symptom onset. But, it may not be effective in treating advanced cases of gastroenteritis [21].
The strong point of this study is that we achieved successful randomization without any lost-to-follow-up children, and all patients included in the investigation adhered to the prescribed treatment course of zinc and probiotics. However, the study had some limitations. Firstly, patients were recruited from both the public and private sectors, with different recruitment days and repeat visits. While we cannot be certain of the effect of these differences, there was no significant difference between the 2 groups after 2 weeks of follow-up. Secondly, the comparison of our study with others in the discussion may not provide a complete picture of effectiveness, as many of those studies compared zinc versus placebo, while we studied the effectiveness of probiotics plus zinc versus probiotics alone. To avoid bias, both groups in our study received probiotics. Finally, we do not believe that the storage of the medicines and probiotics influenced our results since the study was conducted during the cold season.
The authors of this study suggest robust large clinical trials with 2 or more follow-up times. We followed up with the patients for 2 weeks only. We recommend that clinicians use the probiotics along with zinc based on our findings and the findings reported in the literature but not more than one week. We suggest that using probiotics and zinc be tested in severe children with gastroenteritis in the future attempts. However, the ethical challenges behind using probiotics and zinc in severe cases must be considered in the future protocols.
In conclusion, based on the results of this study, it was found that the use of probiotics plus zinc did not have a significant impact on disease severity, duration of diarrhea, maximum number of watery stools per 24 hours, duration of vomiting, maximum number of vomiting episodes per 24 hours, maximum recorded rectal temperature, unscheduled health care visits, and treatment when compared to receiving probiotics alone in children with gastroenteritis at 2 weeks. However, the children who received probiotics plus zinc recovered shorter compared to the probiotics-only group.
Footnotes
Acknowledgments
We would like to present our deep thanks to the administration of Heevi Pediatric Hospital and the parents of the children.
Table 1.
General and medical characteristics of probiotics versus probiotics plus zinc groups
| Characteristic |
Study group No (%) |
P value | |
|---|---|---|---|
| Probiotics (n=51) | Probiotics plus zinc (n=50) | ||
| Age (yr), mean±SD (range) | 1.79±1.16 (1 mo–14 yr) | 1.69±0.98 (4 mo–13 yr) | 0.645a) |
| Sex | 0.373b) | ||
| Male | 30 (58.82) | 25 (50.00) | |
| Female | 21 (41.18) | 25 (50.00) | |
| Comorbidity | 0.118b) | ||
| No | 51 (100) | 47 (94.00) | |
| Yes | 0 (0.00) | 3 (6.00)c) | |
| Treatment for acute gastroenteritis | 0.513b) | ||
| None | 49 (96.08) | 48 (96.00) | |
| Intravenous fluids | 2 (3.92) | 1 (2.00) | |
| Multiple treatment | 0 (0) | 1 (2.00) | |
| Maximum recorded temperature | 0.067b) | ||
| <37°C | 26 (50.98) | 18 (36.00) | |
| 37.1°C–38.4°C | 19 (37.25) | 28 (56.00) | |
| 38.5°C–38.9°C | 6 (11.76) | 2 (4.00) | |
| ≥39°C | 0 (0) | 2 (4.00) | |
| Receipt of antibiotics in previous 14 days | 0.741b) | ||
| No | 45 (88.24) | 46 (92.00) | |
| Yes | 6 (11.76) | 4 (8.00) | |
| Receipt of any dose of rotavirus vaccine | 0.612b) | ||
| No | 11 (21.57) | 8 (16.00) | |
| Yes | 40 (78.43) | 42 (84.00) | |
| Duration of symptoms <48 hr | 51.71±44.37 | 38.60±27.01 | 0.572a) |
Table 2.
Incidence of dehydration and disease severity of probiotics versus probiotics plus zinc groups at baseline and 2 weeks
| Dehydration and disease severity |
Study groups at baseline |
MD (95% CI) | RR (95% CI) | P value | |
|---|---|---|---|---|---|
| Probiotics (n=51) | Probiotics plus zinc (n=50) | ||||
| Dehydration score | 1.53±0.99 | 1.80±0.78 | 0.27 (-0.08 to 0.62) | 0.131a) | |
| Dehydration | 0.088b) | ||||
| No dehydration | 9 (17.65) | 2 (4.00) | Reference | ||
| Some dehydration | 41 (80.39) | 47 (94.00) | 1.17 (1.2–1.39) | ||
| Moderate/severe dehydration | 1 (1.96) | 1 (2.00) | 3.33 (0.29–38.7) | ||
| Disease severity | 6.12±2.05 | 6.66±2.33 | 0.54 (-0.32 to 1.41) | 0.216a) | |
| Disease severity category | 0.109b) | ||||
| Mild gastroenteritis | 46 (90.20) | 39 (78.00) | Reference | ||
| Moderate-to-severe gastroenteritis | 5 (9.80) | 11 (22.00) | 2.24 (0.84–5.99) | ||
| Dehydration and disease severity |
Study groups at 2 weeks |
MD (95% CI) | RR (95% CI) | P value | |
| Probiotics (n=51) | Probiotics plus zinc (n=50) | ||||
| Dehydration score | 0 | 0 | NA | NA | |
| Dehydration | 1.000 | ||||
| No dehydration | 49 (96.08) | 48 (96.00) | |||
| Some dehydration | 2 (3.92) | 2 (4.00) | 1.02 (0.15–6.96) | ||
| Disease severity | 0 | 0 | NA | NA | |
| Disease severity category | 0.495 | ||||
| No gastroenteritis | 51 (100) | 49 (98.00) | |||
| Mild gastroenteritis | 0 (0) | 1 (2.00) | 1.02 (0.07–15.84) | ||
Table 3.
Dehydration characteristics and disease severity components of probiotics versus probiotics plus zinc groups of children with gastroenteritis at 2 weeks
Table 4.
Dehydration and disease severity at pre- and post-treatment in probiotics versus probiotics plus zinc groups
| Dehydration and disease severity |
Probiotics (n=51) |
MD (95% CI) | P value | |
|---|---|---|---|---|
| Baseline | Two weeks | |||
| Dehydration score | 1.53 | 0 | -1.53 (-1.81 to -1.25) | <0.001a) |
| Disease severity | 6.12 | 0 | -6.12 (-6.69 to -5.54) | <0.001a) |
| Dehydration | <0.001b) | |||
| No dehydration (ref) | 9 (17.65) | 49 (96.08) | Reference | |
| Some dehydration | 41 (80.39) | 2 (3.92) | 0.05 (0.01–0.19) | |
| Moderate/severe dehydration | 1 (1.96) | 0 (0) | 0.20 (0.13–2.99) | |
| Disease severity category | <0.001b) | |||
| No gastroenteritis (ref) | 0 (0) | 51 (100) | Reference | |
| Mild gastroenteritis | 46 (90.20) | 0 (0) | 0.02 (0.002–0.14) | |
| Moderate-to-severe gastroenteritis | 5 (9.80) | 0 (0) | 0.02 (0.002–0.14) | |
| Dehydration and disease severity |
Probiotics plus zinc (n=50) |
MD (95% CI) | P value | |
| Baseline | Two weeks | |||
| Dehydration score | 1.80 | 0 | -1.8 (-2.02 to -1.58) | <0.001a) |
| Disease severity | 6.66 | 0 | -6.66 (-7.32 to -6.00) | <0.001a) |
| Dehydration | <0.001b) | |||
| No dehydration (ref) | 2 (4.00) | 48 (96.00) | Reference | |
| Some dehydration | 47 (94.00) | 2 (4.00) | 0.04 (0.01–0.16) | |
| Moderate/severe dehydration | 1 (2.00) | 0 (0) | 0.06 (0.005–0.77) | |
| Disease severity category | <0.001b) | |||
| No gastroenteritis (ref) | 0 (0) | 49 (98.00) | Reference | |
| Mild gastroenteritis | 39 (78.00) | 1 (2.00) | 0.02 (0.022–0.14) | |
| Moderate-to-severe gastroenteritis | 11 (22.00) | 0 (0) | 0.02 (0.022–0.14) | |
Table 5.
Other outcomes of children in probiotics versus probiotics plus zinc groups
| Outcome |
Study groups at 2 weeks no (%) |
MD (95% CI) | RR (95% CI) | P value | |
|---|---|---|---|---|---|
| Probiotics (n=51) | Probiotics plus zinc (n=50) | ||||
| Receipt of intravenous fluids | 1.000b) | ||||
| No | 50 (98.04) | 50 (100) | 1.02 (0.07–15.84) | ||
| Yes | 1 (1.96) | 0 (0) | - | ||
| Hospital admission | 1.000b) | ||||
| No | 50 (98.04) | 50 (100) | 1.02 (0.07–15.84) | ||
| Yes | 1 (1.96) | 0 (0) | - | ||
| Repetition of Emergency Department visitc) | 0.495b) | ||||
| No | 51 (100) | 49 (98.00) | 1.02 (0.07–15.84) | ||
| Yes | 0 (0) | 1 (2.00) | - | ||
| Healing day | 2.00±0.0 | 1.34±0.81 | -0.66 (-0.89 to -0.44) | <0.001a) | |
| Healing duration (day) | - | 0.031 | |||
| 1–2 | 36 (70.59) | 44 (88.00) | 0.41 (0.17–0.97) | ||
| 3–7 | 15 (29.41) | 6 (12.00) | |||
References
1. Elliott E, Moyer V. Evidence-based pediatrics and child health. Hoboken (NJ): John Wiley & Sons, Inc., 2008.
2. Nazarian L, Berman J. Practice parameter: the management of acute gastroenteritis in young children. Pediatrics 1996;97:424–35.



3. Critchley M, MacNalty AS. Butterworths medical dictionary. London: Butterworth, 1980.
4. GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis 2017;17:909–48.


5. Vesikari T, Van Damme P, Giaquinto C, Dagan R, Guarino A, Szajewska H, et al. European Society for Paediatric Infectious Diseases consensus recommendations for rotavirus vaccination in Europe: update 2014. Pediatr Infect Dis J 2015;34:635–43.

6. Wardlaw T, Salama P, Brocklehurst C, Chopra M, Mason E. Diarrhoea: why children are still dying and what can be done. Lancet 2010;375:870–2.


7. United Nations Children’s Fund (UNICEF)/World Health Organization (WHO). Diarrhoea: why children are still dying and what can be done. New York (NY): UNICEF/Geneva (Switzerland): WHO, 2009.
8. Lazzerini M, Wanzira H. Oral zinc for treating diarrhoea in children. Cochrane Database Syst Rev 2016;12:CD005436.


9. Rouhani P, Rezaei Kelishadi M, Saneei P. Effect of zinc supplementation on mortality in under 5-year children: a systematic review and meta-analysis of randomized clinical trials. Eur J Nutr 2022;61:37–54.



10. Patro B, Golicki D, Szajewska H. Meta analysis: zinc supplementation for acute gastroenteritis in children. Aliment Pharmacol Ther 2008;28:713–23.


12. Friedman JN, Goldman RD, Srivastava R, Parkin PC. Development of a clinical dehydration scale for use in children between 1 and 36 months of age. J Pediatr 2004;145:201–7.


13. Schnadower D, Tarr PI, Gorelick MH, O'Connell K, Roskind CG, Powell EC, et al. Validation of the modified Vesikari score in children with gastroenteritis in 5 US emergency departments. J Pediatr Gastroenterol Nutr 2013;57:514–9.



14. Ahmadipour S, Mohsenzadeh A, Alimadadi H, Salehnia M, Fallahi A. Treating viral diarrhea in children by probiotic and zinc supplements. Pediatr Gastroenterol Hepatol Nutr 2019;22:162–70.




15. Kulkarni H, Mamtani M, Patel A. Roles of zinc in the pathophysiology of acute diarrhea. Curr Infect Dis Rep 2012;14:24–32.



16. Canani RB, Buccigrossi V, Passariello A. Mechanisms of action of zinc in acute diarrhea. Curr Opin Gastroenterol 2011;27:8–12.


17. Kakar Z, Essazai AB, Ahmed SM, Ullah N, Jan P. Comparison of zinc-probiotic combination therapy to probiotic therapy alone in treating acute diarrhea in children. Pakistan J Medical Health Sci 2022;16:253–5.

18. Goldenberg JZ, Yap C, Lytvyn L, Lo CK, Beardsley J, Mertz D, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev 2017;12:CD006095.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link PubMed
PubMed Download Citation
Download Citation


