Needle aspiration as therapeutic management for suppurative cervical lymphadenitis in children
Article information
Abstract
Purpose
This study aimed to evaluate the usefulness of the needle aspiration alternative to open surgical drainage of children with suppurative cervical lymphadenitis requiring surgical drainage.
Methods
From January 1998 to June 2008, we retrospectively reviewed 38 children treated with needle aspiration as management with suppurative cervical lymphadenitis instead of open surgical drainage.
Results
All 38 children underwent only 1 puncture. Two patients (5.2%) out of 38 patients experienced reformation of an abscess and all recovered completely after re-treatment with antibiotics. Minor complications were detected in 2 patients (5.2%). One complication originated from remnant necrotic tissue and the other involved formation of a small scar in two patients, which resolved spontaneously. There were no major complications.
Conclusion
Needle aspiration can be a simple, safe, and effective alternative procedure to open surgical drainage of children with suppurative cervical lymphadenitis requiring surgical drainage.
Introduction
Cervical lymphadenitis refers to inflammation of one or more lymph nodes of the neck. This condition is a common problem in the pediatric age group and largely infectious in etiology. The most commonly involved lymph nodes are the submandibular, upper cervical, submental, occipital, and lower cervical nodes1). Large (>2-3 cm), solitary, tender, unilateral cervical lymph nodes that rapidly enlarge in the preschool age child are commonly due to bacterial infection2). Staphylococcus aureus and group A streptococcus are the most common bacterial pathogens3).
If there is a failure to respond to antibiotics medication, open surgical drainage is recommended for treatment of cervical lymphadenitis4-6). But this invasive procedure usually requires general anesthesia and may result in a disfiguring scar7). Therefore, needle aspiration for suppurative cervical lymphadenitis in children not only can be an alternative method to an open surgical drainage procedure, but also an effective and safe treatment of suppurative cervical lymphadenitis in other studies7, 8).
There is no data and a study about needle aspiration for the pediatric suppurative cervical lymphadenitis in Korea. The purpose of this study was to evaluate the effectiveness and usefulness of the needle aspiration alternative to open surgical drainage of patient with suppurative cervical lymphadenitis that required surgical drainage.
Materials and methods
Data were collected on children diagnosed with suppurative cervical lymphadenitis at Pusan National University Hospital from January 1998 to June 2008 who underwent needle aspiration. They were referred for a drainage procedure because they needed to require open surgical drainage. We studied 38 children with suppurative cervical lymphadenitis that required open surgical drainage as management of infected lymph nodes.
The aspiration procedure was done using 18 or 21 gauge needle under US guide. After a local anesthetic ointment (EMLA®, Astra, Södertälje, Sweden) was applied for 1 hour before the aspiration in all patients, aspiration was performed until there was no return in the 5 mL syringe. In noncooperative patients, a conscious sedation with midazolam (0.05-0.1 mg/kg) was done with oxygen monitoring throughout the procedure. The aspirated specimen was sent for microbiologic culture study to the microbiology laboratory.
For the clinical database, we retrospectively collected demographic details, clinical characteristics, laboratory data, presentation of involved lymph nodes, and culture of aspirated fluid. We excluded anatomical anomalies, immunologic abnormality, BCG lymphadenitis, and TB lymphadenitis. Statistical analysis was performed using Student's t-test and chi-square analysis.
Results
1. Demographic characteristics
Thirty-eight children underwent needle aspiration for treatment with suppurative cervical lymphadenitis that required surgical drainage (Table 1). There were 15 males and 23 females. Mean age was 2.6±2.5 years (range: 0.1-10.0 years). The patient population was representative of a wide range of age groups, including 11 children from age 0 to 1 years, 16 children from 1 to 4 years, 10 children from 4 to 8 years, 1 child > 8 years of age. Patients typically present with a clinical manifestation of tenderness (78.9%), fever (71.0%), redness (55.3%) and heating sensation (52.6%).
Average WBC count and C reactive protein was 19,500±7,265/µL (range: 7,600-37,440/µL) and 6.35±6.97 mg/dL (range: 0.22-26.8 mg/dL). There was no statistical difference between patients who presented high white blood count and C reactive protein, and those with low counts concerning the characteristic of lymph nodes. All of the 38 patients received one or two antibiotic medications before needle aspiration. Twenty-three patients received one antibiotic treatment and fifteen patients received two antibiotic treatments. The antibiotics administered before needle aspiration included nafcillin (16 cases), cefazolin (9 cases), nafcillin and cefotaxime (3 cases), ampicillin/sulbactam and cefotaxime (3 cases), cefazolin and clindamycin (3 cases), nafcillin and clindamycin (2 cases), ampicillin/sulbactam and clindamycin (2 cases).
Mean duration of antibiotics before needle aspiration was 4.8±2.7 days and mean total duration of antibiotics treatment was 21.6±13.9 days. Mean duration of hospitalization was 13.7±9.4 days (range: 5-59 days).
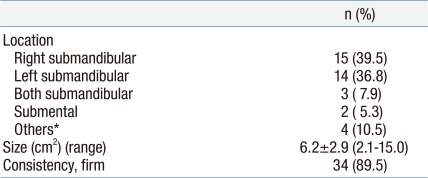
2. Characteristics of lymph nodes
The most common site of infected lymph nodes is the submandibular lymph node. Thirty-two patients (84.2%) presented submandibular lymph nodes, two patients with submental lymph node, each patient with retropharyngeal, preauricular, paravertebral and multiple lymph nodes (Table 2). Twenty-nine (90.6%) of 32 patients with submandibular lymph node were unilaterally involved lymph nodes. The mean size of involved lymph nodes is 6.2±2.9 cm2 (range: 2.1-15.0 cm2). The size of submandibular lymph nodes ranged from 2.1 to 12.0 cm2 (mean 5.8 cm2). The size of abscess pocket ranged from 1.0 to 4.0 cm2 (mean 1.9 cm2). The amount of fluid aspirated for any 1 case ranged from 0.3 to 6.0 mL (mean 1.7 mL). Thirty-four (89.5%) lymph nodes were firm in consistency at the time of needle aspiration. Hospitalization duration was not related with the size of the lymph nodes and prior antibiotic treatment.
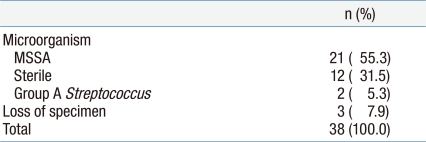
3. Culture of aspirated fluid
Bacterial cultures were sent to the laboratory on all patients, but the specimens of three patients were lost (Table 3). Cultures from twenty-one (60.0%) out of 35 patients confirmed that culture of aspirated fluid grew out of S. aureus. Of the S. aureus isolates that grew in culture, 100% were methicillin-sensitive S. aureus (MSSA). Of MSSA isolates, 100, 75, 60 % were sensitive to clindamycin, trimethoprim/sulfamethoxazole, ciprofloxacin, respectively. Cultures from two (5.7%) patients grew out Streptococcus pyogenes. Cultures from 12 patients (34.3%) grew out of no organisms.
Discussion
Suppurative cervical lymphadenitis is a common problem in children. Most children with this condition are treated successfully without complication. Forty to eighty percent of cases of acute unilateral cervical lymphadenitis of 1- to 4-year old children are due to S. aureus or S. pyogenes1). Antibiotics should be targeted against S. aureus and group A streptococcus , and should include a 10-day course of oral cephalexin, amoxicillin/clavulanate, or clindamycin9). In most cases, symptomatic improvement should be noted after 2 to 3 days of therapy, although complete resolution of nodal enlargement may require several weeks2).
The initial treatment approach of patients with suppurative cervical lymphadenitis that had failed to respond to antibiotic treatment is open surgical drainage. Some investigators reported considering an open approach when there is no improvement after 48-72 hours of appropriate antibiotic treatment4, 10). But in the pediatric age group, open surgical drainage has some limitations. It needs to be performed under general anesthesia, and may be associated with disfiguring scars. Other limitations are longer hospitalization and peri- and post-operative morbidity.
In our study, needle aspiration is mentioned as a therapeutic rather than diagnostic procedure. Needle aspiration is limited evidence to suggest a single definitive approach to the work-up and treatment of a child with suppurative cervical lymphadenitis. But it has been used successfully in patients with atypical mycobacterial cervical adenitis11).
In a previous study, Gorenstein et al8) reported that therapeutic needle aspiration was an attractive alternative to an open incision and drainage procedure. They suggested that seven (70%) out of 10 patients had 1 puncture and all patients had no scars and relapses of lymph nodes. All patients responded favorably to the procedure with defervescence and gradual regression of the cervical mass. Serour et al7) reported needle aspiration as the treatment of suppurative cervical lymphadenitis that required drainage procedures in thirty-five children seems to be an effective and safe treatment of suppurative cervical lymphadenitis that may avoid open surgical drainage. Twenty-seven (77.1%) out of 35 children underwent 1 puncture. There were no major complications and no relapses or scar formation.
In our study, thirty-eight children underwent needle aspiration treatment with suppurative cervical lymphadenitis that required open surgical drainage. All patients underwent only 1 puncture. Two patients (5.2%) out of 38 patients experienced reformation of an abscess and all recovered completely after antibiotic retreatment. Two patients that experienced reformation of an abscess received initially antibiotic treatment against S. aureus and group A streptococcus because the most common pathogens are S. aureus and group A streptococcus3). After isolation in culture, antibiotic re-treatment is based on determination of the etiological agent and its relevant antibiotic sensitivity. A minor complication was detected in 2 patients. One was remnant necrotic tissue and the other was a small scar formation, which was resolved spontaneously in both patients. Similar to other studies, there were no major complications in our study. But two (5.2%) out of 38 patients had a minor complication that was not troublesome and was resolved spontaneously.
In conclusion, the advantage of needle aspiration over open surgical drainage is that it is a simple, safe and effective procedure which does not require general anesthesia. Our study had several limitations. First, this was a retrospective study. Second, this single-center study included only a small number of patients. Therefore, further investigation is clearly needed to determine an initial approach of patients with suppurative cervical lymphadenitis that required open surgical drainage through prospective and large-scale studies.