Role of colonoscopy in the diagnosis and treatment of pediatric lower gastrointestinal disorders
Article information
Abstract
The safety and effectiveness of colonoscopy in the investigation of lower gastrointestinal tract pathology in children has been established for more than 2 decades in Korea. Skill and experience have since advanced to the point that both diagnostic and therapeutic colonoscopy are now routinely performed by most pediatric gastroenterologists. Pediatric colonoscopy differs significantly from its adult parallels in nearly every aspect including patient and parent management and preparation, selection criteria for sedation and general anesthetic, bowel preparation, expected diagnoses, instrument selection, imperative for terminal ileal intubation, and requirement for biopsies from macroscopically normal mucosa. Investigation of inflammatory bowel disease, whether for diagnosis or follow-up evaluation, and suspected colonic polyps are the most common indication for pediatric colonoscopy. The child who presents with signs and symptoms of lower gastrointestinal disorder should undergo colonoscopy with biopsy to make the diagnosis, as well as to help determine the appropriate therapy. This review introduces practical information on pediatric colonoscopy, the author's experiences, and the role of colonoscopic examination in the diagnosis and treatment of pediatric lower gastrointestinal disorders.
Introduction
Experience with flexible colonoscopy in infants and children trailed slightly behind that with flexible upper tract endoscopy. Initial reports of pediatric colonoscopy appeared in the literature during the late 1970s and extended into the 1980s1). Skill and experience have since advanced to the point that both diagnostic and therapeutic colonoscopies are now routinely performed by most pediatric gastroenterologists. Currently available equipment permits examination of all pediatric age groups including the neonate. Successful completion of total colonoscopy with or without examination of the terminal ileum is technically challenging in any patient age. Pediatric patients introduce an additional level of complexity to the procedure due to their poor compliance or cooperation, with the need for bowel preparation and with the difficulties in sedating a frightened, agitated, or otherwise uncooperative patient1).
The first report on pediatric colonoscopy in Korea was made by Park EB2) who was an internist. In 1990s, 2 reports concerning pediatric colonoscopy were published in a large population by Seo JK3, 4). The history of pediatric colonoscopy in Korea is about 20 years and the experience of pediatric colonoscopy may still be trifle. This review introduces the practical information on pediatric colonoscopy, the author's experiences, and the role of colonoscopic examination in the diagnosis and treatment of pediatric lower gastrointestinal (GI) disorders.
Indications and contraindications of colonoscopy
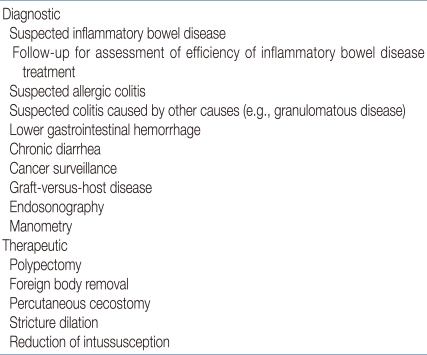
The indications for colonoscopy in children are listed in Table 15). The power of colonoscopy lies in its simultaneous ability to visually inspect the entire length of the colon, often including the distal ileum, the sample tissue for histology, and intervene therapeutically by applying hemostasis, removing polyps, dilating strictures, or decompressing the obstructed bowel. Investigation of inflammatory bowel disease, whether for diagnosis or follow-up evaluation, and suspected colonic polyps are the most common indication for pediatric colonoscopy in European and North American society6-8).
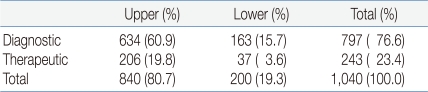
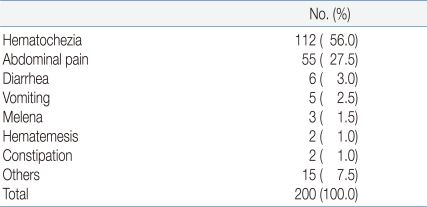
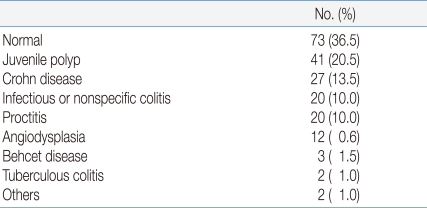
The author reviewed 1,040 endoscopy reports from Pusan National University Hospital from January 2001 to June 20059). Neonates and infants accounted for 6.0% and 16.5% respectively. The mean age was 8.5±2.1 years. Two hundred procedures (19.3%) were considered colonoscopies. Therapeutic lower GI endoscopies were performed in 37 children (polypectomy in 92%, argon laser cauterization for angiodysplasia in 4%) (Table 2). The main causes leading to colonoscopy were hematochezia (56.0%), abdominal pain (27.5%), and diarrhea (3.0%) (Table 3). The most common endoscopic diagnoses were juvenile polyp in 20.5% and Crohn disease in 13.5% (Table 4).
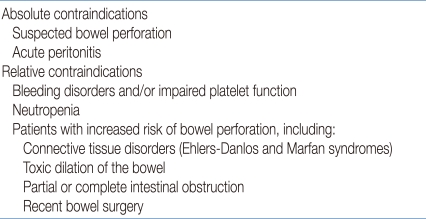
The contraindications for colonoscopy are similar to those for upper GI endoscopy (Table 5)10). Cardiovascular, respiratory, or neurologic instability usually preclude safe colonoscopy. Coagulopathy should be corrected before proceeding with colonoscopy. Colonoscopy is contraindicated when bowel perforation is suspected. Neutropenia and suspected bowel ischemia should be considered relative contraindications. Inadequate bowel preparation can be a cause of cancellation of colonoscopy.
Preparation for colonoscopy
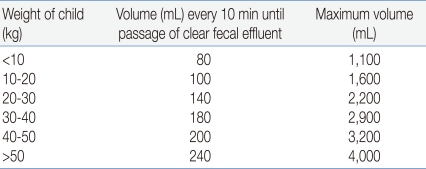
In addition to fasting, colonoscopy can be successfully only if the colon is free of fecal debris. Many bowel preparations have been successfully utilized to cleanse the colon. The method depends on the age and cooperation of the child, and the individual experience of the examiner. In infants, adequate preparation can usually be obtained with the use of small-volume enemas by substituting clear liquids for milk for 12-24 h. In older children and adolescents, the best preparation is usually done with the use of colonic lavage solutions that contain a nonabsorbable solution of polyethylene glycol and electrolytes (PEG-ELS), which causes osmotic diarrhea11). To be effective, a large volume of solution must be ingested over a relatively short period. Table 6 shows the volume at every 10 min and the maximum volume of PEG-ELS oral solution according to the body weight of the child5).
Sedation in pediatric endoscopy
With increased experience, careful screening, and the specialization in pediatric gastroenterology, endoscopy can now be performed safely with intravenous (IV) sedation on almost all patients12). Although safe, the sedation of pediatric patients has serious associated risks, such as airway obstruction, hypoxia, hypoventilation, apnea, and cardiopulmonary arrest.
The American Academy of Pediatrics has defined conscious sedation as a medically controlled state of depressed consciousness that (1) allows protective reflexes to be maintained, (2) retains the patient's ability to maintain a patent airway continuously, and (3) permits appropriate patient response to physical stimulation or verbal command13).
Conscious sedation should be used as the main sedation modality for most pediatric endoscopies; however, deep sedation or general anesthesia should be used for specific cases. The approach to sedation varies among institutions and among physicians. In children, the perceived intolerance of colonoscopy under conscious sedation, as well as fear of complications, many pediatric endoscopists has done colonoscopy under general anesthesia7, 14). However, the author has done colonoscopy only under conscious sedation9, 15).
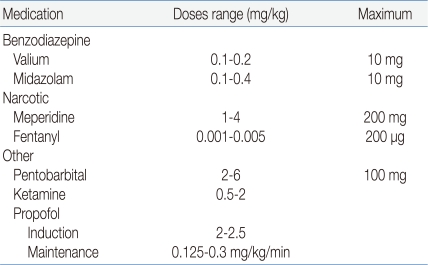
The three broad groups of IV medications commonly used for sedation during endoscopy are (1) benzodiazepines, (2) narcotics, and (3) nonbarbiturates. Combination therapy is often used (Table 7)16).
Rescue medications
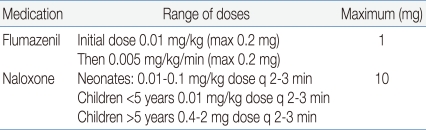
Opiates and benzodiazepines have specific antagonists to reverse overmedication. These medications are usually given to patients who become apneic or unable to maintain oxygenation levels even with supplemental oxygen. Flumazenil may benefit patients who develop paradoxic agitation following adminstration of benzodiazepines. The usual doses are listed in Table 816). The routine use of flumazenil after completion of the procedure has not been shown to shorten recovery time in children.
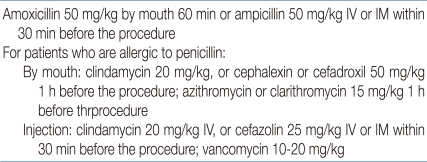
Antibiotic prophylaxis
The incidence of bacteremia after gastrointestinal endoscopy varies according to the patient's underlying medical problem and the procedure performed: colonoscopy 0-25% (mean 4.4%)17). Certain bacteria are more likely to be the cause of bacteremia after a procedure. These include Escherichia coli, Bacteroides, Pseudomonas, Veillonell, and Peptostreptococcus18). However, other bacteria may be more virulent and more likely to cause endocarditis, especially Streptococcus viridans and enterococcus19). Prophylaxis is directed by the frequency and virulence of the anticipated organisms that may be encountered during the procedure. The current antibiotic recommendations for prophylaxis are outlined in Table 910).
Complications of colonoscopy
Sedation complications during colonoscopy are similar to those reported during upper gastrointestinal tract examination. Several series have demonstrated a correlation between the frequency of technical complications during colonoscopy and the experience of the endoscopist10).
Bleeding after colonoscopy is usually minimal but may follow mucosal biopsy or polypectomy. Bleeding following a diagnostic procedure has been reported in 0.008-0.1% of procedures in adults and is likely as rare in children10). Bleeding following polypectomy is also uncommon, but may occur in 0.26-2.5% of patients depending on the series20, 21). Perforation is the most serious complication of colonoscopy in children. It is usually related to polypectomy and can be successfully managed with surgical intervention. The risk ranges from 0.06% to 0.3%14, 20, 22). In the author's study, colonic perforation occurred in 1 patient (0.5%) who underwent argon plasma coagulation for ablation of multiple angiodysplasia in the colon. However, no bleeding did not occur after polypectomy or mucosal biopsy occurred9, 23).
Specific diagnostic and therapeutic applications
1. Inflammatory bowel disease
Once considered rare in pediatric practice in Korea, inflammatory bowel disease, especially Crohn disease, is now being recognized with increasing frequency in children15). In fact, Crohn disease presents before the age 20 years in 25% to 30% of all patients24). Four percent of pediatric inflammatory bowel disease occurs before the age of 5 years, with a peak age of onset in the adolescent years25). With the increasing recognition of IBD among pediatric patients, it has become one of the most significant chronic diseases affecting children and adolescents25).
In addition to the usual gastrointestinal symptoms, children may exhibit prominent extraintestinal manifestations such as growth failure, delayed puberty, osteoporosis, and joint pain26). These symptoms may be subtle. The presence of perianal disease and occult fecal blood suggest the diagnosis of Crohn disease. The next step in the diagnostic evaluation includes radiologic examination and endoscopic evaluation. Gastrointestinal endoscopy with biopsy is an essential tool for the diagnosis of Crohn disease and ulcerative colitis in children27). Endoscopy also helps define the extent and severity of disease, which may identify complications and influence initial management28).
The author reviewed 30 cases of Crohn disease in Pusan National University Hospital from January 1996 to December 2005 (actual period 8 years)15). The actual number of newly diagnosed patients with Crohn disease has increased during the 8-year period. The mean age at diagnosis was 10.6±4.3 years. Crohn disease was localized in the small bowel in 33.3%, the large bowel in 12.5%, and both the small and large bowel in 54.2%.
Up to 85% of all patients with Crohn disease have evidence of terminal ileal disease, which is confirmed using colonoscopy and ileal biopsy29). Batres LA et al.14) reviewed 2,038 endoscopy reports from the Children's Hospital of Philadelphia which is one of the most famous GI center in the United States, from 1994 to 1996 and 1999 to 2000; 1,516 (74%) procedures were considered colonoscopies. Between the years 1994 and 1996, 637 colonoscopies were performed (average of 212 per year) with a success rate of terminal intubation of 21.5%. Between 1999 and 2000, 879 colonoscopies were performed (average 440 per year) with a success rate of terminal ileum intubation of 65.6%. There were 2 colonic perforations, 1 in each time period. The colonic perforation rate was 0.16% and between 1994 and 1999, and 0.11% between 1999 and 2000.
In the author's study9), 1,040 patients underwent endoscopy from January 2001 to June 2005 (4 years and 6 months); 200 (19.3%) procedures were considered colonoscopies (average of 44.4 per year). Between January 2009 and June 2010, 729 endoscopies were performed; 189 (25.9%) procedures were colonoscopies (average of 126 per year). The data suggest that the number of colonoscopic examination is increasing. The success rate of terminal ileum intubation was higher than that of the latter period in Batres' report.
2. Lower gastrointestinal tract hemorrhage
Rectal bleeding is not uncommon in children. However, it is alarming for parents and requires further investigation. The differential diagnosis is extensive and includes anal fissure, hemorrhoid, gastrointestinal infection, inflammatory bowel disease, allergic colitis, polyps, and GI malignancy. Colonoscopy has become a standard procedure, and studies have demonstrated its efficacy in the diagnosis of hematochezia of lower gastrointestinal GI origin8, 30). The benefits of colonoscopy in rectal bleeding include identification of the site of bleeding, the low risk of complications of the procedure, and the possibility of endoscopic intervention31).
Polyps are the most common causes of rectal bleeding in children. Polyps occur in 1% of children, and 90% of these are juvenile polyps32). Juvenile polyps are generally thought to be hamartomatous lesions with little malignant potential. Juvenile polyps have been reported to be solitary and rectosigmoid in location in 80-90% of cases33, 34). However, some of the recent studies revealed that a significant number of cases of polyps are multiple and proximally located, which emphasizes the need for total colonoscopy in all cases34, 35). The first report of clinical experience in pediatric colonoscopic polypectomy was made by Gans et al.36) in 1975. Colonoscopic polypectomy is now an established therapeutic modality for the treatment of colorectal polyps37). In the author's study9), hematochezia was the first main cause (56.0%) leading to colonoscopy (Table 3) and juvenile polyp was the most common endoscopic diagnosis (Table 4).
The frequency of angiodysplasia of the colon as a cause of lower intestinal bleeding is 40% among adults38) and is unknown in children. Angiodysplasia is also known as arteriovenous malformation, vascular dysplasia, vascular ectasia, colonic ectasia, and hamartoma39). These lesions have varied clinical expressions, with lower intestinal bleeding being the most common problem. Argon plasma coagulation is a noncontact form of monopolar coagulation and has been shown to be safe and effective for management of GI bleeding in children40). The author have also determined the efficacy of argon plasma coagulation on ablation of colonic angiodysplasia23).
Conclusion
Pediatric GI endoscopists are able to perform almost all endoscopic techniques. At the same time, they are developing unique applications of these techniques for pediatric patients. Pediatric GI endoscopists have the advantage of being familiar not only with age-related physiologies but also with the spectrum of disease in pediatric patients. The referring physician and endoscopist should be familiar with the risks and benefits of endoscopy, as well as clinical situations in infants and children in which the procedure is most likely to be useful.
In conclusion, the child who presents with signs and symptoms of lower GI disorder should undergo colonoscopy with biopsy to make the diagnosis, as well as to help determine the appropriate therapy. Colonoscopy is a safe procedure in the pediatric population.