Testicular torsion in the inguinal region in an extremely low birth weight infant
Article information
Abstract
Testicular torsion is rare in newborn infants. However, its frequency has increased, most of which are reported in full-term infants. We diagnosed and treated testicular torsion in an extremely low birth weight infant (ELBWI). A 2×2 cm red mass was palpable in the left groin of a 24-week-old, 745 g, male newborn at 23 days of age. Left testicular torsion was diagnosed, and emergent orchiopexy was performed. Careful physical examination is needed in cases suspicious of testicular torsion in ELBWIs with cryptorchidism. Moreover, early diagnosis and emergent exploration are necessary to prevent complications such as the risk of anorchia.
Introduction
Testicular torsion occurs in the prenatal or the postnatal period, which is scarcely recognized in neonates1). Fertility might be lost without immediate surgical operation on diagnosing it1). The authors promptly diagnosed and managed the testicular torsion in inguinal region in an extremely low birth weight infant (ELBWI). We report this case taking account of the fact that there have not been any case reports on the occurrence of testicular torsion in inguinal region in an ELBWI.
Case report
A 24-week, 745-g appropriate-for-gestational-age boy was born by vaginal delivery. The pregnancy was complicated by the onset of premature labor and Apgar scores were 3 at 1 minute, 5 at 5 minutes. He was intubated immediately right after the birth in the delivery room, given surfactant and put on a conventional ventilator for the treatment of respiratory distress syndrome. At the initial physical examination of birth, the testes were palpable in both of the inguinal regions because of the cryptorchidism with no other specific findings. However, apparent specifics were not noticed.
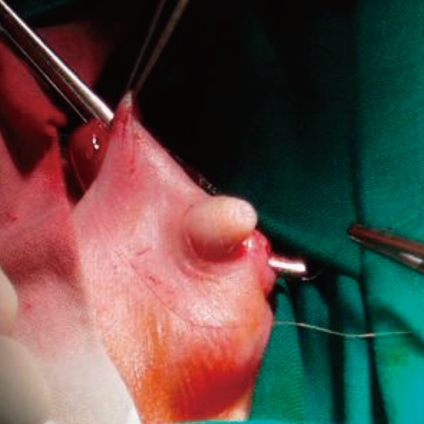
At 23 days of age, a newly recognized firm and enlarged 2×2 cm mass was observed in the left inguinal region where the previously described undescended testis was located (Fig. 1). It was an emergency and evaluated by the ultrasound of the inguinal canal as quickly as possible. There was no blood flow in the left testis, but heterogeneous echogenicity was observed by Color Doppler ultrasonography. Contralateral inguinal area was normal and testis was not palpable in the right scrotum. Consequently, unilateral testicular torsion was suspected in the left inguinal region, which made us perform an emergency exploration under general anesthesia. Tunica vaginalis covering the left testis appeared to represent dark blue color on surgical operation. Fluid in the incised tunica vaginalis was drained. The left testis was subtly discolored pink and twisted, but was not necrotic in appearance (Fig. 2). The spermatic cord was edematous and the hematoma was observed around the cord. After checking potential viability in the left testis through manual reduction, we performed left orchiopexy (Fig. 3). The contralateral testis was not operated because it was an ELBWI and respiratory distress made it unlikely to persevere the operation under general anesthesia.
At 4-month follow-up after orchiopexy, both testes remained within the scrotum with good flow on ultrasound. There was no recurrence after the discharge from neonatal intensive care unit.
Discussion
Neonatal testicular torsion is divided into two groups. One is prenatal testicular torsion presenting at birth. The other is postnatal testicular torsion occurring within the first 30 days of life2). 72.4% of neonatal torsion is prenatal and 27.5% postnatal2). In our case, testicular torsion occurred at 23 days of age, which fell into postnatal category. In spite of the speculation that the torsion might have been perinatal at birth, both testes were palpable in inguinal area and there was no discoloration. Besides, the perinatal torsion of the spermatic cord is normally irrelevant to prematurity and low birth weight, and it occurs bilaterally2). To summarize, considering that our case is unilateral testicular torsion in the left inguinal region and diagnosed in an ELBWI, it can be confirmed as postnatal torsion.
Testicular torsion can also be divided into "intravaginal" and "extravaginal" torsion3). Intravaginal torsion is seen mostly in older children and adult, which is related with tunica vaginalis that not only surrounds the testicle and most of the epididymis, but also surrounds the spermatic cord allowing free ration of the structures within the tunica3). On the other hand, extravaginal torsion is seen mainly in neonates3), which is associated with the lack of tunica vaginalis attachment to the scrotum4), occurring at the level of the spermatic cord5). However, one distinctive feature of intravaginal torsion of our case is that it is observed in an ELBWI and at 23 days of age.
The etiology of neonatal testicular torsion is unclear1, 6, 7). Especially, the cause of torsion in the undescended testes has not been found yet8). But we assume the causes of the testicular torsion in our case as follows.
First, the undescended testis can be the cause of the testicular torsion. The torsion within the inguinal canal is rare despite the fact that 75% of undescended testes are located there8). However, as suggested in a report, testicular torsion can be one of the complications of the cryptorchism9). The incidence of cryptorchism in preterm babies is 30%, which is much higher than that of fullterm infants' 3.4%8, 9). Considering this, the testicular torsion is likely to occur in preterm infants with high incidence of undescended testes.
Second, the warm inguinal region of the lower abdomen and debris of the intra-abdomen may inhibit the migration of the undescended testes and cause the testicular torsion through the incomplete closure of the process vaginalis. The testicular descent into the scrotum requires lower temperature, which is cooling hypothesis of the testes in human9, 10). The infant in our case had bloody stool 2 days before the presentation of the testicular torsion, which made us suspect necrotizing enterocolitis stage IB. Thinking that the necrotizing enterocolitis made testes in inguinal canal warmer and debris from intestinal mucosa descend into tunica vaginalis through a patent process vaginalis, we supposed that this intestinal inflammation had stimulated the testicular torsion. Consequently, we need to consider the possibility of testicular torsion in preterm and newborn infants who have undescended testes with intestine infections such as necrotizing enterocolitis or enteritis.
Though the prophylactic fixation of contralateral testis is recommended, we left the other normal part not being operated. That was because we considered that this infant with extremely low birth weight might have the poor rates of surgical salvage and the high surgical and anesthetic risks.
The salvage rate of the testicular torsion is in between 20% to 40%, depending on the prompt surgical intervention8). In the experimental models of testicular ischemia, spermatogenesis is lost after 6 hours and endocrine secretion ceases at 10 hours4, 7). Besides, when patients with testicular torsion were followed up without immediate surgery, affected testis showed progressive atrophy3, 5). Therefore, our emergent operation was thought to be done right after the immediate diagnosis because there was neither discoloration nor ischemia of the left testis. Moreover, at 4 months post operative follow-up, this patient had normal blood flow by color Doppler ultrasound of testes. And there was no recurrence observed even after one year. Regular long-term follow-up is essential, however, to determine endocrine and fertility potential as an anorchia.