Treatment of obstructive sleep apnea in children
Article information
Abstract
Obstructive sleep apnea (OSA) in children is a frequent disease for which optimal diagnostic methods are still being defined. Treatment of OSA in children should include providing space, improving craniofacial growth, resolving all symptoms, and preventing the development of the disease in the adult years. Adenotonsillectomy (T&A) has been the treatment of choice and thought to solve young patient's OSA problem, which is not the case for most adults. Recent reports showed success rates that vary from 27.2% to 82.9%. Children snoring regularly generally have a narrow maxilla compared to children who do not snore. The impairment of nasal breathing with increased nasal resistance has a well-documented negative impact on early childhood maxilla-mandibular development, making the upper airway smaller and might lead to adult OSA. Surgery in young children should be performed as early as possible to prevent the resulting morphologic changes and neurobehavioral, cardiovascular, endocrine, and metabolic complications. Close postoperative follow-up to monitor for residual disease is equally important. As the proportion of obese children has been increasing recently, parents should be informed about the weight gain after T&A. Multidisciplinary evaluation of the anatomic abnormalities in children with OSA leads to better overall treatment outcome.
Introduction
Obstructive sleep apnea (OSA), alternative name sleep-disordered breathing (SDB), refers to a group of respiratory conditions that are exacerbated during sleep due to increased upper airway resistance, disruption of ventilation, and sleep discontinuity1, 2). Contemporary descriptions of the condition begin with the report of Guilleminault3) in 1976 on 8 children with OSA accompanied by additional symptoms, such as hypertension, hyperactivity, and daytime somnolence, which have contributed to the present understanding that the clinical manifestations and treatments for OSA are substantially different in children compared with adults.
The overall prevalence of parent-reported snoring, by any definition, in a meta-analysis was 7.45%4). Although the definition and measurement of OSA vary, a recent review of literature4) suggested the prevalence of OSA from 0.1% to 13%, and most studies report 1% to 4% diagnosed by varying criteria on diagnostic studies. Korean research reported that 4.3% of elementary school children snore almost every day5), and the prevalence of habitual snoring (>3 per week) was 7.1% among elementary school children6), and the prevalence of habitual snoring and OSA among high school children is 11.2% and 0.9% respectively7). OSA occurs at all ages, with the peak prevalence from 2 to 8 years of age, when tonsils and adenoids are largest in relation to the upper airway size1, 2 ,8). If unrecognized and untreated, OSAS can lead to neurobehavioral, growth, and cardiovascular sequelae in childhood1, 2). Adenoidectomy and/or tonsillectomy (T&A) are most often performed as the first-line treatment in childhood OSA1, 2). While it is generally believed that T&A is successful in most cases, recent reports showed success rates that vary from 27.2% to 82.9%9-13). New treatment modalities have been described in the last few years for childhood SDB beyond T&A14-16). The purpose of this article is to summarize current knowledge on available treatments for OSA in children to improve pediatric OSA management.
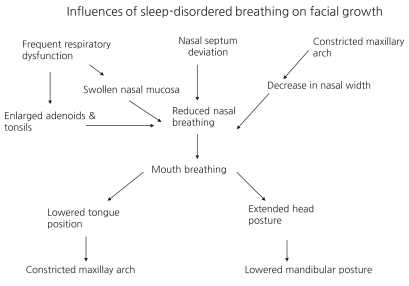
Craniofacial morphological changes secondary to upper airway obstruction
By the age of 4 years the craniofacial skeleton has attained 60% of adult size, and by the age of 12 years, it is 90% of adult size8). Craniofacial anomaly results from both genetic and environmental determinants. The observation of familial aggregates of SDB17, 18), and that an African American or Far Eastern origin is a risk factor for SDB, strongly suggests the importance of genes in linking the craniofacial skeleton and SDB19). However, environmental factors are also important determinants of craniofacial growth and development. Studies in monkeys and children have shown that upper airway obstruction with mouth breathing can induce craniofacial anomalies, which can be improved or normalized after SDB treatments such T&A20-22). Children who do not improve tend to have a narrower oropharyngeal airspace and mandibular retrognathia23, 24). SDB can induce craniofacial anomalies, which likely further increase the risk of SDB. This necessitates the early detection and treatment of SDB in children. It is suggested that continuation of SDB leads to worsening of the craniofacial pattern year by year25) (Fig. 1).
Treatment of OSA in Children
Treatment of OSA should include providing space for ventilation, improvement of cranio-facial growth, improvement all symptoms, and preventing the development of adult OSA.
Surgical Treatment
1. Adenoidectomy and Tonsillectomy
1) Indications for T&A
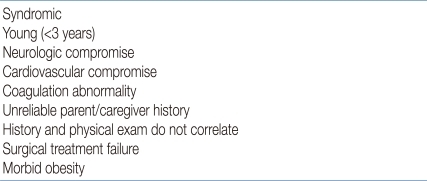
The indication for T&A in children with adenotonsillar hypertrophy is straightforward in the presence of OSA proven by polysomnography (PSG) or in snoring children with an abnormal, full-night pulse oxymetry recording1, 2, 26). The American Academy of Pediatrics (AAP) Clinical Practice Guidelines state that all children should be screened for snoring and recommended PSG as the gold standard for diagnosis of OSA because patient history and physical examination are poor discriminators of primary snoring and OSAS2). The prevalence of snoring was reported to be 6-12%, and the prevalence of OSAS was about 1-3%4). Testing 10% of children is a lot for PSG, but unnecessary surgery poses problems such as high cost and suffering in the patient. In a survey of the members of American Society of Pediatric Otolaryngology, only 10% of children undergoing T&A had PSG27). The recent guidelines2) that envisage the use of PSG as a reference method to differentiate primary snoring from OSAS are inapplicable in clinical practice due to cost of the test and the lack of laboratories that study sleep in the pediatric age group27, 28). Also, there is currently no definitive set of PSG criteria that will reliably discriminate those children who have OSAS and require treatment1, 2, 4, 28-32). Therefore, for otherwise healthy children with a history consistent with nighttime snoring; restless sleep; daytime symptoms including somnolence, behavior changes, and poor cognitive performance; and a physical exam consistent with adenotonsillar hypertrophy, with or without witnessed apnea, it is reasonable to proceed with T&A without prior PSG30, 31). Doubt in the diagnosis and being categorized as a high-risk individual for surgery are the most common indications for PSG28-30). Preoperative PSG is needed when the child has medical comorbidity, age <3 years, morbid obesity, small tonsils and adenoids, and history and physical findings that do not correlate with the degree of airway obstruction1, 2, 28-31) (Table 1).
T&A is generally accepted as the first-line treatment in associated medical conditions such as abnormal control of upper airway muscles, e.g., cerebral palsy, Down syndrome, and obesity, even in the absence of clear adenotonsillar hypertrophy. However, persistence or recurrence of snoring and SDB after T&A is also common in these conditions1, 2).
The PSG diagnosis of OSAS in children is defined as apnea hypopnea index (AHI) >1/h, according to the criteria of the American Academy of Sleep Medicine33), but there have been different criteria for childhood OSAS such as apnea index >1/h or AHI ≥1.5/h in several studies1, 2, 4, 34). This does not mean that every child with an AHI ≥1.5/h will benefit from treatment29-32). There is good consensus that moderate to severe PSG abnormality (AHI ≥5) should be treated with T&A1, 32, 35). However, for mild PSG abnormality, T&A is controversial and should depend on clinical symptoms and physical examination1, 2, 29-32).
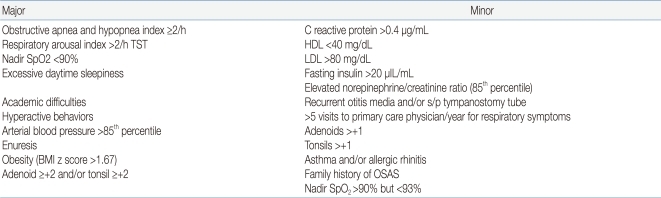
Gozal35, 36) suggested his criteria for diagnosis of pediatric OSA that requires treatment, like Jones criteria for the diagnosis of rheumatic fever, which included a combination approach of nocturnal PSG derived cut-off, and the presence of specific symptoms and measurable outcomes (biomarker, functional measures, etc.) (Table 2). It is not validated and revised continuously.
2) Age, when to treat
The age limit for T&A may be related to fear about more frequent upper airway infections and postoperative complications. Children under 3 years old had more postoperative complications1, 2, 28, 37).
OSAS occurs in children of all ages but peaks between 2 and 8 years, coinciding with the peak age of lymphoid hyperplasia8). Usually, children over 3 years or >15 kg could be operated without respiratory complications28). However, T&A can be performed in the presence of severe airway obstruction without any age restriction. Moreover, age is not a contraindication for T&A if OSA is present37, 38). Moreover, younger children under 3 years of age would have more severe OSAS, and surgery in younger children even with craniofacial abnormalities, syndromic features, and neurodevelopmental disorders had shown a more significant decrease in AHI after intervention than medical treatment38). This validates the safety and efficacy of surgical treatment in higher-acuity, young, tertiary-center patients with good respiratory investigation and support37-39).
3) Tonsillectomy or adenoidectomy, or both?
Both the tonsils and the adenoid should be removed, even if one or the other appears to be more enlarged, because OSAS is caused by both structural and neuromuscular abnormality and the treatment should widen the airway as much as possible1). There were anecdotal reports of the high persistence or recurrence of OSA if adenoidectomy or tonsillectomy alone was done instead of T&A1). Nieminen found improvement of OSA after tonsillectomy in 73% of children with previous adenoidectomy40). This suggests that adenoidectomy alone was insufficient. However, tonsillectomy alone is recommended for velopharyngeal incompetence such as submucous cleft palate1).
4) Outcome
The results of published data on success rate of T&A in curing OSA are highly variable, ranging from 24%10) to 100%11). A systematic review of all published series in 200611) reported an overall success rate of 82.9% for uncomplicated pediatric patients. In a recent meta-analysis of current literatures, the success rate was 66.3% when cure was defined as an AHI <113). In a recent multicenter retrospective study12), only 27.2% of children normalized their respiratory patterns during sleep as determined by the post-T&A PSG. Contrary to popular belief, these data demonstrate that pediatric sleep apnea is often not cured by T&A defined by PSG criteria, although there is a statistically significant AHI improvement in nearly all patients undergoing T&A11). High-risk groups of residual disease include patients with young or old age, morbid obesity, craniofacial syndrome, Down syndrome, neuromuscular disorders, and severe preoperative sleep apnea9-13). Preoperative AHI and BMI percentile are important factors that should be considered in the diagnosis and treatment plan of pediatric patients10, 12). Close postoperative follow-up to monitor for residual disease is important.
For long-term outcome, there also appeared to be increased risk of snoring and desaturation on PSG 12 years later in children treated for OSA25).
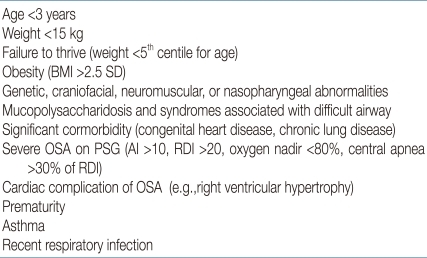
5) Risk of T&A, morbidity and mortality
T&A continues to be associated with significant morbidity. The perioperative complication rate was 8.8%, and the unplanned admission rate was 8.0%28). Mortality of T&A can be as low as 1 in 10,000-35,0001, 16). Acute general complications of T&A include hemorrhage, respiratory decompensation, anesthetic complication, pain, and poor oral intake. Postoperative hemorrhage has been reported in up to 3-8%, higher in older children, and return to surgery has been reported in 0.8% to 1.8% of patients28, 41). Respiratory complication is increased when T&A is undertaken for airway obstruction relative to other indications. Postoperative respiratory complications has been reported in 4.4-15.1% in overall T&A, increased up to 23-36% in routine OSA cases and 60% in urgently performed cases. These complications result from transient worsening of OSA secondary to postoperative edema and increased secretion, respiratory depression from anesthetic agents or the use of oxygen with a blunted hypoxic drive and the occurrence of postoperative pulmonary edema28, 42). The major risk factors for post-operative respiratory complications in children include young age (2-3 years), high preoperative AHI, low nadir oxygen saturation (<70-80%), and the presence of concurrent medical problems (obesity, prematurity, cerebral palsy) or craniofacial disorders (Table 3). T&A is currently performed as an outpatient day-surgery, but high-risk patients should be hospitalized for continuous cardiopulmonary/oxygen monitoring38). Continuous positive airway pressure (CPAP) can be used in the perioperative period to stabilize patients before T&A and to treat postoperative complications39, 41). Late complications of T&A may be nasopharyngeal stenosis and velopharyngeal incompetence. Velopharyngeal incompetence is transient, and mostly resolves with time1).
Tonsillotomy is less painful, but has a greater recurrence rate than tonsillectomy. Therefore, it should be avoided in SDB children with concomitant history of recurrent tonsillitis1).
2. Alternative Surgical Treatment
1) Other soft tissue reduction procedures
An example of such procedures is radiofrequency ablation of the tongue base, which is only rarely undertaken in children, such as those with Down syndrome or other causes of macroglossia.
(1) Septoplasty and turbinectomy
With the increasing understanding of the progression of allergic rhinitis to SBD and the interplay between nasal obstruction and facial mal-developmen, which further predisposes to OSA, maximizing nasal patency quickly and safely should be considered in children with SDB. Septoplasy or turbinectomy may improve nasal airflow in older children. Due to the impact on facial growth, concerns about violating cartilage growth centers in the septum, no direct treatment of nasal septum deviation can be performed in children, however, inferior turbinate reduction is another viable option in treatment of allergic rhinitis to improve nasal flow and decrease nasal resistance much faster than nasal steroidal medication in older children1, 15, 42).
(2) Uvulopalatopharyngoplasty (UVPP)
UVPP is a surgical procedure involving the excision of the uvula and posterior portion of the palate and tonsils, and trimming and reorientation of the tonsillar pillar. In adults, it has a success rate of approximately 50%. UVPP is not commonly performed in children, because most children with sleep apnea do not demonstrate the redundant tissue found in adults. UVPP is reserved for children with abnormal upper airway neuromuscular tone, such as those with cerebral palsy or Down syndrome, and in obese children with high Mallampati scores or redundant lateral pharyngeal tissue1, 43).
(3) Lingual tonsillectomy
Enlargement of lingual tonsils is increasingly being recognized as a cause of OSA , especially in Down syndrome, obese children, residual OSA after T&A44). In about 35%, previous T&A is associated with an increased risk of overgrowth of the lingual tonsils. Endoscopic-assisted coblation lingual tonsillectomy is an effective technique for the treatment of lingual tonsillar hypertrophy causing persistent OSA in some children. It is important to identify enlargement of the lingual tonsils as a cause of OSA because it is one of the surgically curable causes of OSA. Especially when symptom recurs after T&A, lingual tonsillar hypertrophy should be suspected45).
2) Craniofacial surgery
Craniofacial surgery is indicated in complex patients who do not tolerate CPAP or who would also benefit from the cosmetic effect of surgery, particularly those with craniofacial anomalies1).
3. Orthodontic treatment
An appropriate treatment of upper airway anatomic abnormalities must be achieved as early and as completely as possible. It is much easier to use orthodontic treatment in children than in adults46) (Fig. 2).
1) Rapid maxillary expansion (RME)
RME is an orthodontic procedure that uses a fixed appliances with expansion screw anchored on selected teeth, causing skeletal expansion of the upper jaw by application of orthopedic force to the midpalatal suture in maxillary widening46). The procedure consists of an active increase of the palatal transverse diameters by progressive opening of the midpalatal suture (1 mm/d) during 10-20 days, followed by a fixed retention time of 6-12 months. Eventually, its indication was extended to OSA in children with or without T&A47).
2) Mandibular distraction procedures and/or mandibular midline osteotomy
Distraction osteogenesis consists of slowly moving the mandible or midface in the direction desired by using a distraction device. It can be performed in children with severe micrognathia, including infants with Pierre Robin syndrome or hemifacial microsomia. Because the procedure take advantage of the rapid healing and capacity of growth in the pediatric skeleton, osteotomy with distraction of bone is widely accepted as the procedure of choice in the early management of airway obstruction caused by craniofacial disproportion48).
Medical therapies
1. Continuous positive airway pressure
Nasal positive airway pressure therapy to maintain upper airway patency is the main treatment of choice in adults with OSA. However, due to the different pathophysiology of childhood OSA, CPAP is reserved only for moderate to severe cases of OSA in children who are not eligible for T&A (noneligibility criteria includes neuromuscular diseases, obesity, severe bleeding tendency, craniofacial abnormality, idiopathic OSAS, and small tonsils and adenoids in adolescents)1, 2, 49). CPAP has also been prescribed for children whose SBD persisted despite T&A.
CPAP is not curative and often needs to be used indefinitely. Thus, compliance with long-term CPAP therapy is a major issue, and behavioral intervention is helpful50). The remaining significant problems are related to the lack of optimal equipment for young children and frequent difficulties with regard to initial adaptation to the nasal mask and compliance to treatment.
The most common side effects of CPAP use are nasal symptoms, including nasal congestion, rhinorrhea, dryness, and epistaxis, which are caused by the cooling and drying effect of CPAP, which, in turn, alters the nasal mucosa and impedes mucociliary clearance. Side effects, such as mask leak, skin irritation, and pressure sores, are generally mild and self-limited; however, the development of midface hypoplasia following prolonged use of nasal CPAP has been reported as a rare long-term complication1, 2, 51).
2. Antibiotics
Broad-spectrum antibiotics may offer temporary improvement52). However, the use of antibiotics does not seem to obviate the need for surgery in most cases with adenotonsillar hypertrophy.
3. Anti-inflammatory Therapies
Upper airway inflammation is an important component of SDB in children. Chronic snoring causes repetitive vibration of upper airway soft tissues, inducing mechanical stress resulting in upper airway inflammation. Moreover, chronic systemic inflammation with SDB may contribute to upper airway inflammation. Such understanding has generated new therapeutic concepts in children with SDB. Nasal corticosteroids exert lympholytic action to treat inflammation and upper airway edema53). Nasal fluticasone for 6 weeks significantly decreased both adenoid size and AHI53). In an open-labeled study, the leukotriene receptor antagonist montelukast was found to be clinically effective in reducing disease severity in children with mild OSA54). In a subsequent study, a combination of intranasal steroids and leukotriene modifier for 12 weeks was found to be useful in children with residual OSA after adenotonsillectomy55). However, there was no long-term follow-up result more than 12 weeks after discontinuation of the medication.
4. Weight Loss
Weight loss is recommended for all obese children1, 56). After T&A, even obese children with OSA will demonstrate increase in weight gain57). After treatment of OSA, initial severe OSA, obesity, and those with a positive family history of OSA, initial high BMI, and African-American race, Mallampati score, and have other anatomical abnormalities of upper airway confer an independent increased risk for recurrence or persistence of SDB after T&A9-13). This implies that good weight control is important after surgical treatment. Postoperative PSG and CPAP are frequently recommended after T&A in obese children. Bariatric surgery is an effective weight reduction treatment for morbidly obese adults and children with severe apnea who failed other treatments.
5. Oral Appliance
Tongue retraining or mandibular repositioning devices are widely used in adults with OSA to increase the oropharyngeal space, but most are cumbersome and poorly tolerated by children58).
6. Supplemental Oxygen
Supplemental oxygen abolishes desaturation episodes associated with OSA, but it does not treat the underlying obstruction and may worsen hypoventilation59). If supplemental oxygen is considered in SDB children with severe desaturation, it must be used for a few days only, while awaiting urgent T&A, and should be monitored for ETCO2.
7. Environmental Control
There is high prevalence of allergy in children with OSA. Passive smoking is associated with snoring. Thus avoidance of allergens and cigarette smoking would help. If allergic rhinitis coexists, nasal corticosteroid as well as decongestant and immunotherapy are of value1, 42).
Follow Up
All children should be reevaluated clinically after surgery. Significant improvement may occur soon after surgery and, traditionally, OSA improves 6-8 weeks after T&A28). Those with severe OSA preoperatively continue to have risk factors for persistent OSA and thus require postoperative PSG9, 10). Adenoidal recurrence may occur, especially in very young children. If children develop a recurrence of OSA symptoms, lateral PNS X-ray or direct visualization of the adenoid by endoscopy could check the adenoidal regrowth. Revision adenoidectomy is required. Adhesion and contraction of posterior pharyngeal wall were sometimes found1, 28).
Conclusion
OSA in children is a frequent disease with a 1-4% prevalence rate. It imposes significant morbidity, causing neurobehavioral, cardiovascular, and endocrine complications. The impairment of nasal breathing with increased nasal resistance has a well-documented negative impact on early childhood maxillomandibular development, making the upper airway smaller and might lead to adult OSA after puberty. Optimal diagnostic methods and criteria are still being defined.
T&A should be considered a first-line therapy. For the majority of children with OSA, T&A improved upper airway obstructive sign and symptoms, quality of life, and behavioral and cognition problems, and decreased polysomnographic abnormality. However, recent published data on the success rates of T&A in curing pediatric OSAS are highly variable. Close postoperative follow-up to monitor for residual disease is equally important. Parents should be informed about the weight gain after T&A, and reduction of body weight is considered primarily for obese children. Management with ongoing CPAP therapy and/or other surgical interventions and anti-inflammatory therapies are also considered. Initially for severe cases, multidisciplinary team approach is recommended to plan the optimal therapy.