Outcomes of small for gestational age micropremies depending on how young or how small they are
Article information
Abstract
Purpose
The outcomes of small for gestational age (SGA) infants especially in extremely low birth weight infants (ELBWIs) are controversial. This study evaluated the mortality and morbidity of ELBWIs, focusing on whether or not they were also SGA.
Methods
The medical records of 415 ELBWIs (birth weight <1,000 g), who were inborn and admitted to the Samsung Medical Center neonatal intensive care unit from January 2000 to December 2008, were reviewed retrospectively. Mortality and morbidities were compared by body size groups: very SGA (VSGA), birth weight ≤3rd percentile; SGA, 3rd to 10th percentile; and appropriate for gestational age (AGA) infants, >10th percentile for gestational age. For gestational subgroup analysis, groups were divided into infants with gestational age ≤24+6 weeks (subgroup I), 25+0 to 26+6 weeks (subgroup II), and ≥27+0 weeks (subgroup III).
Results
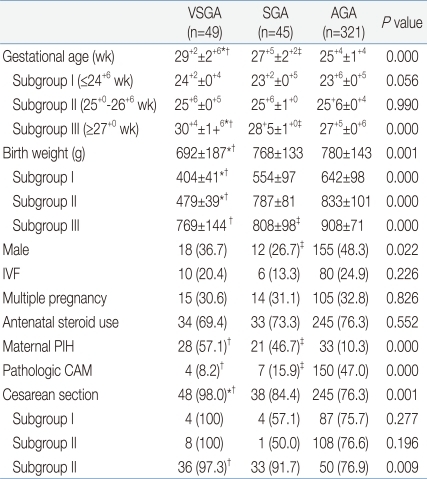
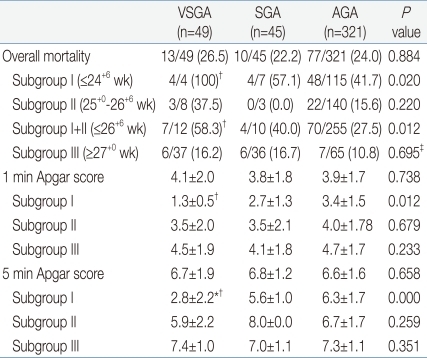
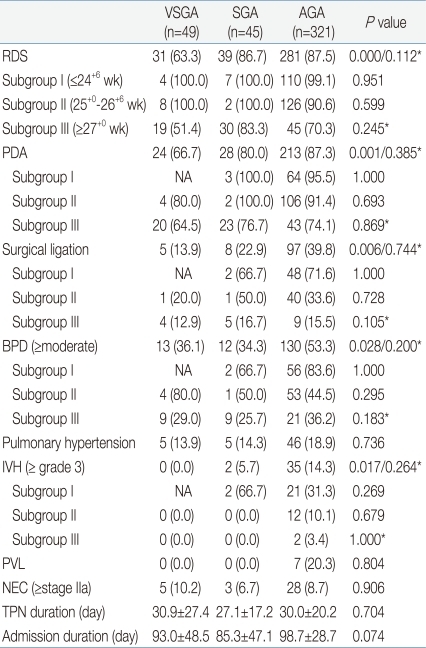
Gestational age was 29+2±2+6 weeks in the VSGA infants (n=49), 27+5±2+2 weeks in the SGA infants (n=45), and 25+4±1+4 weeks in AGA infants (n=321). Birth weight was 692±186.6 g, 768±132.9 g, and 780±142.5 g in the VSGA, SGA, and AGA groups, respectively. Cesarean section rate and maternal pregnancy-induced hypertension were more common in the VSGA and SGA than in AGA pregnancies. However, chorioamnionitis was more common in the AGA group. The mortalities of the lowest gestational group (subgroup I), and also of the lower gestational group (subgroup I+II) were significantly higher in the VSGA group than the SGA or AGA groups (P=0.020 and P=0.012, respectively). VSGA and SGA infants showed lower incidence in respiratory distress syndrome, ductal ligation, bronchopulmonary dysplasia, intraventricular hemorrhage than AGA group did. However, by multiple logistic regression analysis of each gestational subgroup, the differences were not significant.
Conclusion
Of ELBWIs, extremely SGA in the lower gestational subgroups, had an impact on mortality, which may provide information useful for prenatal counseling.
Introduction
With social and environmental changes including increased maternal age and advances in in vitro fertilization techniques, the risk of preterm birth has increased. Of all preterm births, the proportion of extremely low birth weight infants (ELBWIs) has been rising; for example, the birth rate of ELBWIs in Korea increased by 360% from 1993 to 20071,2). However, with the development of improved prenatal and neonatal intensive care unit (NICU) care, including antenatal steroids, surfactant, meticulous mechanical ventilation, infection control, and early aggressive nutrition, both mortality and morbidity in ELBWIs has been reduced. With improved survival of ELBWIs, factors influencing mortality and morbidity in micropremies become an issue of current importance.
In most preterm deliveries, small for gestational age (SGA) infants are generally associated with intrauterine growth restriction, which is caused by an inadequate supply of oxygen and nutrients that is attributable to placental insufficiency3-5). It is generally thought that the frequency of mortality and morbidity in SGA infants is much higher than that in non-SGA infants. However, most studies have not properly adjusted for the confounding effect of gestational age, and therefore, the effect of SGA on prognosis, especially in ELBWIs, is uncertain.
In this study, we evaluated the mortality and morbidity of ELBWIs focusing on whether or not the infants were SGA. We hypothesized that the prognosis for SGA ELBWIs would be different from appropriate for gestational age (AGA) ELBWIs, depending on the gestational subgroups and the severity of SGA.
Materials and methods
1. Subjects
This study was retrospective, involving 415 infants born with weight below 1,000 g and admitted to Samsung Medical Center NICU between January 2000 and December 2008. Among these infants, we excluded 1 infant with a gestational age of 21 weeks who died soon after birth. There were no cases of congenital anomalies, such as chromosomal abnormality or congenital infection.
For gestational subgroup analysis, infants of gestational age ≤24+6 weeks formed subgroup I, infants between 25+0 and 26+6 weeks formed subgroup II, and infants of gestational age≥27+0 weeks formed subgroup III. The number of infants in each subgroup was as good as equally distributed (subgroup I, n=126; subgroup II, n=151; subgroup III, n=138).
The parents consented to have their infants cared for in the NICU and enrolled in the study using retrospective chart review.
2. Methods
We reviewed maternal medical records for factors including multiple pregnancy, in vitro fertilization, maternal pregnancy-induced hypertension (PIH), pathologic chorioamnionitis (CAM), use of antenatal steroid, and mode of delivery. Also, we reviewed infants' medical records for gestational age, birth weight, sex, Apgar scores, mortality and morbidities such as respiratory distress syndrome (RDS), patent ductus arteriosus (PDA), ductal ligation, bronchopulmonary dysplasia (BPD), pulmonary hypertension, intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), necrotizing enterocolitis (NEC), duration of total parenteral nutrition, and admission duration.
Gestational age was calculated by last menstrual period, evaluated by early prenatal obstetric ultrasonography, and confirmed by modified Ballard Score examined within 12 hours after birth6,7). SGA was defined as birth weight under the 10th percentile for gestational age8). In this study, we defined very SGA (VSGA) as birth weight ≤3rd percentile for gestational age, and SGA was defined by a birth weight in the 3rd to 10th percentile for gestational age, thus the SGA group excluded VSGA infants. AGA infants had a birth weight in the 10th to 90th percentile for gestational age.
Neonatal mortality was defined as death before discharge. RDS was defined as respiratory distress needing oxygen over 40% to maintain PaO2 over 50 mmHg with radiological findings of air-bronchogram, decreased lung volume, and bilateral reticular infiltration. Because RDS can be assessed soon after birth, mortality cases were included in the count of RDS.
PDA was clinically diagnosed by symptoms and signs and confirmed by echocardiography. PDA was treated by indomethacin and/or surgical ligation. Surgery was done in cases of contraindications to indomethacin or failed indomethacin therapy. The definition and severity of BPD was investigated according to the criteria established by Jobe and Bancalari9). Moderate to severe BPD cases were considered significant. IVH was assessed by brain sonography10) and IVH ≥grade 3 cases were counted. PVL was evaluated by brain magnetic resonance imaging or sonography at post menstrual age 36 weeks or more. NEC was defined by modified Bell's criteria11) and stage ≥IIa was considered significant. Only survivors were included in the count of morbidities other than RDS.
3. Statistics
All analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were analyzed by χ2 test for a parametric test and Fisher's exact test for non-parametric test, and comparisons of continuous variables were conducted with one-way analysis of variance for a parametric test and Kruskal-Wallis test for a non-parametric test. P value <0.05 was considered statistically significant.
Multivariate logistic regression analyses were done to evaluate outcomes after adjusting for confounding factors. Factors significant in the univariate analysis were included in the initial model. The demographic variables of gestational age, maternal PIH, pathologic CAM, and mode of delivery were considered confounding factors. Each variable was assessed by each outcome. Interactions between variables were considered, and a stepwise selection was used for modeling. For the final models, goodness-of-fit test was done according to the Hosmer and Lemeshow method of multivariate analysis.
Results
1. Demographic characteristics
The average gestational age was 26+2±2+2 weeks (range, 23+0 to 34+4 weeks) and birth weight was 768±149 g (range, 350 to 999 g) in 415 ELBWIs. The number of VSGA, SGA, and AGA infants was 49 (11.8%), 45 (10.8%), and 321 (77.3%), respectively.
The proportion of VSGA or SGA infants did not significantly increase during the time period; however, the ratio of infants with lower gestational age did increase (P=0.026).
There were 126 patients in subgroup I (≤24+6 weeks), which was composed of 4 (3.2%) VSGA, 7 (5.6%) SGA, and 115 (91.3%) AGA infants. There were 151 patients in subgroup II (25+0 to 26+6 weeks) with 8 (5.3%) VSGA, 3 (2.0%) SGA, and 140 (92.7%) AGA infants. There were 138 patients in subgroup III (≥27+0 weeks) with 37 (26.8%) VSGA, 36 (26.1%) SGA, and 65 (47.1%) AGA infants.
Table 1 shows the demographic findings according to each body size group. Gestational age, birth weight, sex, maternal PIH, pathologic CAM, and delivery mode were significantly different between the VSGA, SGA, and AGA groups. Based on the result of the subgroup I and II analysis, there was no significant difference in gestational age that depended on body size. Subgroup III only showed significant difference in gestational age, depending on each body size group. Decreased male ratio in the SGA group was only significant in subgroup II (P=0.023). Maternal PIH and pathologic CAM were significantly different according to body size groups, even after being analyzed in gestational subgroups. The cesarean section rate was significantly increased only in subgroup III (P=0.009).
The etiologies of being small were investigated, and PIH was identified as a dominant factor in both the SGA (25/45, 55.6%) and VSGA (30/49, 61.2%) groups. In the SGA group, discordant twin, gestational diabetes in the mother, and advanced maternal age contributed to 22.2% (10/45). Other risk factors for being small included donors of twin-to-twin transfusion cases, 6.7% (3/45) and preterm labor with oligohydramnios (because of membrane rupture), 15.6% (7/45). In the VSGA group, factors leading to being small were discordant twin, placental anomaly, cord blood flow abnormality, maternal vascular disease, 26.5% (13/49), oligohydramnios with or without membrane rupture, 10% (5/49), and donor of twin to twin transfusion case, 2% (1/49).
2. Mortality rates
The total mortality rate in ELBWIs was 24.1% (100/415). The mortality rate in each of the VSGA, SGA, and AGA groups is described in Table 2, showing no significant difference in mortality rates according to the body size.
When analyzed by gestational subgroups, the mortality rate of subgroup I was 100% (4/4) in the VSGA group, resulting in a significant difference compared to AGA infants (P=0.020). In this lowest gestational age group, all the VSGA and SGA infant' mortalities occurred within 28 days of birth. In contrast, 67% (32/48) of mortality cases in the AGA group occurred after 28 days of age. The mortality in subgroup I VSGA infants was related to severe asphyxia in 3 cases, demonstrated by significantly lower 1 minute and 5 minutes Apgar scores. One of the mortality cases in this group was a donor in twin-to-twin transfusion syndrome, with intractable seizures because of massive brain hemorrhage soon after birth. Causes of death among subgroup I SGA infants included air leak, hemorrhagic shock, bowel perforation with shock, and septic shock with disseminated intravscular coagulopathy. The main causes of death in AGA infants were septic shock (18 cases) and cor pulmonale (13 cases) after 28 days of age.
The mortality in subgroup II was higher in the VSGA than in SGA or AGA group, however, there was no statistical significance. Subgroup II had only 3 mortality cases in the VSGA group. Causes of death were severe asphyxia, air leak, and bowel perforation with NEC, and all death were within 28 days of birth. The main causes of death in subgroup II AGA infants were not different from subgroup I.
Because the number of VSGA and SGA cases in subgroup II was small, the statistics of infants in subgroup I and II were assessed together. VSGA infants with gestational age <27 weeks (subgroup I+II) showed significantly increased mortality compared to AGA infants with gestational age <27 weeks (P=0.012).
The mortality rate in subgroup III was not different in the VSGA, SGA, and AGA groups after adjusting a confounding factor, gestational ages.
3. Morbidities
The VSGA group showed a significantly lower incidence of RDS, symptomatic PDA, ductal ligation, BPD (≥moderate), and IVH (≥grade 3) than the non-SGA group. However, by gestational subgroup analysis, the difference was not significant especially in subgroup I and II. In subgroup III, VSGA infants had lower RDS frequency than SGA or AGA infants (P<0.05) by univariate analysis. However, the RDS frequency in subgroup III VSGA infants was offset after adjusting confounding factors using multiple logistic regression analysis. Morbidities other than RDS in subgroup III were also evaluated after adjusting for gestational age, resulting in no statistically significant difference between the body size groups (Table 3).
Discussion
This study examined the effect of small for gestational age on mortality and morbidity in ELBWIs. The prognosis of preterm SGA infants, especially ELBWIs, is controversial because there are few studies of preterm SGA infants, and most of the outcomes have been confounded by varying gestational age and different populations. This retrospective study covering nine years was done in a single center, which is one of the largest NICUs in Korea. The ratio of ELBW SGA infants and the outcomes according to gestational age were not significantly different during the period, although the proportion of infants with lower gestational age has increased.
ELBW SGA infants seem to have a similar pathogenesis of being small, which is distinct from term or near term SGA infants who may have other etiologies of growth restriction. ELBW SGA infants were more likely to be born from PIH mothers. The pathogeneses of being small, maternal vascular disease, cord blood flow abnormality, placental anomaly, smaller placenta of discordant twins are all similar to PIH because they can cause 'placental insufficiency'. In this study, the etiologies causing 'placental insufficiency' were present in 78% of SGA and 88% of VSGA groups. In contrast, ELBW AGA infants were more likely to be born from mothers with CAM mainly after preterm premature rupture of membranes. Thus, SGA and AGA preterm infants may experience different in utero environments. Different intrauterine fetal exposures can influence mortality and morbiditiy in ELBWIs. Infants exposed to placental insufficiency may have experienced chronic hypoxia and nutritional problems in utero12), while, infants exposed to CAM with or without oligohydramnios may have experienced congenital infections and conditions unfavorable for lung development. Which of the two conditions is more influential in determining the outcome is uncertain. In this study, PIH or CAM alone was not a confounding factor for overall mortality or morbidity.
In this study population, SGA infants were analyzed by SGA severity. The study showed that overall survival of VSGA, SGA, and AGA infants was similar. However, in subgroup I, the VSGA infants showed significantly higher mortality compared to AGA infants. Asphyxia was the main cause of death in the subgroup I VSGA infants, consistent with significantly lower Apgar scores in this group. It follows that the smaller the baby, the more their birth condition is an immediate extension of the in utero conditions. The mortality cases in the SGA and VSGA groups occurred in the early hours and days following birth, in contrast to those in the AGA group. Thrombocytopenia or neutropenia can occur in SGA infants as a result of chronic hypoxic stress in utero12). Thus, VSGA or SGA infants are particularly vulnerable to bleeding with thrombocytopenia or infection associated with neutropenia especially early after birth. Initial complete blood count examinations showed that thrombocytopenia was present in 50% of subgroup I VSGA and SGA infants, compared to 9% of AGA infants (data not shown). Neutropenia was observed in 63% of subgroup I VSGA and SGA infants, compared to 13% of AGA infants (data not shown). Although there was no statistical significance, a high rate of thrombocytopenia or neutropenia may place VSGA and SGA groups at increased risk just after birth.
The most serious morbidities that led to mortality were pulmonary hypertension (r2=0.606, P=0.000) and NEC (r2=0.511, P=0.000) in the study population. However, SGA status was not related to pulmonary hypertension or NEC even after the subgroup analysis was adjusted for gestational age. Khemani et al.13) reported that severe pulmonary hypertension is involved in a high proportion of SGA infants and SGA with pulmonary hypertension was associated with worse outcomes from a 9-year study. However, the relationship between pulmonary hypertension and SGA status is uncertain, and in an experimental study, chronic hypoxia in utero did not induce pulmonary hypertension or precocious muscularization of the precapillary unit directly14). This implies that lung condition, including BPD severity, may have an impact on pulmonary hypertension independent of SGA status.
Our result regarding NEC are inconsistent with some studies15,16), but Bardin et al.17) and Regev et al.18), in agreement with our findings, showed no significant difference in the rate of NEC in SGA and AGA infants born before 27 weeks. Intrauterine growth restriction which is related to SGA status, is known as a risk factor for NEC following intestinal ischemia due to placental insufficiency19-21). In our study population, the incidence of NEC was 14% in subgroup I and 8% in subgroup II which was relatively low. At this incidence, a larger study sample would be required to reliably determine the impact of SGA on NEC.
RDS was decreased in the subgroup III VSGA group. Other studies report that the incidence of RDS is decreased in SGA infants due to accelerated lung maturation related to the stressful intrauterine environment22,23). On the contrary, other studies report that placental insufficiency do not accelerate lung maturation but worsens respiratory outcome because these infants are exposed to "oxidative stress," resulting in lung damage rather than lung maturation24). An analysis adjusted for gestational age revealed that the RDS rate in subgroup III was not significantly different according to body sizes.
This study showed that the rate of BPD (≥moderate) was not significantly different depending on body size, after adjusting for gestational age. The prevalence of BPD in SGA infants is important in terms of long-term neurological outcome. There are some data suggesting that there are higher BPD rates in preterm SGA infants with longer ventilator duration and hospital stay than in AGA infants, which implies poorer neurologic outcomes in preterm SGA infants22,25). However, our data showed that SGA or VSGA infants did not have increased risks of BPD or a longer hospital stay. Considering that some infants in AGA group were deceased with cor pulmonale, the effect of being small on BPD can be decreased more.
The rate of symptomatic PDA and ductal ligation was not significantly different according to body size according to a multivariate analysis. The effect of being small on PDA is also controversial. Several studies have suggested that maternal PIH may reduce the risk of symptomatic PDA because mothers with PIH are likely to deliver before labor and thus, have a low possibility of prostaglandin exposure which is known to be important for ductal patency26). PDA incidence is mainly influenced by gestational age and the development of RDS27). A report suggested that intrauterine inflammation can influence ductal patency28). Therefore, the rate of PDA in SGA infants may be confounded by gestational age, RDS, and CAM. In our study, we used multivariate analysis to exclude such variants was done, and SGA status did not significantly influence the rate of PDA and ductal ligation.
The incidence of IVH in SGA infants is also controversial. Some studies have reported that the incidence of IVH is decreased in SGA infants from PIH mothers, suggesting that pre-exposure to hypoxia may induce adaptive mechanisms, with fetal cerebral blood flow modulated by prostanoids in utero29,30). Meanwhile, several reports have shown that intrauterine inflammation is associated with IVH in preterm infants, suggesting a higher chance of IVH in AGA infants with CAM31,32). However, the Vermont Oxford Network study reported that there was a trend toward an association of SGA with increased risks of IVH16). IVH incidence was not different between SGA and AGA infants in another population study18). In this study, being small did not affect the rate of IVH, after adjusting for gestational age.
This study has a few limitations due to some missing infants whose birth weight might be over 1,000 g while gestational age at birth could be in the range of subgroup III. Thus, no significant difference in mortality and morbidity according to body size in subgroup III is inconclusive. However, the mortality difference according to body size with a summation of subgroup I and II, can be a useful information in the perinatal medicine. Getting information of micropremies below 27 weeks of age at birth, is now available due to advanced neonatal intensive care medicine. The number of SGA infants below 27 weeks of gestation is usually not enough for the investigation, though. Thus, survived SGA infants of lower gestational age should be more investigated for the understanding of morbidity outcomes.