Complications of nephrotic syndrome
Article information
Abstract
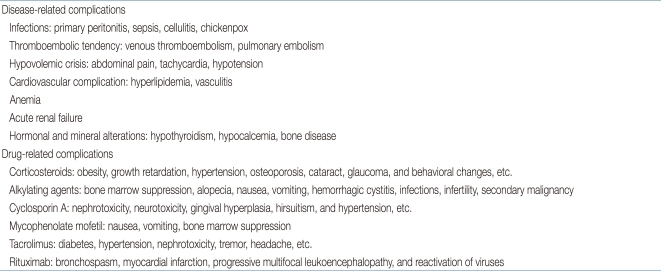
Nephrotic syndrome (NS) is one of the most common glomerular diseases that affect children. Renal histology reveals the presence of minimal change nephrotic syndrome (MCNS) in more than 80% of these patients. Most patients with MCNS have favorable outcomes without complications. However, a few of these children have lesions of focal segmental glomerulosclerosis, suffer from severe and prolonged proteinuria, and are at high risk for complications. Complications of NS are divided into two categories: disease-associated and drug-related complications. Disease-associated complications include infections (e.g., peritonitis, sepsis, cellulitis, and chicken pox), thromboembolism (e.g., venous thromboembolism and pulmonary embolism), hypovolemic crisis (e.g., abdominal pain, tachycardia, and hypotension), cardiovascular problems (e.g., hyperlipidemia), acute renal failure, anemia, and others (e.g., hypothyroidism, hypocalcemia, bone disease, and intussusception). The main pathomechanism of disease-associated complications originates from the large loss of plasma proteins in the urine of nephrotic children. The majority of children with MCNS who respond to treatment with corticosteroids or cytotoxic agents have smaller and milder complications than those with steroid-resistant NS. Corticosteroids, alkylating agents, cyclosporin A, and mycophenolate mofetil have often been used to treat NS, and these drugs have treatment-related complications. Early detection and appropriate treatment of these complications will improve outcomes for patients with NS.
Introduction
Nephrotic syndrome (NS) is classically defined as massive proteinuria (>40 mg/m2/hr), hypoalbuminemia (<2.5 g/dL), generalized edema, and hyperlipidemia in most cases1). The majority of nephrotic children have minimal change lesions, and these will either remit spontaneously within three years (two-thirds of the cases) or have earlier remission without complications following treatment with corticosteroids (CS) or cytotoxic agents (95%)2). However, the minority of children who have lesions of focal segmental glomerulosclerosis and severe and prolonged proteinuria are at high risk for complications. In these children, full nephrotic syndrome may progress to renal failure and even to dialysis, ultimately requiring renal transplantation.
Complications in NS may occur as a part of the disease itself or as a consequence of drug treatment. The loss of plasma proteins in the urine causes complications of NS as a direct result of the changing protein concentrations in the plasma or as a secondary result of altered cellular function3). Disease-associated complications include infections, thromboembolism, cardiovascular disease, hypovolemic crisis, anemia, and acute renal failure. CS, alkylating agents, calcineurin inhibitors, and mycophenolate mofetil (MMF) are usually related to the complications of long-term therapy in nephrotic children. Here, we focus on the complications occurring in children with NS (Table 1).
Nephrotic syndrome-related complications
1. Infections
Patients with NS are at increased risk for infections. Although the incidence of infections in NS has decreased in advanced countries, they are still a major problem in developing countries4).
Sepsis remains one of the main causes of death in children with NS5). Children treated with cytotoxic drugs have a higher clinical infection rate than those treated only with prednisolone6). In children with NS, Streptococcus pneumoniae is known to be the most important organism in primary peritonitis. However, other organisms such as β-hemolytic streptococci, Haemophilus and Gram-negative bacteria are also frequently found7). Cellulitis is also the result of β-hemolytic streptococci or a variety of Gram-negative bacteria.
Several immunological factors such as low serum immunoglobulin G concentrations, factor B and factor I in the alternative pathway components, transferrin, depressed T-cell function, and physiological factors such as fluid collection in cavities and dilution of local humoral defenses by edema may play a major role in the susceptibility of nephrotic patients to infection8).
Pneumococcal vaccines against capsular antigens is recommended for all children with NS9), but vaccination should be administered when the treatment with high doses of CS or with cytotoxic therapy is discontinued. Nephrotic children taking high-dose CS or other immunosuppressive agents within three months of their use are at risk of varicella infection, requiring varicella zoster immunoglobulin treatment within 72 hours of exposure and intravenous acyclovir during active varicella zoster infection10).
2. Thromboembolism
NS is a well-known risk factor for arterial or venous thromboembolism (TE), and patients with severe proteinuria have a 3.4-fold higher risk of venous TE11). It is also known that there is higher risk of TE in steroid-resistant NS than in steroid-sensitive NS12).
Thrombosis may arise in NS from loss of proteins involved in the inhibition of systemic hemostasis, increased synthesis of prothrombotic factors or by local activation of the glomerular hemostasis system13). The predisposing factors of TE in NS are as follows14,15): 1) abnormalities in platelet activation and aggregation, 2) activation of the coagulation system; increased synthesis of factors V, VII, VIII, X, von Willebrand factor, fibrinogen, and α2-macroglobulin accumulation, 3) decreased endogenous anticoagulants; antithrombin III, protein C, protein S, and tissue factor pathway inhibitor, 4) decreased activity of fibrinolytic system; plasminogen, the precursor for plasmin, and the imbalance of two major regulators of plasmin formation, plasminogen activator inhibitor-1 and tissue plasminogen activator16), 5) changes in the glomerular hemostatic system, 6) intravascular volume depletion, and 7) exposure to CS and diuretics17,18).
Doing arterial punctures should be avoided in nephrotic children due to the risk of arterial thrombosis. Gross hematuria with or without acute renal failure may suggest renal vein thrombosis in nephrotic children, which needs Doppler ultrasonography or magnetic resonance angiography19). Particularly, when nephrotic patients appear to have tachypnea and dyspnea, we should keep in mind the high probability of pulmonary embolism and perform ventilation-perfusion lung scanning or pulmonary angiography immediately20).
3. Cardiovascular complications
An increased risk of cardiovascular disease exists in patients with NS because of hyperlipidemia, increased thrombogenesis, and endothelial dysfunction21). Hypercholesterolemia is strongly associated with severity of hypoalbuminemia, and persistent proteinuria or renal insufficiency also contributes to cardiovascular disease22).
There is little or no risk of cardiovascular disease in children with MCNS who are responsive to CS because hyperlipidemia is intermittent and of short duration. The risk of premature atherosclerosis is increased due to hyperlipidemia. The duration of nephrotic hyperlipidemia appears to be critical to initiating vascular damage, and patients with unremitting proteinuria and hypoalbuminemia are the most at risk23).
Very low-density lipoprotein (VLDL), low-density lipoprotein (LDL) and lipoprotein (a) are elevated in children with long-standing and frequently relapsing NS21). Elevated VLDL and LDL should place patients at increased risk for developing atherosclerosis. Hyperlipidemia contributes to the development of glomerular and interstitial renal disease. Endothelial damage from hyperlipidemia may favor influx of lipoprotein into the mesangium, leading to proliferation and sclerosis22).
Therapy with lipid-lowering drugs, hydroxymethylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, should be given with extreme caution in children as it remains controversial. Although Prescott et al.24) reported that lowering cholesterol levels during childhood might reduce the risk for atherosclerotic changes and suggested short-term safety and efficacy of HMG-CoA reductase inhibitors, others showed that excessive free lipid-lowering drugs with low albumin levels may affect proximal muscle pain and malaise even at a normal dose25,26). Therefore, more prospective controlled studies in children are needed in the future to evaluate the efficacy and safety of lipid-lowering drugs.
4. Hypovolemic crisis
Hypovolemic shock is one of the attentive presentations in NS27). Risk factors for hypovolemic crisis include severely depressed albumin levels, high dose diuretics, and vomiting. The clinical manifestations are tachycardia, cold extremities, poor capillary refill, and moderate to severe abdominal pain, and laboratory tests may show elevated hematocrit and uric acid levels.
It is useful to measure urinary sodium (UNa) excretion or fractional excretion of sodium (FENa) when evaluating physical volume status. Donckerwolcke et al.28) found a better correlation between log aldosterone and urinary potassium / urinary potassium + urinary sodium (UK / UNa + UK) ratio than with other parameters measuring renal potassium and sodium handling. In patients with renal sodium retention (FENa: <0.5%), UK / UNa + UK ratio of higher than 0.6 (UK / UNa + UK: >60%) identifies patients with increased aldosterone levels and functional hypovolemia29).
This index may therefore be used to assess which patients will benefit from intravenous normal saline (20 mL/kg over 1 to 2 hours) or albumin administration at maximum dose of 1 g/kg over 3 to 5 hours with blood pressure monitoring29). The administration of albumin is not routinely given to all patients in relapse and may be dangerous in children who are not volume depleted due to the risk of pulmonary edema.
5. Anemia
Mild anemia is observed on occasion in patients with NS. Anemia is usually microcytic and hypochromic, typical of iron deficiency, but is resistant to therapy with iron because of large loss of serum transferrin in the urine of some nephrotic patients30). Vaziri31) reported some data on the metabolism and regulation of erythropoietin (EPO) and transferrin, which are essential for erythropoiesis in nephrotic children.
Urinary loss of EPO causes EPO-deficiency anemia and transferrinuria, and increased transferrin catabolism induces hypotranferrinemia and iron-deficiency anemia in some cases. Subcutaneous administration of recombinant EPO and iron supplementation can be used for the treatment of EPO- and iron-deficiency anemia, respectively32). However, correction of the underlying proteinuria will be the ideal approach to reversing these complications.
6. Acute renal failure
Acute renal failure (ARF) is an uncommon but alarming complication of NS33). When massive proteinuria develops and the levels of albumin are profoundly decreased, the circulating volume in the plasma is reduced to produce circulatory collapse or pre-renal uremia, usually of mild degree. However, much less commonly, ARF that is unresponsive to volume replacement and aggressive diuretic therapy may be seen in certain forms of NS without the features of volume depletion. This may be due to severe disturbance in visceral epithelial cells that results in almost total obliteration of the slit pores and severe reduction in surface area for filtration34). With severe proteinuria, occlusion of the distal nephron lumina from cast formation or extratubule compression from renal interstitial edema may result in an increase in proximal tubular pressure, leading to a fall in glomerular filtration rate35).
ARF is usually precipitated by sepsis, radiocontrast agents, acute tubular necrosis from nephrotoxic antibiotics and non-steroidal anti-inflammatory agents. If renal failure persists for more than a few days, dialysis may be necessary for complete recovery.
7. Edema
Edema is often observed in nephrotic children and where tissue pressure is low. Ascites and pleural effusions frequently occur, but pericardial effusion is rare unless cardiac function is abnormal. Edema is caused by increased glomerular permeability and hypoalbuminemia, resulting in decreased plasma oncotic pressure and functional hypovolemia. These stimulate secondary sodium retention by the kidney36).
Treatment of edema consists of dietary sodium restriction and judicious use of loop-acting diuretics such as furosemide and bumetanide. Hyperoncotic salt-poor albumin and furosemide may be administered in cases of severe and refractory edema36).
8. Hormonal, mineral alterations and intussusceptions
Urinary loss of hormone-binding proteins contributes to various hormonal abnormalities in patients with NS. While thyroid function tests are in the normal range in most nephrotic patients, the mean values for triiodothyronine (T3) and thyroid-binding globulin (TBG) are lower than those in non-NS children because of a significant increase in urinary excretion of T3, T4 and TBG37). Routine thyroid screening and early replacement therapy of thyroid hormone are necessary for infants with severe NS and clinical hypothyroidism.
Hypocalcemia in NS is also attributed to the decreased albumin level, which results in reduced bound and ionized calcium in 50 to 80% of NS cases38). Children with NS often have hypocalciuria due to decreased gastrointestinal absorption of calcium and increased renal tubular reabsorption of calcium. These suggest the possibility of an abnormality in vitamin D metabolism. The abnormalities are due to increased filtration of vitamin D metabolites bound to vitamin D-binding globulin39). However, bone disease is rarely shown in NS patients, and therefore, routine treatment with vitamin D is not recommended. Nevertheless, special concern should be given to subclinical mineral bone disorder like secondary hyperparathyroidism.
Intussusceptions can occur within the ileocolic junction and the small intestines in patients with NS, causing acute abdominal pain. They are caused by a combination of patches of bowel wall edema and peristaltic incoordination. Cho et al.40) reported a case involving reversal of intussusceptions associated with nephrotic syndrome by infusion of albumin.
Adverse effects of long-term drug therapy
1. Corticosteroids
CS have reduced the NS mortality rate to around 3%41). However, CS have well-recognized potentially serious adverse effects such as cushingoid features, obesity, growth retardation, hypertension, osteoporosis, cataracts, impaired glucose metabolism, dyslipidemia, emotional deprivation, behavioral changes, and avascular necrosis of the femoral head42).
Two major causes of growth retardation in patients with NS are the loss of insulin-like growth factors (IGFs) and/or IGF-binding proteins (IGFBPs) and CS therapy. Several reports have suggested that there are changes in serum levels of IGFs and IGFBPs among nephrotic children43,44). CS induce overt elevation of serum IGF-1 levels, which results in the potential development of IGF resistance, one of the main factors responsible for persistent growth retardation45). Bone maturation and linear growth are delayed and arrested by long-term, high-dose CS therapy46), particularly when the dosage exceeds 0.5 mg/kg/day47). Therefore, the initial dose should be low in the range of 0.2 to 0.4 mg/kg (5 to 15 mg/m2) per dose for treatment maintenance.
Jeon et al.48) reported that alternate-day steroid therapy, as a single morning dose, does not affect growth but may lead to decrement of serum vitamin D3 levels and bone mineral density in children with NS. The best way to avoid growth retardation is to stop unnecessarily extended courses of therapy with high doses of CS. To reduce the complications associated with CS therapy, the following strategies may be helpful:
Adrenal suppression: alternate-day steroid therapy.
Impairment of statural growth: CS-sparing agents, and growth hormone therapy.
Osteoporosis: Calcium, vitamin D supplementation, and use of steroid-sparing protocols.
Peptic ulceration: H2 blockers.
Hypertension: anti-hypertensive agents.
Cataract: low dose and short duration of CS treatment, regular examination by ophthalmologists.
Increased intracranial pressure: investigate papilledema.
Behavioral changes49): reduce or withdraw CS.
2. Cyclophosphamide (CPM)
Alkylating agents impair DNA transcription by attaching alkyl chains to purine bases. Latta et al.6) addressed the side effects of alkylating agents, including early complications of bone marrow suppression, alopecia, gastrointestinal upset, hemorrhagic cystitis, and infections, and late complications of possible malignancies and impaired fertility, especially in males. There is a dose-dependent relationship between sperm counts and the cumulative dose of CPM50). To avoid gonadal toxicity, CPM should not be used for more than 12 weeks (2 mg/kg, single oral dose) and should be withheld if the white blood cell count is less than 5,000/mm3 during CPM use. High fluid intake is recommended to elude hemorrhagic cystitis during the use of CPM.
3. Cyclosporin A (CsA)
CsA is an immunosuppressive fungal metabolite that acts by modifying T-cell function and inhibiting the release of interleukin-2 from activated T helper cells51). Long-term use of CsA causes reduced renal function, gingival hyperplasia, hirsuitism, hypertension, hyperkalemia, and encephalopathy52). CsA-induced tubulointerstitial lesions are found in 30 to 40% of children who have received CsA for more than 12 months53). Several publications have shown risk factors for CsA complications, such as the long duration of CsA treatment, a high CsA trough level, and a younger age at the start of CsA treatment54-56). Therefore, the lowest effective dose of CsA is recommended for the maintenance treatment in nephrotic children, with slow tapering over one year to 1 to 3 mg/kg/day. Yang et al.57) found that the combined treatment of CsA and MMF did not prevent the development of chronic CsA nephrotoxicity, but MMF treatment after CsA withdrawal improves chronic CsA nephrotoxicity. Recently, Hara et al.58) also reported protective effects of Mizoribine on CsA nephropathy in rats.
4. Others
Complications of MMF include gastrointestinal disturbances, bone marrow suppression, and headache, requiring dose reduction or even withdrawal59). Tacrolimus is a calcineurin inhibitor that has similar action to CsA but can have several side effects, such as hypertension, abnormal renal function, tremor, muscle cramps, hyperkalemia, hypophosphatemia, leukopenia, and hyperglycemia. Levamisole, the antihelminthic agent, can be used in steroid-dependent patients, but is ineffective as a permanent therapy for NS. Levamisole may have the minor side effects of leukopenia, gastrointestinal effects, and vasculitis, but no important side effects were reported60). Rituximab has recently been introduced and may be applied to steroid-dependent or refractory nephrotic syndrome61). Complicatons of Rituximab include life-threatening bronchospasm, myocardial infarction, progressive multifocal leukoencephalopathy, and reactivation of viruses such as cytomegalovirus and hepatitis B virus62).
Conclusions
The complications of the NS can be divided into two categories, disease-associated and treatment-related. When we treat children with NS, it is important to start with early identification and appropriate treatment for acute complications. Regular examinations and monitoring for chronic complications will improve outcomes for children with NS.