Dietary patterns and metabolic syndrome risk factors among adolescents
Article information
Abstract
Purpose
Unbalanced diets and decreased physical activity have contributed to increased prevalence of obesity and metabolic syndrome in adolescents. We have performed a systematic review and data analysis to examine the association between dietary pattern and metabolic syndrome risk factors in adolescents.
Methods
We searched the PubMed and BioMedLib databases for appropriate articles published during the past 10 years and selected 6 articles. The studies reviewed applied factor analysis or cluster analysis to extract dietary patterns. For data analysis, we examined the association between dietary patterns and the prevalence of metabolic syndrome risk factors using data of 3,168 adolescents (13 to 18 years) obtained from 4 consecutive Korean Nutrition Health and Nutrition Examination Surveys (1998, 2001, 2005, and 2007 to 2009).
Results
Our systematic review confirmed that western dietary patterns are positively associated with metabolic syndrome risk factors such as obesity and elevated triglycerides, while traditional dietary patterns were negatively associated. Data analysis found that the number of adolescents aged 16 to 18 years who had "Rice & Kimchi" dietary pattern decreased, while the number having western dietary patterns increased during the 1998 to 2009 time frame. There were no changes in the dietary patterns in adolescents aged 13 to 15 years. The risk of elevated serum triglycerides and reduced serum high density lipoprotein cholesterol was high in the "Rice & Kimchi" dietary pattern compared to the other dietary pattern groups.
Conclusion
Because adolescents' dietary patterns are changing continuously and have long-term effects, further studies on the dietary patterns of adolescents and their health effects into adulthood are necessary.
Introduction
Adolescence is a period of rapid body growth and cognitive development, requiring balanced and sufficient nutrient intake1). Since dietary habits are usually acquired in this period and could affect dietary practice in later life2), it is crucial for adolescents to acquire healthy dietary behaviors for long-term health. However, the prevalence of diet-related metabolic syndrome risks such as obesity, glucose intolerance, elevated blood pressure, and dyslipidemia is increasing worldwide due to unbalanced nutrient intake among adolescents3).
The prevalence of metabolic syndrome in United States adolescents was estimated as 9.2% in 1988 to 1994 National Health and Nutrition Examination Survey, and was almost 30% in overweight or obese adolescents4). In Korea, the overall prevalence of metabolic syndrome was 6.8% in the 1998 Korean National Health and Nutrition Examination Survey (KNHANES) and increased to 9.2% in the 2001 KNHANES5).
Although dietary behaviors are known to be associated with current and future health6), the compliance of adolescents to healthy dietary guidelines is low. For example, adolescents consume less fruits, vegetables, dairy products, and fish, but consume more sugar, refined grain, meat, and fat compared with recommended dietary guidelines7-9). According to the Korea Youth Risk Behavior Web-based Survey, the percentages of adolescents who consume vegetables, milk, carbonated drinks, or ramen more than 3 times per week are 17.6%, 13.7%, 52.9%, and 50.9%, respectively10).
Previous studies associating dietary factors with metabolic syndrome or its components have mainly focused on the intake level of a single nutrient or food, making it difficult to assess interactions among nutrients. Because a variety of foods are generally consumed together, providing a range of interacting nutrients in a diet, the assessment of dietary intakes based on a single nutrient or food is not helpful in detecting associations between overall diet quality and disease. Recently, dietary pattern analyses have been applied to examine the complex nature of dietary intake and explore the relationships with various health outcomes. Dietary pattern analyses can evaluate overall features of diet composition and help identify complex relationships, potential interactions, and antagonistic or synergistic effects between nutrient intake and disease.
In this study, we have performed a systematic review and data analysis to identify trends of dietary patterns and their association with metabolic syndrome risk factors in Korean adolescents.
Materials and methods
1. Literature selection for review
To identify articles that evaluated dietary patterns with regard to metabolic syndrome, we searched PubMed (http://www.ncbi.nlm.nih.gov/pubmed/) and BioMedLib (http://bmlsearch.com/) using combinations of the following terms: "factor analysis," "principal component analysis," "cluster analysis," "patterns," "diet," "food," "obesity," "metabolic syndrome," "adolescent," and "children." Potentially relevant papers were selected by screening titles and abstracts or entire articles (i.e., if abstracts were absent or provided limited information), and then evaluated to determine whether they met all the inclusion criteria, which were: 1) published in English in the last 10 years; 2) included a sample of adolescents; 3) included a dietary pattern analysis; and 4) analyzed the association between dietary pattern and metabolic syndrome or its components. Reports that addressed only overweight/obesity, metabolic disorders, or other diseases were excluded. Out of 101 potentially relevant articles from the search, 6 papers were selected for review.
2. Analysis of dietary pattern and metabolic syndrome risk factors
Samples were extracted from 4 waves of KNHANESs. The first survey was conducted in 1998, the second in 2001, the third in 2005, and the fourth in 2007 to 2009 by the Korean Ministry of Health and Welfare. Samples were composed of adolescents aged 13 to 18 years with a 24-hour dietary recall, blood analysis, and anthropometric data. The final analytic sample consisted of 3,168 respondents: 858 from the first survey, 842 from the second, 735 from the third, and 733 from the fourth.
Dietary patterns were identified by cluster analysis in which dietary data from a 24-hour recall were combined for each subject. Foods consumed by subjects were categorized into 23 groups based on common food groups classified in the Korean Nutrient Database. The percent of energy from each food group was used as an independent variable to avoid clustering around foods with the greatest volumes and to adjust for weight differences between solid and liquid foods. For ease of discussion, each dietary pattern was labeled with a descriptive name based on the predominant food groups.
Metabolic syndrome was defined using the pediatric International Diabetes Federation (IDF) criteria11). Waist circumference (≥90th percentile for waist reference data from the Korean Pediatric Growth Chart12) was a mandatory criterion. Two or more of the following components were also required: fasting triglycerides≥150 mg/dL (1.7 mmol/L), fasting glucose≥100 mg/dL (5.6 mmol/L), blood pressure≥130 mmHg systolic or ≥85 mmHg diastolic, and/or high density lipoprotein (HDL) cholesterol<40 mg/dL (1.03 mmol/L) for both sexes, except for HDL<50 mg/dL (1.29 mmol/L) for girls age≥16 years. Obesity was defined as a body mass index (BMI)≥95th percentile for age and sex. The reference values for BMI percentile were adapted from the Korean Pediatric Growth Chart12).
The chi-square test and logistic multiple regression models were used to assess secular trends of dietary patterns and their association with metabolic syndrome risks. All statistical analyses were conducted using SAS ver. 9.1 (SAS Institute Inc., Cary, NC, USA).
Results and discussion
1. The systematic review of the selected studies
The overall characteristics of the 6 studies reviewed in this study are presented in Table 1. The "Healthy" or "Health conscious" or "Fruit, salad, cereal, fish" patterns were negatively associated with risk of overweight/abdominal obesity or dyslipidemia or high blood pressure, whereas the subjects with "Western," "Snacking," or "Sweet" patterns had an increased risk of metabolic disorders. The results are consistent with previous studies for adult populations. The "Healthy pattern," rich in vegetables, grains, and dairy, characterized as a "balanced diet," was favorably associated with lowering risks for metabolic syndrome or its components in Tehrani middle-aged women13), in an adult population in Greece14), in Japanese young women15), and in middle-aged Koreans16).
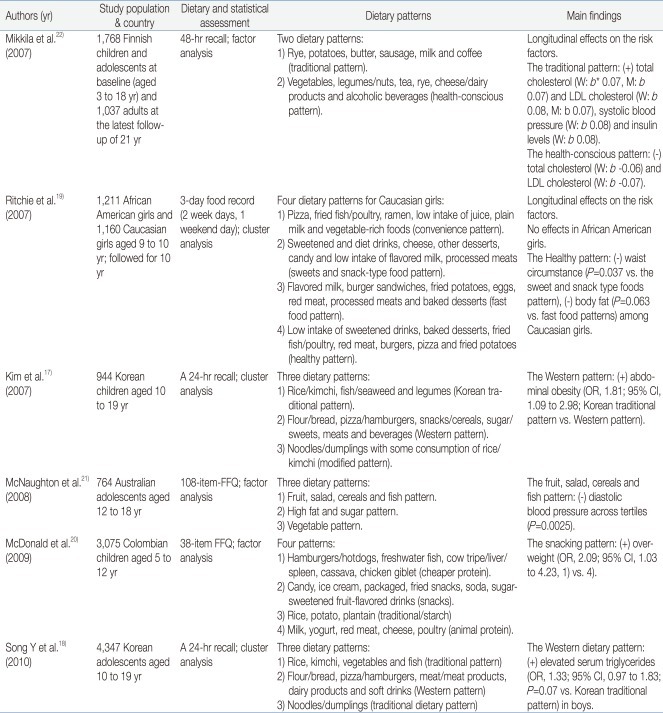
Previous Studies of Association between Dietary Patterns and Metabolic Syndrome Risk Factors in Children and Adolescents
This review included 2 reports addressing dietary patterns among Korean adolescents. Kim et al.17) identified the "Korean traditional," the "Modified," and the "Western" patterns among 1,271 adolescents aged 10 to 19 years from the 2001 KNHANES. Song et al.18) identified the "Modified," "Western," and "Traditional" patterns from 4,347 adolescents (1,572 from 1998; 1,484 from 2001; and 1,291 from 2005 KNHANES). The "Traditional" dietary pattern was characterized by a high intake of rice, kimchi, vegetables, and fish. The "Western" dietary pattern included high consumption of flour/bread, pizza/hamburgers, meat/meat products, dairy products, and soft drinks. The adolescents with "Western" patterns had 1.81 times higher risk of abdominal obesity (95% confidence interval [CI], 1.09 to 2.98)17) and 1.33 times higher risk of elevated serum triglycerides in boys (95% CI, 0.97 to 1.83; P=0.07)18) compared with the Korean "Traditional" pattern. Both studies used cluster analyses based on 24-hour recall data from KNHANES and identified similar dietary patterns and the association with obesity.
Similar results were also reported among American adolescent girls and Columbian children. Ritchie et al.19) identified 4 dietary patterns among American adolescent girls and termed "Convenience"; "Sweets and snack-type foods"; "Fast food"; and "Healthy." The "Healthy" pattern exhibited smaller mean values for waist circumference after a 10-year follow-up among African American girls. McDonald et al.20) found "Cheaper protein," "Snacking," "Traditional/starch," and "Animal protein" patterns among Columbian children and reported that the children with the highest "Snacking" pattern score had 2.09 times higher risk of being overweight (95% CI,1.03 to 4.23), as compared to those with the lowest pattern scores. Two other studies, in Finland and Australia, reported that healthy dietary patterns composed of a high consumption of vegetables, legumes, fruit, and dairy products were associated with reduced risk of high blood pressure21) and elevated total/low density lipoprotein cholesterol22), respectively.
The 6 studies included in our systematic review adopted different statistical methods for identifying dietary patterns: 3 used factor analyses and 3 used cluster analyses. Factor analysis is a method that extracts factors from a set of variables, which is similar to principal component analysis in terms of reducing dimensionality of multi-variables. Cluster analysis formulates clusters based on similarities among the variables to increase data interpretability23). Thus, selecting the appropriate analytical method depends on the purpose of the study. The dietary information used in the selected studies came from various methods such as 24-hour recall, diet records, and food frequency questionnaires (FFQ). The dietary intake of individuals usually has large daily variations, which can result in the misclassification of subjects. To elucidate the association between dietary factors and health outcomes, including metabolic syndrome risks, dietary information should be representative of usual intake. Most epidemiological studies adopt the FFQ method because of ease and feasibility; however, results from FFQ have limited in use due to the low accuracy of quantitative intake estimates. For accurate quantitative analysis of dietary intake, it is necessary to employ accurate and comprehensive open-ended survey methods such as multiple days of 24-hour recall and dietary records.
Dietary pattern analysis is useful in examining the diet-disease associations because dietary patterns reflect actual dietary practices. In addition, dietary patterns are easy to interpret and helpful in explaining diet-disease associations, and can provide information for dietary guidelines. However, interpretation of dietary patterns should proceed with caution because subjective judgments by a researcher can influence identification of the dietary pattern and the association with health outcomes. In order to extract dietary patterns, various factors, including the number of clusters, the grouping methods of food, and the selection of variables being analyzed (such as consumption frequency, intake amount, and % energy contribution) should be determined by researchers. Statistical analyses do most of the work, but researchers make the final choice. These decisions can impose bias and cause low reproducibility of the results. Nevertheless, recent dietary pattern studies have produced similar dietary patterns from study populations with similar periods, ages and regions15,24).
2. Trends in dietary patterns and their association with metabolic syndrome in Korean adolescents
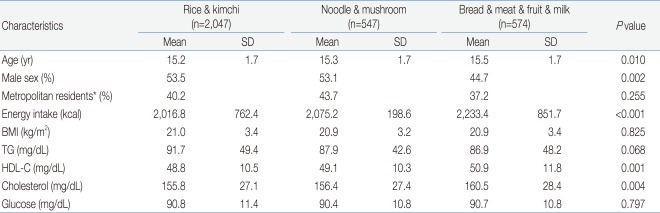
We derived 3 dietary patterns using the dietary intake data from 3,168 Korean adolescents described in 4 waves of KNHANESs. The "Rice & Kimchi" pattern, which is similar to a traditional dietary pattern and accounting for 64.6% of study participants (n=2,047), was featured high consumption of white rice, kimchi, beans, vegetables, and fish. The "Bread & Meat & Fruit & Milk" pattern, which is similar to western dietary pattern and accounting for 18.1% of participants (n=574), was characterized by high intake of grain, flour, bread, pizza, hamburgers, snacks, sugar, candy, meat and meat products, fruit, milk, and dairy products. Lastly, the "Noodle & Mushroom" pattern, accounting for 17.3% (n=547), had intermediate diet features that ranged between the "Rice & Kimchi" and "Bread & Meat & Fruit & Milk" patterns and is similar to a modified dietary pattern (Table 2).
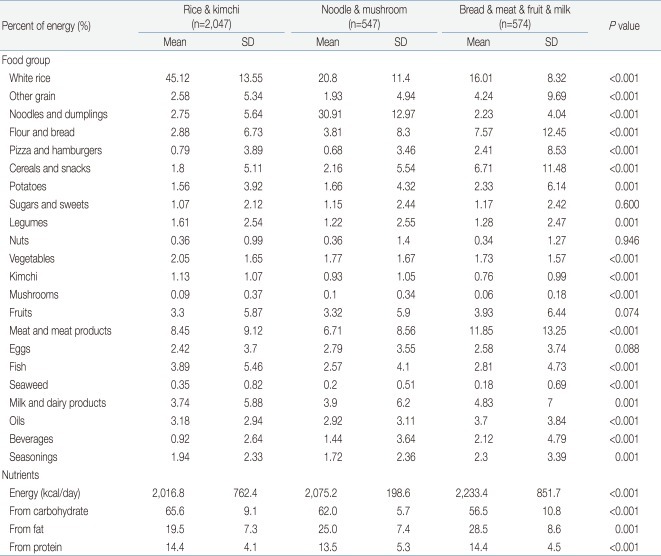
Percent Energy Intakes from Each Food Group and Nutrient Intakes by Dietary Patterns among Korean Adolescents
The percentages of males in the "Rice & Kimchi," "Noodle & Mushroom," and "Bread & Meat & Fruit & Milk" dietary patterns were 53.5%, 53.1%, and 44.7%, respectively. The number of metropolitan residents in the "Noodle & Mushroom" pattern (43.7%) tended to be high, but there were no significant differences across the dietary patterns. The subjects with the "Bread & Meat & Fruit & Milk" pattern had higher mean HDL cholesterol (50.95 mg/dL, P=0.001) and total cholesterol (160.5 mg/dL, P=0.004) levels compared to the subjects with "Rice & Kimchi" and "Noodle & Mushroom" dietary patterns (Table 3).
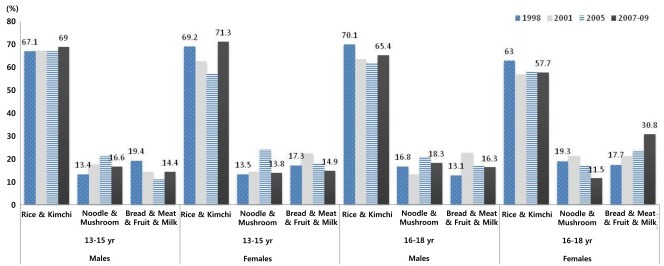
Secular changes in dietary patterns by age and gender are displayed in Fig. 1. There were differences in trend between age groups (13 to 15 years vs. 16 to 18 years). Among males aged 13 to 15 years, there were no changes in the proportion of the "Rice & Kimchi" pattern; however, the proportion of the "Bread & Meat & Fruit & Milk" group dropped from 19.4% in 1998 to 14.4% in 2007 to 2009 (P=0.007). Among females aged 13 to 15 years, the proportion of the "Rice & Kimchi" pattern increased and that of the "Bread & Meat & Fruit & Milk" pattern decreased. As for the 16 to 18 years old group, the proportion of the "Rice & Kimchi" pattern decreased among males (70.1% in 1998 to 65.4% in 2007 to 2009), and the proportion of the "Bread & Meat & Fruit & Milk" pattern increased among females (17.7% in 1998 to 30.8% in 2007 to 2009).
We further examined the association between the dietary pattern and metabolic syndrome and its components. The risk of elevated serum triglyceride was low in adolescents in the "Noodle & Mushroom" (odds ratio [OR], 0.457; 95% CI, 0.267 to 0.781) dietary pattern groups, and the risk of low HDL-cholesterol levels was low in adolescents in the "Bread & Meat & Fruit & Milk" pattern group (OR, 0.684; 95% CI, 0.511 to 0.916) compared to the "Rice & Kimchi" pattern group (Table 4). The "Rice & Kimchi" pattern was characterized by heavy consumption of white grain, as compared to the "Bread & Meat & Fruit & Milk" pattern. A positive relationship between metabolic syndrome and refined grain consumption and a negative relationship between metabolic syndrome and whole grain consumption were also confirmed by a Mexican study based on 5,240 adults25). Contrary to previous studies by Kim et al.17) and Song et al.18), there were no significant differences of obesity risks among the dietary pattern groups.
These results indicated that the "Rice & Kimchi" dietary pattern is highly correlated with serum triglyceride; therefore, dietary patterns having more fruits, vegetables and whole grains and fewer refined grains should be recommended for prevention of metabolic syndrome.
This study has a number of strengths. To our knowledge, this is the first study that analyzed secular trends of dietary pattern over more than 10 years among Korean adolescents. However, several limitations also need to be considered in the interpretation of our findings. First, we used cluster analysis to identify dietary patterns using one day 24-hour recall data, which may not be representative of usual dietary intake. Second, the cross-sectional study limited the interpretation of the findings for causal association. Therefore, further research is required for longitudinal studies with large populations and measurement of usual dietary intakes.
In conclusion, based on our systematic review, that Western dietary patterns are positively associated with metabolic syndrome risk factors such as obesity and elevated triglycerides, while traditional dietary patterns were negatively associated. Data analysis found that the "Rice & Kimchi" pattern has decreased and the "Bread & Meat & Fruit & Milk" pattern has increased over the last 10 years among Korean adolescents. In contrast to the positive association of "Western" dietary pattern with metabolic risk factors, our data on Korean adolescents showed that the "Rice & kimchi" dietary pattern was related with increased risk of elevated serum triglycerides and reduced HDL cholesterol levels compared with other dietary pattern groups. Furthers studies on the effects of carbohydrate-oriented "Rice & Kimchi" dietary pattern of young people on dyslipidemia or long-term metabolic risks are needed.
Acknowledgment
This study was done by the grant from Moonseok, The Korean Association of Obesity 2010.