Antibody response to pneumococcal vaccination in children with chronic or recurrent rhinosinusitis
Article information
Abstract
Purpose
Although chronic and recurrent rhinosinusitis is prevalent in children, little is known about its causes. Here, we investigated the humoral immunity in children with chronic or recurrent rhinosinusitis.
Methods
We examined 16 children attending the outpatient clinic at the CHA Bundang Medical Center including 11 boys and 5 girls, aged 3.11 years (mean age, 5.6 years), who had rhinosinusitis for >3 months or >3 times per year. The complete blood count with differential and total serum concentrations of Immunoglobulin (Ig) E, IgA, IgD, IgM, IgG, and IgG subclasses (IgG1, IgG2, IgG3, and IgG4) of all children were measured. All subjects received 23-polysaccharide pneumococcal vaccination (PPV), and the levels of antibodies to 5 serologic types (4, 6B, 14, 18C, and 23F) of pneumococcal capsular polysaccharide antigens were measured before and after vaccination. Post-PPV antibody titers ≥0.35 µg/mL or with a ≥4-fold increase were considered as positive responses.
Results
The titers of IgG, IgA, IgD, and IgM were within normal range in all 16 children, whereas the total IgE concentration was higher than normal in 2 children. IgG1 deficiency was observed in 1 patient and IgG3 deficiency in 3. After PPV, 1 patient failed to respond to all 5 serologic types, 2 failed to respond to 4 serologic types, and 2 failed to respond to 3 serologic types.
Conclusion
Clinicians should consider the evaluation of humoral immune functions in children with chronic or recurrent rhinosinusitis who do not respond to prolonged antibiotic treatment.
Introduction
Rhinosinusitis, defined as an inflammation of the nose and paranasal sinuses, is one of the most common disorder in pediatric populations. Although it is difficult to estimate the incidence of rhinosinusitis in children, 5-10% of children with upper respiratory tract infections will go on to develop acute rhinosinusitis with a subset of children progressing on to chronic or recurrent state1,2). The chronic or recurrent inflammatory state disrupt daily activities and impair their quality of life, especially when the symptoms are recurrent or chronic. Acute rhinosinusitis is usually infectious whereas the etiology of chronic or recurrent rhinosinusitis remains poorly defined. The general consensus is that the etiology of chronic or recurrent rhinosinusitis is multifactorial. Factors predisposing to the development of chronic or recurrent rhinosinusitis include allergy, various immune-associated disorders, defects in the mucociliary clearance system, and biofilms-associated chronic bacterial infection.
Immunoglobulin (Ig) antibody levels, the four subclasses of human IgG, have an important role in host defenses against bacteria and viruses. Deficiencies in IgA or IgG are considered to play an important role in the development of chronic rhinosinusitis3). Of the IgG subclass deficiencies, IgG2 deficiency has been most closely associated with chronic/recurrent rhinosinusitis in children4,5). However, IgG-subclass levels can vary with age and therefore, transitory Ig defects may occur as one ages. Additionally, the existence of serotype-specific IgG antibodies to pneumococcal bacteria may play an important role in the prevention of pyogenic infections. Furthermore, antibody response to pneumococcal vaccination (PPV) is a good measure of humoral immune function6). A great body of evidence have demonstrated a close association between immune function, as measured by antibody response to PPV, and recurrent infections, such as rhinosinusitis7,8). To date, however, there have been no studies confirming a relationship between humoral immune function and antibody titers in a Korean subjects who had vaccination against pneumococcus. Therefore, we sought to ascertain the association between humoral immune deficiency and chronic or recurrent rhinosinusitis in Korean children by measuring antibody responses to 23-polysaccharide PPV in children with chronic or recurrent rhinosinusitis.
Materials and methods
1. Subjects
The present study involved 16 children attending the outpatient clinic at the CHA Bundang Medical Center, who had chronic or recurrent rhinosinusitis for more than 3 months or more than three times in a year at the CHA Bundang Medical Center between January and July 2007. Informed consent for participation was obtained from the guardian of each subject. Rhinosinusitis was diagnosed by patient inquiry and subsequent examination by an experienced pediatrician according to the guidelines of the American Association of Pediatrics9). Chronic rhinosinusitis was defined as episodes of inflammation of the paranasal sinuses with the presence of thick nasal discharge and productive cough for more than 3 months. Recurrent rhinosinusitis was defined as presence of bacterial infection of the paranasal sinuses, each lasting less than 30 days and separated by intervals of at least 10 days during which the patient is asymptomatic9).
2. Methods
All patients were vaccinated with Streptococcus pneumoniae capsular polysaccharide (Pneumo 23, Korean Vaccine Co., Seoul, Korea) in the outpatient clinic at the CHA Bundang Medical Center. Prior to vaccination, a differential complete blood count was performed; erythrocyte sedimentation rate (ESR) was measured; and serum concentrations of total IgE, IgA, IgD, IgM, and IgG, and the IgG subclasses (i.e., IgG1, IgG2, IgG3, and IgG4) were assayed. Igs were analyzed using a BN II Nephelometer (Dade Behring, Marburg, Germany). Antibody titers to five serologic types of capsular polysaccharide (4, 6B, 14, 18C, and 23F) were measured in serum samples obtained before and 4-6 weeks after vaccination, using third-generation enzyme-linked immunosorbent assay, at the Center for Vaccine Evaluation and Study at Ewha Womans University. The five most common serologic types in Korea7,10,11) were selected for analysis. Antibody titers ≥0.35 µg/mL after vaccination or with a ≥4-fold increase were considered positive12,13). Conversions of three of five antibody titers with a <4-fold increase were considered abnormal10,13). Normal ranges for immunoglobulins were determined using data of the Mayor Medical Laboratory14), figures from Boston15), and a Korean database16).
Results
1. Clinical characteristics of chronic or recurrent rhinosinusitis in children
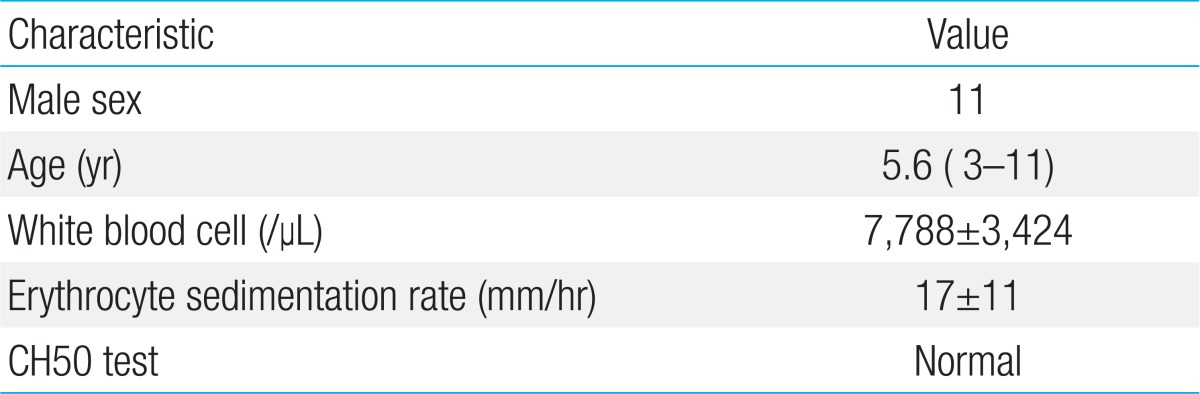
The present study consisted of 16 patients (11 boys and 5 girls) aged between 3 and 11 years, with a mean age of 5.6 years. The total blood cell numbers and proportion of white blood cells (WBCs) were within normal ranges in all patients, although the ESR levels of three children were higher than the reference range. All patients had normal CH50 test results (Table 1).
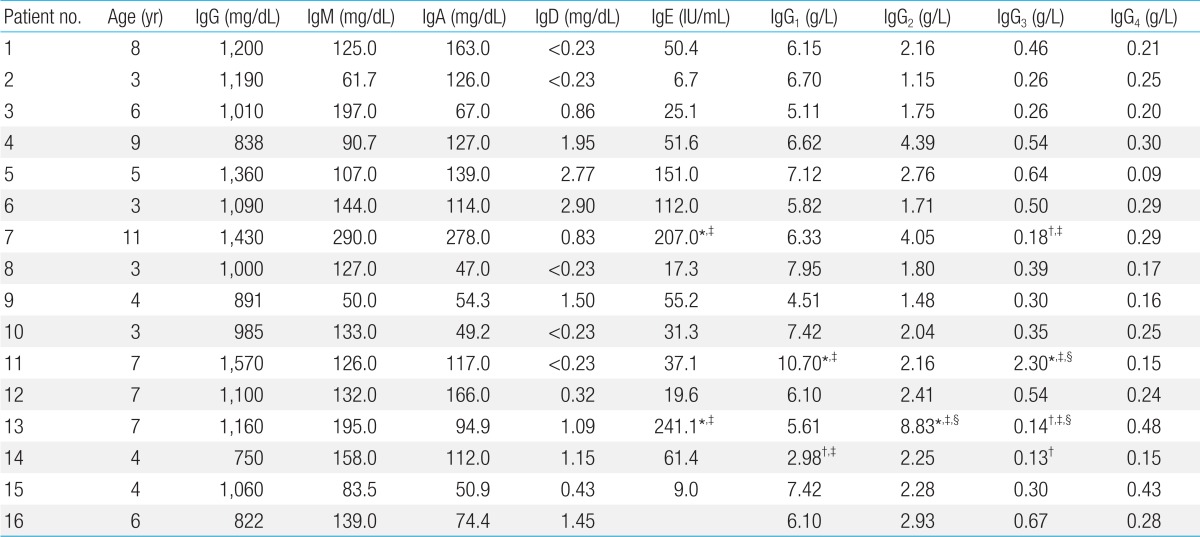
2. Serum immunoglobulin concentrations in patients
Total IgG, IgA, IgD, and IgM concentrations were normal in all patients, when comparing the patients' results to the test's reference values14), whereas total IgE concentrations were high in two patients. Among the IgG subclasses, all patients had normal IgG4 concentration. One patient had an above-normal IgG1 concentration and one a below-normal level, and one patient had an above-normal IgG2 concentration. One patient had an above-normal and three a below-normal IgG3 concentration (Table 2).
3. Antibody titers before and after polysaccharide PPV
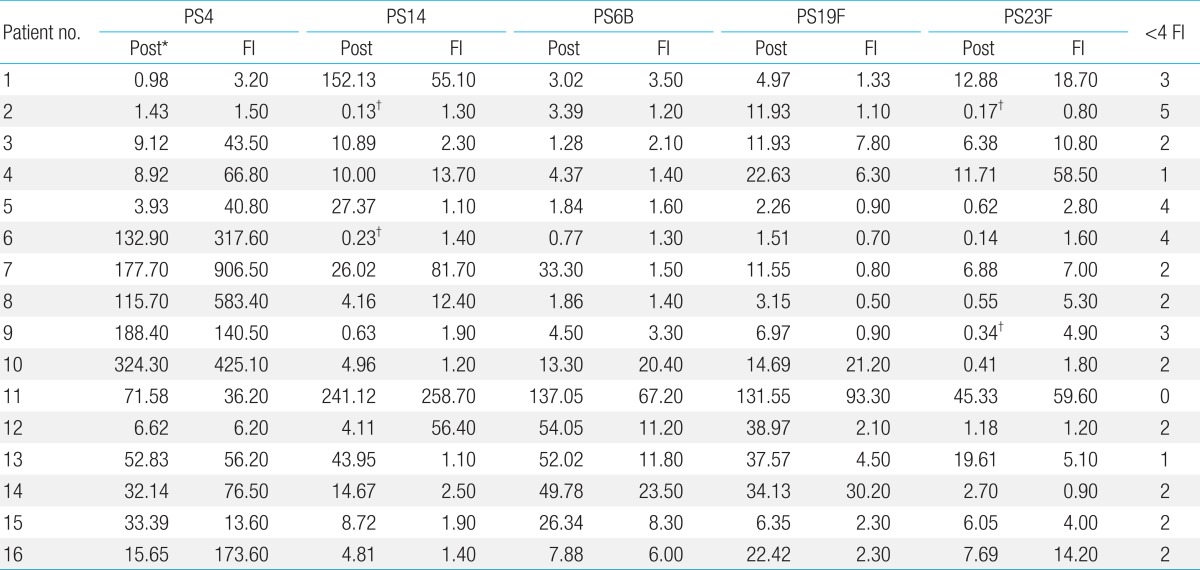
Thirteen of the 16 patients (81%) showed normal antibody conversion, >0.35 µg/mL, to all five antigens (4, 6B, 14, 18C, and 23F) after polysaccharide PPV. Of the three patients who showed abnormal conversion, all responded to PS23F and two patients responded to PS4. Five patients (31%) did not yield a 4-fold increase; of these, two showed a <4-fold increase in three polysaccharide-specific antibodies, two showed a <4-fold increase in four antibodies, and one showed a <4-fold increase in all five antibodies (Table 3).
Discussion
We found that one patient (6.2%) had an IgG1 deficiency and three (18.7%) had an IgG3 deficiency. Based on antibody titers to five pneumococcal antigens, we found that 5 of 16 patients (31%) showed abnormal humoral immune function. Taken together, 8 of 16 patients (50%) had abnormal results on immune studies, three of whom had IgG subclass deficiency and five of whom had abnormal humoral immune function.
The most important measure of humoral immune function is assessment of changes in antibody titer after vaccination6). We measured antibodies to five serologic types. We defined a significant change as a ≥4-fold increase in at least three titers. We found that two patients (12.5%) showed no significant increase in three titers (sensitivity, 63.6%; specificity, 87.4%) and one showed no significant increase in any of the five titers (sensitivity, 72.7%; specificity, 56.8%). A previous study consisting of 307 adult patients with chronic rhinosinusitis demonstrated that 67 patients of them (21.8%) showed a humoral immune deficiency17,18). Another study by Shapiro et al.19) in 61 children with refractory sinusitis showed that 34 of them (55.7%) had abnormal immune results; 11 patients had low Ig levels, 6 had low Ig levels and vaccine hyporesponsiveness, and 17 had poor vaccine response only. In line with previous studies, we found that a high proportion of our patients (5 of the 16 patients [31%]) demonstrated humoral immune deficiency. In contrast, the study by Hidalgo et al.6) in in 78 children with recurrent infections found that only five of them (6.4%) failed to develop protective antibody levels after vaccination against pneumococcus. Another study examining 245 adult patients with chronic rhinosinusitis not responding to prolonged antibiotic treatment reported that only 22 patients (9%) showed low Ig levels after vaccination against pneumococcus18). Furthermore, it has been suggested that antibody production capacity may not have an important role in the development of chronic rhinosinusitis. Taken together, humoral immune deficiency is not a common cause of chronic rhinosinusitis and clinicians should consider other causes of chronic rhinosinusitis not responding to proper antibiotic treatment8).
Although previous studies have demonstrated a relationship between IgA and IgG2 deficiencies and chronic rhinosinusitis in adults20,21), we were unable to confirm these data as none of our patients showed an IgA or IgG2 deficiency. We found that one patient (6.2%) had an IgG1 deficiency and three (18.7%) had IgG3 deficiencies. In line with our study, a previous study of 30 patients with chronic rhinosinusitis showed that 3, 7, 14, and 10 patients had IgG1, IgG2, IgG3, and IgG4 deficiencies, respectively.22) Another study of 307 adult patients with chronic rhinosinusitis demonstrated that 7 patients (2.2%) had IgA deficiencies, 6 (2.0%) IgG2 deficiencies, and 55 (17.9%) IgG3 deficiencies.17) Another study consisting of 245 patients with chronic rhinosinusitis found that 5 patients (2.0%), 10 patients (4.1%), 1 patient (0.4%), and 1 patient (0.4%) had IgG1, IgG2, IgG3, and IgG4 deficiencies, respectively, and 5 (2.0%) had a common variable immune deficiency18). A previous study comprising 27 allergic respiratory children with recurrent sinusitis reported that primary and/or secondary humoral immune deficiency is not the main cause of chronic/recurrent sinusitis8). A previous study consisting of 30 Korean children demonstrated that there is a close association between immune deficiency and recurrent or chronic rhinosinusitis in children22). To the best of our knowledge, there have been no studies confirming a relationship between humoral immune function and antibody titers in patients with pneumococcemia. While the prevalence is not different from our results, the smaller number of patients in our study made it difficult to determine the prevalence of immunoglobulin deficiencies. Therefore, it is not clear whether IgG subclass deficiencies are clinically significant in children with chronic or recurrent rhinosinusitis23).
The present study has limitations that need to be taken into account when considering the study and its contributions. Firstly, the present study had no control group. Secondly, it had relatively small number of subjects compared with previous studies.
In conclusion, we determined immune deficiencies in children with chronic or recurrent rhinosinusitis by quantitating immunoglobulin concentrations and measuring antibody titers to PPV and found that a substantial proportion of patients with chronic or recurrent rhinosinusitis had abnormal immune functions. Therefore, humoral immune deficiency may be considered as a cause of chronic or recurrent rhinosinusitis. Relevant treatment guidelines and long-term measurement of antibody titers may be needed in patients with recurrent or chronic rhinosinusitis.
Acknowledgments
We thank Carl Frasch at Center for Biologics Evaluation and Research, Food and Drug Administration, Bethesda, MD, USA. For providing us with the reference standard 89-SF.
Source of financial assistance: This work was partially supported by a grant from KFDA 05092-341 to Kyung-Hyo Kim.
Notes
No potential conflict of interest relevant to this article was reported.