Mycoplasma pneumoniae associated stroke in a 3-year-old girl
Article information
Abstract
Infectious diseases precede a significant proportion of acute ischemic strokes in children. Here, we report a case of acute ischemic stroke in a 3-year-old girl with a Mycoplasma pneumonia-associated respiratory tract infection. She developed an acquired prothrombotic state of protein S deficiency and had increased fibrinogen and fibrinogen degradation product levels and increased titer of antinuclear antibodies. However, these conditions were completely alleviated at the 1-month follow-up examination. Infection with M. pneumoniae may cause a transient prothrombotic state that can potentially cause a thrombus.
Introduction
Childhood stroke, by definition, is a cerebrovascular event that happens between 30 days and 18 years of age. Stroke in children is rare, with an annual incidence of 2-4/100,000 in the United States1), but ischemic stroke is more common than hemorrhagic stroke. Furthermore, infectious diseases precede a significant proportion of acute ischemic strokes (AIS) in children. Based on the research done by the International Pediatric Stroke Study (IPSS), at least 24% of cases of AIS were related to infection2). The most common infectious agent is Varicella zoster virus, but other causes including Mycoplasma pneumoniae, Chlamydia pneumoniae , Parvovirus B19, Borrelia burgdorferi , influenza A virus, Human immunodeficiency virus, and mumps virus infection have been identified as potential risk factors for arterial ischemic stroke during childhood. However, only 11 cases of M. pneumoniae-associated AIS in childhood have been reported. In addition, four of the 11 cases were presumed to be related to a prothrombotic state, but none of them was proved to be acquired.
Here, we report a case of acute stroke in a 3-year-old girl who presented on the seventh day of M. pneumoniae infection with an acquired prothrombotic state, which was normalized 1 month later.
Case report
A previously healthy 3-year-old girl with left-sided paresis was admitted to the Department of Pediatric Neurology in Korea University Ansan Hospital. Seven days before admission, she experienced an abrupt onset of high fever and cough. Three days prior to admission, fever subsided, but she was diagnosed with pneumonia at a local clinic. On the day of admission, left-sided hemiparesis and left facial palsy developed. She was transferred to our hospital with the presumed diagnosis of encephalitis from the local clinic. The patient's family history and past medical history were unremarkable.
Physical examination on admission revealed an alert, oriented girl. Her body temperature was 36.2℃, pulse rate 104/min, respiratory rate 22/min, and blood pressure 105/56 mmHg. Chest examination revealed crackles on the right lung. On neurological examinations, central type facial palsy was observed on the left side of face, and motor strength was decreased to grade III/VI in the left arm and leg.
Initial laboratory studies showed a white blood cell (WBC) count of 15,110/mm3 with neutrophils of 60.9%, lymphocytes of 27.6%; hemoglobin, 13.0 g/dL; and platelets, 449,000/mm3. The erythrocyte sedimentation rate was 63 mm/hr and C-reactive protein, 0.5 mg/dL (reference range, <0.3 mg/dL). Biochemical investigations were normal. Lumbar puncture yielded clear cerebrospinal fluid (CSF) with an opening pressure of 170 mmH20. Cell counts showed WBC, 13/µL (10 lymphocytes); red blood cell, 20/µL; protein, 17 mg/dL; and glucose, 67 mg/dL, while the simultaneous blood glucose was 105 mg/dL. CSF was sterile on culture. Patchy infiltration of the right lung was recognized on the chest radiograph.
Initially, intravenous vancomycin, cefotaxime and acyclovir were administered. Vancomycin and acyclovir were discontinued and oral azithromycin was added when immunoglobulin (Ig) M positivity was detected on the second day of admission. IgM antibody titer to M. pneumoniae determined by the enzyme-linked immunosorbent assay (ELISA) was increased to 9.7 RU/mL (reference range, 0.0 to 1.1 RU/mL), which was still positive (14.1 RU/mL) 13 days later. Prothrombin time and partial thromboplastin time, complement factors (C3, C4), protein C level and antithrombin III level were normal, but protein S level was decreased to 16% (reference range, 58.7% to 119.2%). Fibrinogen and fibrinogen degradation product (FDP) levels were 526 mg/dL (normal, 257 to 503 mg/dL) and 17.2 µg/mL (reference range, 0.1 to 3.6 µg/mL), respectively. Antinuclear antibodies (ANA) were weakly positive, and serum titer was 1:160 with a nonspecific whole cell staining pattern. Electrocardiography and echocardiography were normal. Magnetic resonance imaging (MRI) revealed an acute infarction in the territory of the right lenticulostriate artery (Fig. 1). However, magnetic resonance angiography showed no luminal narrowing or obstruction of regional vessels. Bacteriological cultures of blood and CSF were sterile.
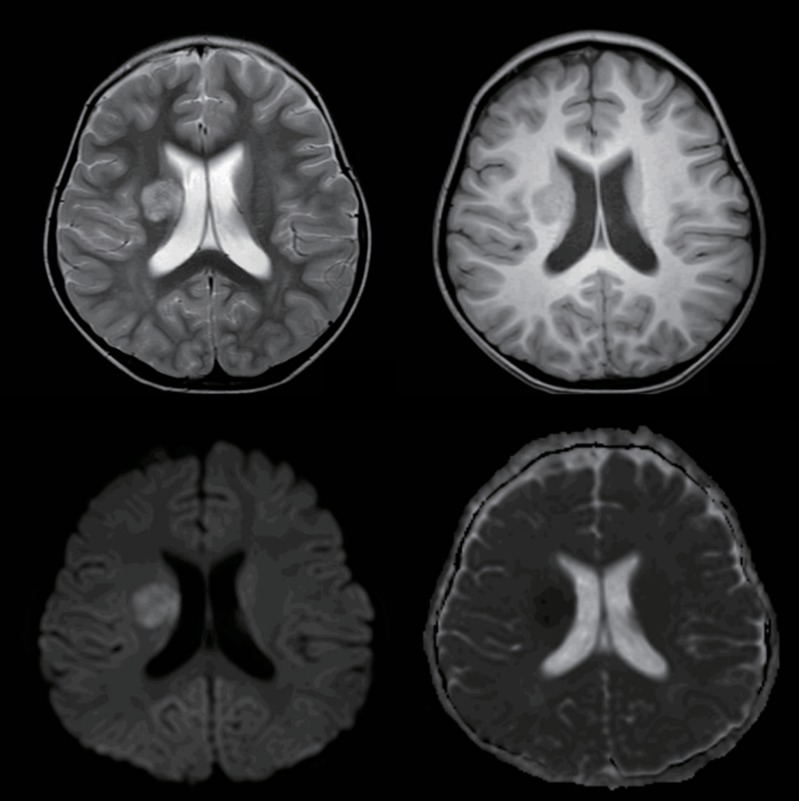
Magnetic resonance imaging (MRI) was performed on a 3T MRI scanner (Achieva 3T; Philips Medical System). MRI images showed a round lesion involving the right basal ganglia, which was hyperintense on T2-weighted images (top left image) and hypointense on T1-weighted images (top right image), with diffusion restriction (bottom left image) and low apparent deficient coefficient values (bottom right image), indicating acute infarction in the area of the right lenticulostriate arteries.
Three days after initiation of oral azithromycin treatment, respiratory symptoms began to improve. Intravenous cefotaxime was discontinued after confirming negative cultures in CSF and blood. Within five days, the left-sided hemiparesis and the left central facial palsy also started to resolve. After eight days of hospitalization, she could walk without dragging her leg, demonstrating minimal weakness, and she was subsequently discharged. Protein S level was increased to 37% two weeks after onset. One month after the beginning of her illness, this level normalized to 63%. Fibrinogen and FDP levels also normalized to 404 mg/dL and 2.3 µg/mL, respectively. ANA also became negative. Neurological symptoms totally resolved.
Discussion
In the present case, the patient manifested left-sided weakness after M. pneumoniae infection, and right-sided infarction was also noted on MRI in the territory of the right lenticulostriate artery, which could explain her symptoms. In addition, ANA and protein S level were abnormal at the time of AIS but normalized spontaneously in a month. Infection with M. pneumoniae may cause a transient prothrombotic state that could feasibly cause thrombus formation.
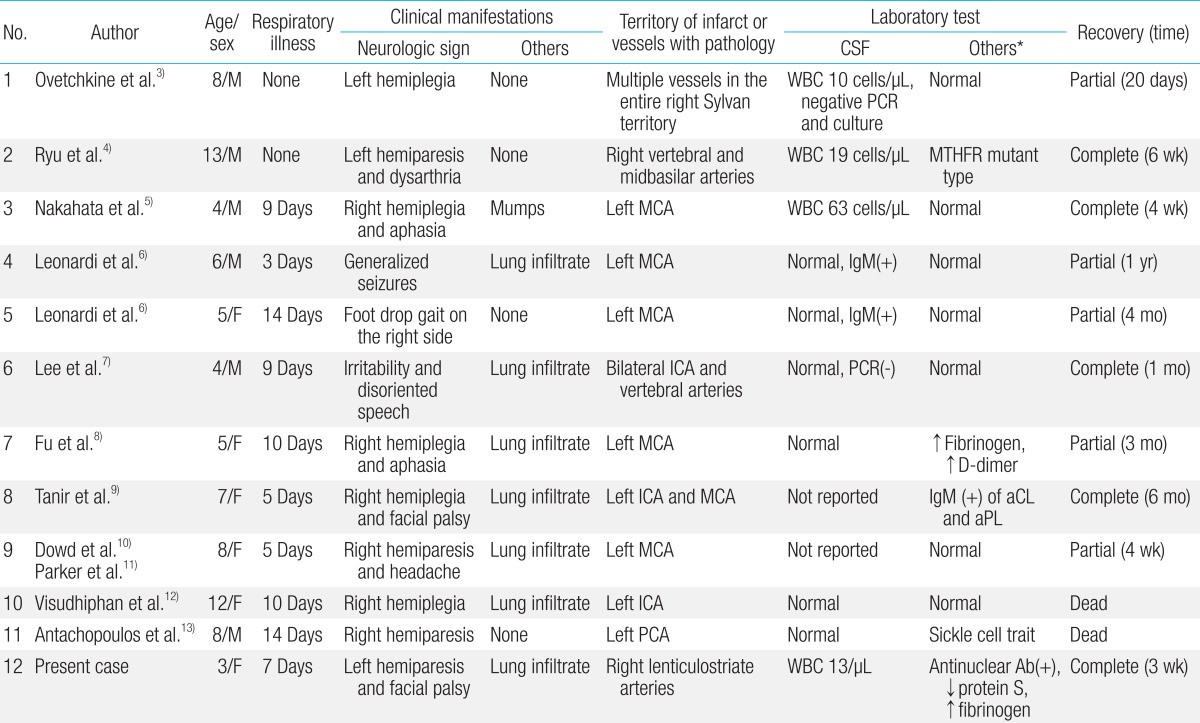
Upon review of the literature, 11 children with M. pneumoniae-associated AIS were previously reported (12 children including our case), as summarized in Table 1. A Medline/PubMed search was performed on February 9, 2012 (keywords: stroke, mycoplasma) to identify all similar cases in the medical literature, followed by manual search of the references of relevant articles written in English. Age distribution was variable, ranging from three to 13 years. Male to female ratio was 1:1. The interval between the onset of respiratory symptoms and CNS manifestation was 8.8 days on average (range, 3 to 14 days). No obvious respiratory symptom was noted in three cases3,4) and mumps was accompanied in 1 case5). However, nine of 12 cases (75%) had recent respiratory symptoms, while six of 12 cases (50%) had definite pneumonic infiltration on chest X-ray6-12). Most patients presented with weakness of one side of the body or face, often with dysarthria or aphasia. Rarely, irritability or seizure was the initial manifestation6,7). CNS pathology was most commonly observed in the left middle cerebral artery (six of 12 cases, 50%). Mycoplasma infection was proved by serology, culture or polymerase chain reaction (PCR). Various methods of serologic testing including ELISA, complement fixation, cold agglutinin assay or immunoblot were used. However, no organism was proven by PCR or culture in CSF. CSF pleocytosis were variably observed in only four cases (33.3%). Prothrombotic tendency was noted in several cases; increased fibrinogen and D-dimer8), sickle cell trait13), positive IgM antibodies of anticardiolipin and antiphospholipid9) and a genetic defect in the methylenetetrahydrofolate reductase gene which can result in hyperhomocysteinemia4). In our case, antinuclear antibody was positive with a titer of 1:160, and fibrinogen level was increased, while protein S level was decreased in the acute stage. However, all of these measures returned to normal after one month. Treatment was mainly with a macrolide for M. pneumoniae infection. Additionally, low-dose aspirin, intravenous immunoglobulin and steroids were used inconsistently throughout all the cases. Prognosis was variable. Two of 12 children (16.7%) died. The remaining children improved quickly soon after initiating treatment, but improved slowly at the later stage, resulting in various outcomes.
There is limited data about M. pneumoniae-associated stroke. In general, all types of CNS disease associated with M. pneumoniae occur more commonly in young people ranging from six to 21 years of age, who are more prone to contract M. pneumoniae respiratory infection. It is well known that infection with M. pneumoniae often accompanies neurologic manifestations, varying from meningoencephalitis, myelitis, Guillian-Barre syndrome and stroke, which are rarely reported in children. Proposed hypotheses include direct invasion of M. pneumoniae, a neurotoxin produced by the organism, or immune-mediated damage. However, direct invasion of the organism does not appear to be the main cause in most cases because of the paucity of reported cases with the organism isolated from the CNS. Immune-mediated damage includes autoimmunity, organism-induced immune suppression, immune complex vasculopathy and thrombosis of vessels. In vitro experimental studies have suggested that the procoagulant activity (tissue factor-like activity) could be induced by lipoglycans of M. pneumoniae via human mononuclear cells14). Though there is no gold standard assay yet, and serology for detecting antibodies in serum plus PCR for detection of M. pneumoniae in CSF has been recommended for better detection, especially in neurologic manifestations. DNA of M. pneumoniae has been rarely detected in CSF using PCR in adult stroke case15), but never detected in children. The presence of an IgM antibody specific to M. pneumoniae signifies acute infection. IgM antibody response precedes IgG response by a few days and is commonly detected after seven to ten days of illness. MRI, computed tomography imaging, and cerebral angiography could help to establish the exact anatomical location of the occlusion or thrombosis in stroke cases and could provide evidence for cerebral vasculitis disclosing multiple stenoses. However, normal findings have been reported.
In conclusion, we should be aware of the risk for cerebral ischemic stroke as a complication during the clinical course of M. pneumoniae respiratory tract infection. Furthermore, a prothrombotic state with increased titers of anticardiolipin and antiphospholipid IgM antibodies, fibrinogen, or D-dimer might be observed if suspected. Infection with M. pneumoniae may cause a transient prothrombotic state that feasibly could create a thrombus.
Notes
No potential conflict of interest relevant to this article was reported.