Hepatitis associated with Mycoplasma pneumoniae infection in Korean children: a prospective study
Article information
Abstract
Purpose
Mycoplasma pneumoniae (MP) infection is a major cause of respiratory infection in school-aged children. Extrapulmonary manifestations of MP infection are common, but liver involvement has been rarely reported. The aim of this study was to determine the clinical characteristics of MP-associated hepatitis.
Methods
This prospective study included 1,044 pediatric patients with MP infection diagnosed serologically with MP IgM at one medical center from January 2006 to December 2012. Eighty of these patients had elevated levels of serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT), each greater than 50 IU/L, without any other specific liver disorder and were compared with the 964 children without liver disorders.
Results
In total, 7.7% of patients with MP infection had a diagnosis of hepatitis, especially in fall and winter. The ratio of male to female patients was 1.7:1, and the mean age of the patients was 5 years and 5 months. The most common symptoms were cough, fever, and sputum. Anorexia was the most common gastrointestinal symptom, followed by nausea/vomiting, diarrhea, and abdominal pain. Mean levels of AST and ALT were 100.65 IU/L and 118.73 IU/L, respectively. Serum AST/ALT level was normalized within 7.5 days on average without complications. The mean duration of hospitalization (11.3 days) was longer for children with hepatitis than for those without hepatitis (P=0.034).
Conclusion
MP-associated hepatitis is not uncommon and has a relatively good prognosis. Therefore, clinicians should be concerned about liver involvement in MP infection but avoid further unnecessary evaluation of hepatitis associated with MP.
Introduction
Mycoplasma pneumoniae is one of the major causes of lower respiratory tract infection in children and adolescents, and accounts for up to 40% of cases of community-acquired pneumonia1), which reportedly is prevalent every three or four years in South Korea2). Contrary to the belief that it was a self-limiting and benign disease when its strain was first discovered, M. pneumoniae infection can cause problems in diverse tissues in the nervous, hematologic, cardiovascular, skeletal, and renal systems, and in the skin as well as the respiratory system34). Common extrapulmonary complications of these conditions include aseptic meningitis, skin rash, hepatitis, pancreatitis, myocarditis, pericarditis, and arthritis34). While hepatitis complicated with M. pneumoniae infection forms as much as 10% to 30% of all M. pneumoniae infections observed so far, no prospective study has been conducted on the subject in a large population of children and adolescents5678).
We prospectively examined the clinical features of hepatitis complicated with M. pneumoniae infection in general and compared them with those of M. pneumoniae infection not accompanied by hepatitis.
Materials and methods
The research was conducted prospectively between January 2006 and December 2012 for identification of the age and gender distribution, seasonal distribution, clinical manifestations, laboratory and radiological findings, and treatment outcomes in M. pneumoniae hepatitis patients. There were 80 patients with liver disorders among a total of 1,044 patients under 19 years old, hospitalized and diagnosed with M. pneumoniae infection at the Department of Pediatrics, Gachon University Gil Medical Center. These 80 patients with hepatitis were also compared with 964 children without liver disorders in terms of the length of hospitalization.
M. pneumoniae infection was defined as the condition where the serum anti-Mycoplasma pneumoniae antibody titer of IgM (Platelia M. pneumonia IgM, enzyme immunoassay; Bio-Rad, Marnes-la-Coquette, France) value is equal to or greater than that of the cutoff serum specimen included in the kit at the time of admission to the hospital. Those who were negative for hepatitis A, B, and C viruses, Epstein-Barr virus, and cytomegalovirus, with serum aspartate aminotransferase (AST) and serum alanine aminotransferase (ALT) levels elevated to 50 IU/L or higher, respectively, were diagnosed as M. pneumoniae hepatitis.
The results were analyzed using MedCalc ver. 13.3.0 (MedCalc Software, Mariakerke, Belgium) and were expressed as mean±standard deviation, standard error or as percentage. Independent Student t-test was performed for determination of the variation in the length of hospitalization according to the presence of hepatitis, with statistical significance set at P<0.05. All of the research protocols were approved by the Ethics Committee of Gachon University Gil Medical Center (GCIRB2014-24).
Results
1. Incidence
The incidence of hepatitis complicated with M. pneumoniae infection was 7.7%, with 80 children having hepatitis as a complication among 1,044 diagnosed with M. pneumoniae infection.
2. Age and gender distribution
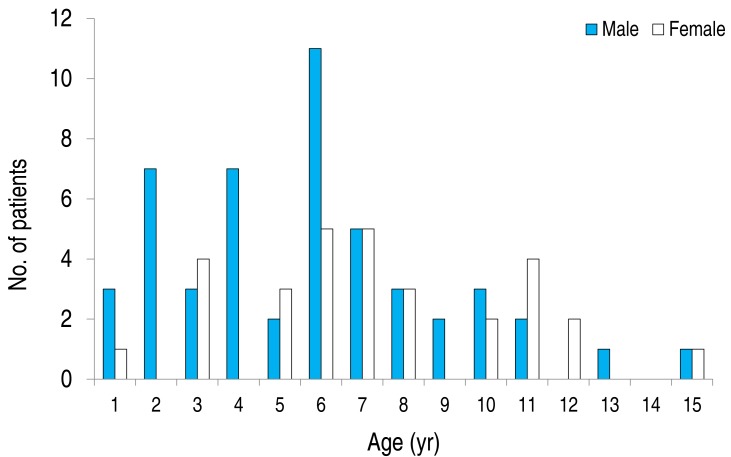
Age ranged from 10 months to 16 years, with a mean of 5.51±3.32 years and a median of five years and a half. The male-to-female ratio was 1.7 to 1 (Fig. 1).
3. Seasonal and annual distribution
Among 1,044 Mycoplasma infection patients, there were markedly fluctuating frequencies over the years. Epidemics were noted in 2007 (291 cases) and 2011 (280 cases). Much less cases occurred in other years (129 cases in 2006, 100 cases in 2008, 91 cases in 2009, 81 cases in 2010, 72 cases in 2012). There were two peaks for the number of the Mycoplasma hepatitis patients during the study period occurring in 2007 (25 cases) and 2011 (22 cases), and a range of 2-12 sporadic cases in other years. Cases also appeared more frequently during fall and winter: from March to August in 20 cases (25.0%), from September to November in 39 cases (48.8%), and from December to February in 21 cases (26.2%) (Fig. 2).
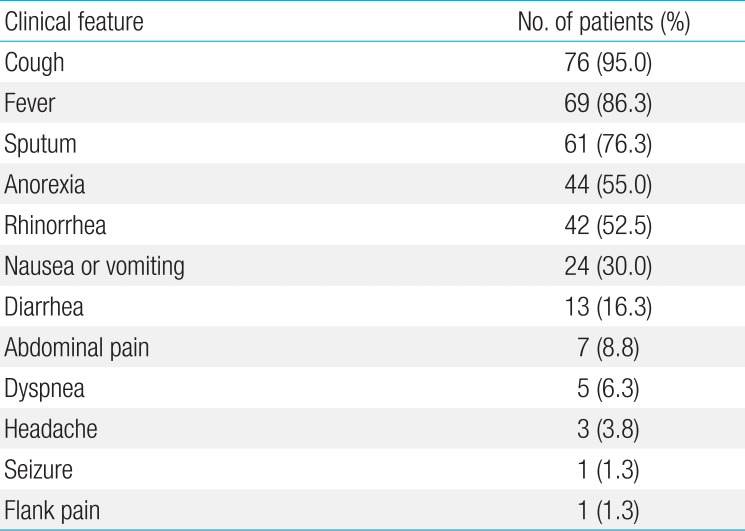
4. Clinical symptoms
Among children with M. pneumoniae hepatitis, the most common respiratory symptom was cough (76 cases, 95.0%), followed by sputum (61 cases, 76.3%), rhinorrhea (42 cases, 52.5%), and respiratory distress (5 cases, 6.3%). The most common gastrointestinal manifestation was anorexia (44 cases, 55%), followed by nausea/vomiting (24 cases, 30%), and diarrhea (13 cases, 16.3%) (Table 1).
5. Findings of physical examination
The most common finding of physical examination was coarse breathing sound (56 cases, 70%), followed by rale (40 cases, 50%), pharyngeal injection (38 cases, 47.5%), decreased breathing sound (19 cases, 23.8%), and palatine tonsillar hypertrophy (17 cases, 21.3%). The nonrespiratory sign most frequently found by examinations was rash (4 cases, 5%), followed by hepatomegaly (3 cases, 3.8%), and cervical lymph node enlargement (2 cases, 2.5%) (Table 2).
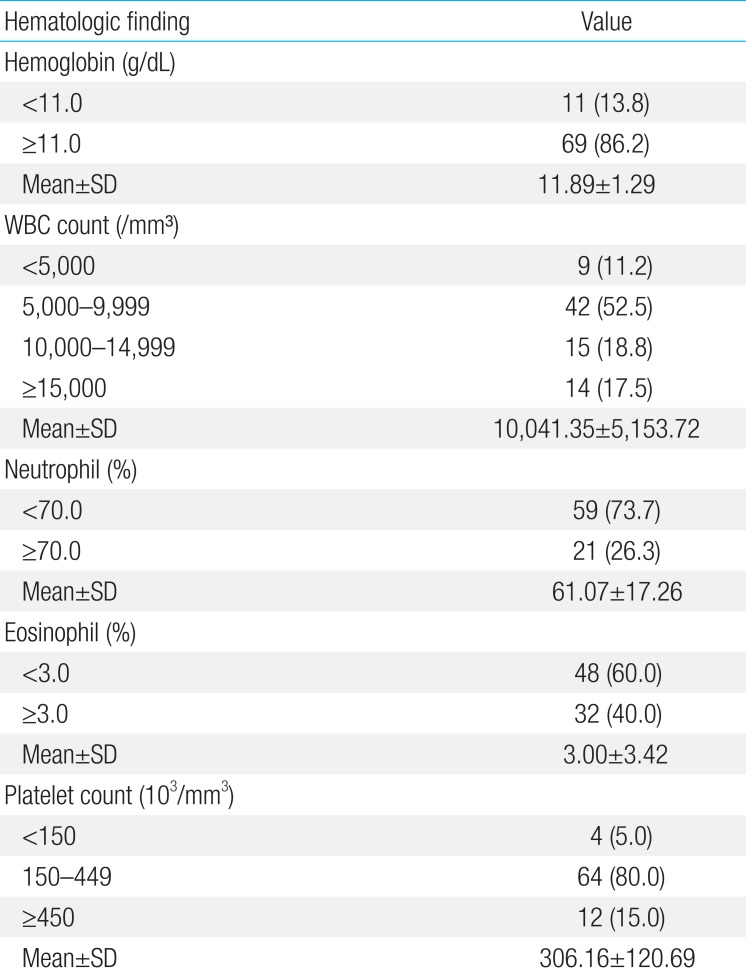
6. Hematologic findings
Eleven cases (13.8%) had hemoglobin of less than 11 g/dL, and the most common level of peripheral blood white blood cell was 5,000-9,999/mm3 (42 cases, 52.5%), followed by 10,000/mm3 or more (29 cases, 36.3%) and less than 5,000/mm3 (9 cases, 11.2%). The results of blood smear showed neutrophilia (>70%) in 21 cases (26.3%), and eosinophilia (>3%) in 32 cases (40.0%). Twelve cases (15.0%) had platelet increased to 450,000/mm3 or more and four cases (5.0%) had it decreased to less than 150,000/mm3 (Table 3).
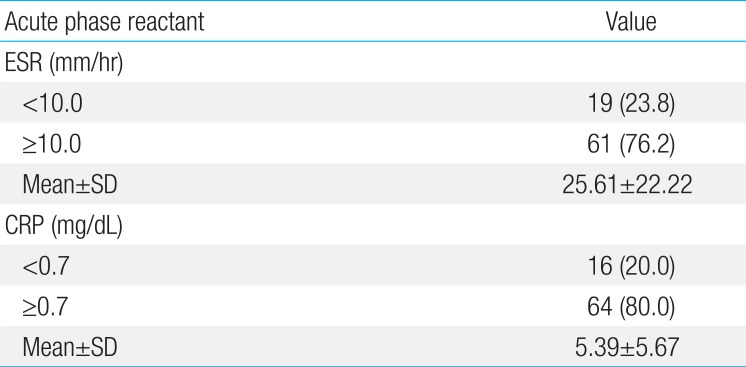
The average erythrocyte sedimentation rate (ESR) was 25.61±22.22 mm/hr and was elevated by 10 mm/hr or higher in 61 cases (76.3%). C-reactive protein (CRP) was 5.39±5.67 mg/dL on average with a maximum of 22.02 mg/dL and was elevated to 0.7 mg/dL or more in 64 cases (80.0%) (Table 4).
7. Findings of liver function test
AST was 100.65±20.34 IU/L on average with a maximum of 1,330 IU/L, and ALT was 118.73±19.43 IU/L on average with a maximum of 1,171 IU/L at day of admission. The average level of bilirubin was 0.39±0.16 mg/dL, with only one case of hyperbilirubinemia (>1.2 mg/dL). Total protein and albumin were 6.73±0.74 g/dL and 3.96±0.57 g/dL on average, respectively, and the latter decreased to less than 3.5 g/dL in 21 cases (26.3%) with the minimum measured value of 2.9 g/dL (Table 5).
8. Radiological findings
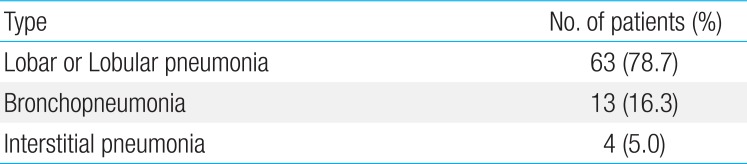
All children with M. pneumoniae hepatitis had pulmonary infiltration: the most common type was lobar or lobular pneumonia (63 cases, 78.7%), followed by bronchopneumonia (13 cases, 16.3%) and interstitial pneumonia (4 cases, 5.0%) (Table 6). Fifty-eight cases (72.5%) had unilateral infiltration, and 31 cases (38.8%) had the left lower lobe affected by infiltration. Pleural effusion was observed in 11 cases (13.8%) and was unilateral in each case (Table 7).

Radiological types of lung infiltration on admission in patients with Mycoplasma pneumoniae hepatitis (n=80)
9. Treatment and outcomes
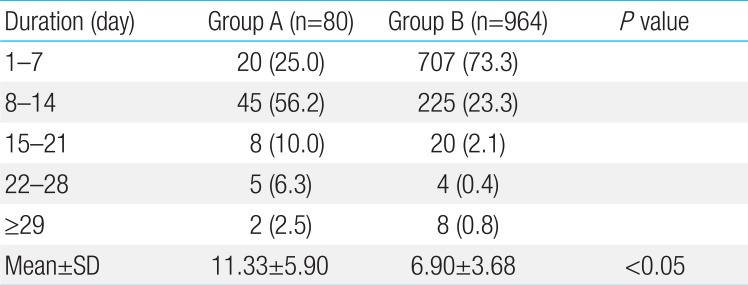
All children with M. pneumoniae infection were given an oral medication of roxithromycin for two weeks. The mean length of hospitalization was longer for children with liver disorder than for those without a such condition: 11.33±5.90 days for the former and 6.90±3.68 for the latter (P<0.05) (Table 8). An average of 7.51±4.57 days was required for the AST/ALT levels to be normalized; 44 cases (55.0%) had it normalized within one to seven days and liver function was fully restored within 28 days in all cases (Table 9).

Comparison of length of hospitalization in patients with Mycoplasma pneumoniae infection with or without hepatitis
Discussion
Our study has been done prospectively using IgM antibodies for diagnosis of M. pneumoniae infection. Even though incidence of Mycoplasma associated hepatitis is not uncommon, studies usually has been done retrospectively, and in Korea, no study has been conducted on the subject using IgM antibodies for diagnosis. There are some limitations, but compared to other diagnostic test like culture or polymerase chain reaction, the IgM test is most efficient for making a serological diagnosis as a single laboratory examination9).
It is believed that formation of M. pneumoniae hepatitis can occur within one to 21 days after a respiratory symptom is found to accompany M. pneumoniae infection1011). Although the apparent mechanism for this complication has not yet been determined, there are two major hypotheses: One is that it is caused by the appearance of autoimmune antibodies or localization of an immune complex following M. pneumoniae infection since M. pneumoniae antibodies can cross-react with liver tissues and cause damage of tissues by the immunomechanism3). As is well known, this can be explained by the formation of autoimmune antibodies, such as cold agglutinin, after M. pneumoniae infection.
The other hypothesis is that M. pneumoniae directly infects epithelial cells12); however, whether it also immediately infects cells in the hepatobiliary system has not yet been determined. According to one report, M. pneumoniae uses pyruvate dehydrogenase on its surface to combine itself with protein fibronectin, which is rich in the liver, on the eukaryotic cell surface13). As we observed that antibiotic medications induced rapid restoration of the liver function, it can be assumed that M. pneumoniae directly infects cells in the hepatobiliary system.
While some researchers5678) reported incidence of M. pneumoniae hepatitis ranging from 9% to 30%, we found an incidence of 7.7%. The variation among researchers is probably due to geographical and temporal factors and the criteria for diagnosis of M. pneumoniae hepatitis. Despite the differences between the reports, the incidences indicate that hepatitis in M. pneumoniae infection is not uncommon, and that it is necessary to give attention to whether the liver function is within normal range in case of a M. pneumoniae infection.
We observed that M. pneumoniae hepatitis appeared more frequently during fall and winter, similar to M. pneumoniae pneumonia: 75.0% of cases occurred from September to February3).
It has also been reported that M. pneumoniae infection tends to occur at a gradually younger age and is most frequently found in children aged 0 to 6 years1415). This is probably due to the fact that more children go to a daycare center on a daily basis, thus they are more susceptible to infection through respiratory secretions14). In this study on M. pneumoniae hepatitis, 70.0% of all of the children were 0 to 6 years old and no more than 6.3% were 11 years or older. It has been reported that M. pneumoniae infection was found slightly more frequently in males than in females16); similarly, we estimated the male-to-female ratio as 1.7 to 1.
Regarding the clinical features of M. pneumoniae infection, it has an incubation period ranging from 15 to 20 days, is primarily transmitted by droplets, and symptoms develop slowly once the infection occurs. It is accompanied by cough in almost all cases and may involve nonrespiratory symptoms, such as digestive symptoms, anemia, muscle pain, joint pain, skin lesions, and neurologic symptoms3). Murray et al.17) and Stevens et al.16) reported that up to 40% of patients with M. pneumoniae infection could have nausea, vomiting, anorexia, diarrhea, or abdominal pain; we observed that 95% had cough, 55% anorexia, 30% nausea and vomiting, and 16.3% diarrhea.
Regarding hematological findings, Smith et al.18) reported that the total leukocyte count was mostly at normal or slightly elevated levels and neutrophilia was found by the differential count in the case of M. pneumoniae infection, and Stevens et al.16) observed that 64% of cases had normal leukocyte count, 33% had leukocytosis, and 67% had neutrophilia; in our study, we found a normal leukocyte count in 42 cases (52.5%), leukocytosis in 29 cases (36.3%), neutrophilia in 21 cases (26.3%), and a reduction of the neutrophil count to less than 5,000/mm3 in nine cases (11.2%). The hemoglobin level dropped to less than 11.0 g/dL in 11 cases (13.8%), the platelet level was elevated to 450,000/mm3 or higher in 12 cases (15.0%), and dropped to less than 150,000/mm3 in four cases (5.0%), and 61 cases (76.3%) had elevated ESR. Watanabe et al.5) reported that CRP was most strongly associated with M. pneumoniae hepatitis; we observed that it was positive in 64 cases (80.0%) with a maximum of 22.02 mg/dL.
The principal type of liver disorder is an elevated AST level, and jaundice is rarely found13). We estimated AST as 100.65±181.91 IU/L on average with a maximum of 1,330 IU/L and ALT as 118.73±173.78 IU/L on average with a maximum of 1,171 IU/L. We also observed that total bilirubin was increased to 1.2 mg/dL or more in only one case and that there was no case of jaundice. Twenty-eight cases (58.5%) had hypoalbuminemia, in agreement with the observations by Park and Chung6) and Lee et al.8).
While we did not perform liver biopsy for any of the patients, one case report in which liver biopsy was performed19) showed massive hepatocellular destruction and inflammatory infiltration and another case20) showed a manifestation of severe and acute lobular hepatitis. One research study involving liver biopsy in three children21) showed a manifestation of non-specific reactive hepatitis.
While the findings from chest radiology for M. pneumoniae pneumonia vary in general, Lee et al.8), who conducted research on M. pneumoniae hepatitis, most frequently found a lobar or lobular type of pneumonic infiltration and we found pulmonary infiltration in 78.8% of the children and left lower lobe affected by infiltration in 38.8%. Park and Chung6) and Lee et al.8) reported that the mean length of hospitalization for M. pneumoniae hepatitis was 15.48 days and 9.91 days, respectively, and we found the mean length of hospitalization to be 11.33±5.90 days, ranging from four to 34 days, for children with M. pneumoniae hepatitis, and 6.90±3.68 days for those with M. pneumonia infection not accompanied by hepatitis; thus, the former were hospitalized longer than the latter. This gap can probably be explained by the fact that patients hospitalized due to hepatitis complicated with M. pneumoniae infection could not be discharged until its cause was determined and the liver function test was normalized. In agreement with previous reports6781019) showing that increased level of hepatic transaminases accompanying M. pneumoniae infection was normalized through treatment without specific complications, we observed that all patients who received an oral medication of roxithromycin for two weeks had full restoration of liver function within 28 days with no secondary complication of hepatitis in any case, despite the extended length of hospitalization. Roxithromycin, an antibiotic metabolized in the liver, can have a side effect of hepatotoxicity; however, we believe that the possibility that any medication caused the hepatitis can be excluded because all patients had an elevated hepatic enzyme level before treatment began and the level dropped after treatment.
This study has a few limitations: Since elevated level of IgM will decay slowly through up to 6 months, it is not certain if the reaction is from current infection or from a primary abnormality. Also poor sensitivity of IgM in the very early phase of the disease could have resulted in failure to diagnose some children with M. pneumoniae infection. Tests to detect respiratory viruses that could also cause hepatitis in these children have not been always performed. Lastly, there could be a selection bias since the study was conducted in children and adolescents hospitalized in only one center. We suggest that conduct of extensive research involving institutions in various regions will be necessary.
In conclusion, hepatitis complicated with M. pneumoniae infection is not uncommon and generally has a relatively good prognosis since it showed no significant difference from M. pneumoniae infection as reported in the existing clinical researches. However, the length of hospitalization was extended due to the amount of time needed for the restoration of the liver function. Therefore, it is recommended that clinicians should consider the potential of hepatitis when M. pneumoniae infection is confirmed and avoid performing more tests than necessary for any liver disorder.
Acknowledgments
This article's abstract was chosen and presented as Oral Abstract Communications Session in ESPGHAN 2014.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.