Food allergen sensitization in young children with typical signs and symptoms of immediate-type food allergies: a comparison between monosensitized and polysensitized children
Article information
Abstract
Purpose
The clinical interpretation of children sensitized to allergens is challenging, particularly in children with food allergies. We aimed to examine clinical differences between children with monosensitization and those with polysensitization to common food allergens and to determine risk factors for polysensitization in young children <10 years of age with immediate-type food allergies.
Methods
The study included children <10 years of age with signs and symptoms indicative of immediate-type food allergies. Serum total IgE level was measured, and ImmunoCAP analysis for food allergens was performed.
Results
The mean age of the study subjects was 1.6±1.6 years (75 boys and 51 girls). Thirty-eight children (30.2%) were monosensitized and 88 children (69.8%) were polysensitized. Multivariate logistic regression analysis showed that the development of polysensitization to common food allergens was positively associated with a parental history of allergic rhinitis (adjusted odds ratio [aOR], 6.28; 95% confidence interval [CI], 1.78-22.13; P=0.004), season of birth (summer/fall) (aOR, 3.10; 95% CI, 1.10-8.79; P=0.033), and exclusive breastfeeding in the first 6 months of age (aOR, 3.51; 95% CI, 1.20-10.25; P=0.022).
Conclusion
We found significant clinical differences between children with monosensitization and those with polysensitization to common food allergens and identified risk factors for the development of polysensitization in young children with immediate-type food allergies. Clinicians should consider these clinical risk factors when evaluating, counseling, treating, and monitoring young children with food allergies.
Introduction
Allergic diseases are an important public health problem due to the fact that they impose a significant socioeconomic burden on society by lowering the quality of life of allergic patients and their families. Among various allergic diseases, food allergy is especially concerning in that it can cause serious and even fatal reactions in individuals of all age groups, particularly in children. A nationwide epidemiological study conducted on Korean children found that the estimated overall prevalence of immediate-type food allergies was 0.6% in children aged 6-7 years and 1.6% in children aged 12-13 years1).
Food allergies are diagnosed when both allergen-specific IgE (sIgE) to food allergens is present and the typical signs and symptoms develop upon exposure to a certain food12). Previous studies have suggested that some people are sensitized to only one class of allergen (monosensitization), whereas others are sensitized to two or more classes of allergen (polysensitization) 34). Additionally, studies have reported that polysensitization differs both clinically and immunologically from monosensitization56). Researchers have demonstrated that there are significant differences between monosensitized and polysensitized subjects with allergic rhinitis3) and asthma4). However, to date, there is no data available reporting whether children with food allergies may present different clinical characteristics in regard to the number of sensitized food allergens.
The aims of the present study were to determine clinical differences between children with monosensitization and those with polysensitization to common food allergens and to identify risk factors for polysensitization in young children less than 10 years of age with immediate-type food allergies.
Materials and methods
1. Study subjects
This is a retrospective review of data from pediatric patients treated between January 2008 through December 2013 at the Pediatric Allergy and Immunology Clinic at the CHA Gangnam Medical Center, Seoul and the CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. The patients were identified from a large clinical database, if they fulfilled the inclusion criteria. The inclusion criteria for this study were children aged 0-10 years presenting with typical signs and symptoms of immediate-type food allergies, who underwent allergy testing for the following foods: hen's eggs, cow's milk, peanuts, soybeans, and wheat by measuring food-specific serum IgE, and who had more than one clinic visit during the study period. Food allergies were diagnosed based on a convincing history of reproducible signs and symptoms within 2 hours following ingestion of a single food7) and specific IgE level to the suspected food ≥0.35 IU/mL8). The charts of 223 children were examined; 57 children were excluded because all of their food-specific IgE levels tested were <0.35 IU/mL and 40 children were excluded because the offending food, according to their parents' report, did not match their food-specific IgE positivity. Children who presented with food allergy signs and symptoms following ingestion of a fruit or vegetable were excluded because specific IgE tests for commercially available fruit or vegetable allergens are often negative owing to structural instability9). Thus, a total of 126 children were included for the final analysis. We divided the signs and symptoms of the children that developed within 2 hours of food intake in regard to the affected organs: (1) skin reactions, such as urticaria, rash, itching, or redness; (2) gastrointestinal reactions, including nausea, vomiting, abdominal pain, diarrhea, or bloody stool; (3) respiratory reactions, such as respiratory difficulty, dyspnea, wheezing, cough, rhinorrhea, nasal obstruction, or chest tightness; (4) isolated angioedema; (5) oropharyngeal reactions, such as itching of the mouth, tongue, and throat or lip swelling; and (6) anaphylaxis7). Anaphylaxis was defined as signs and symptoms that developed immediately after exposure to certain foods and involved at least two major organ systems according to the established guidelines10). Other clinical factors recorded included sex, age, gestational age at birth, birth weight, diet during the first 6 months of age, number of previous live births, season of birth, patient and parental history of allergic diseases including asthma11), allergic rhinitis-like symptoms12), atopic dermatitis13) and food allergy7), and type of delivery. The Institutional Review Board reviewed and approved the study; informed consent was waived by the ethical review board because this was a retrospective analysis of stored laboratory data.
2. Serum specific IgE measurements
The ImmunoCAP system (Phadia AB, Uppsala, Sweden) was used for specific IgE assessment throughout the study period. Sensitization was defined as a specific IgE concentration ≥0.35 IU/mL8).
3. Statistical analysis
All continuous variables are presented as mean values with standard deviation. The Student t test was used to examine the statistical differences in age, gestational age, birth weight, and total IgE levels between monosensitized and polysensitized children. The chi-square test was used to examine the statistical differences in sex, the number of siblings, diet within the first 6 months of age, seasons of birth, type of delivery, family history of allergic diseases, and comorbid allergic diseases of the subjects between groups. All statistical analyses were performed by using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). All statistical tests were two-sided, and statistical significance was determined at a P value <0.05.
Results
1. Population characteristics
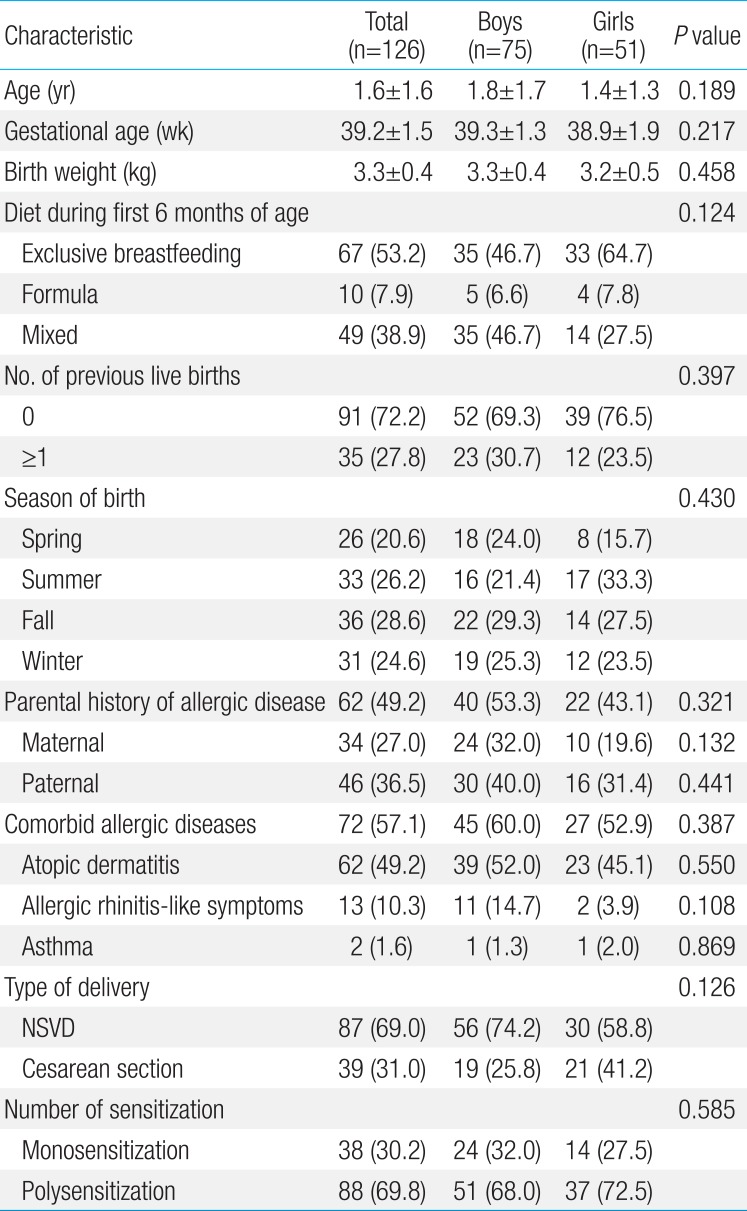
The demographic and clinical characteristics of the study population are presented in Table 1 (75 boys and 51 girls). The mean age of the study subjects were 1.6±1.6 years. Diets during the first 6 months of age were exclusive breastfeeding (53.4%), formula (7.8%), and mixed (38.8%). The percentage of the study subjects who were a first child was 72.1% and 49.1% of the study subjects had a parental history of allergic diseases. With respect to the child's history of allergic diseases, 57.3% of the study subjects were found to have comorbid allergic diseases such as asthma, allergic rhinitis-like symptoms, or atopic dermatitis (Table 1). There were no statistically significant differences in clinical parameters between boys and girls.
2. Signs and symptoms of the study subjects and causative food allergens
Table 2 shows the reported signs and symptoms that developed within 2 hours of ingestion of the offending food according to the afflicted organs; 90.0% of the children showed cutaneous manifestations, 10.0% with gastrointestinal reactions, 7.3% had respiratory reactions, 12.7% displayed angioedema, 5.5% with oropharyngeal reactions, and 12.7% suffered anaphylaxis. Of the young children with typical signs and symptoms of food allergies, hen's eggs (85.5%) were the most frequent food allergen, followed by cow's milk (73.3%), wheat (42.4%), peanuts (38.5%), and soybeans (33.6%).
3. Comparison of clinical variables between monosensitized and polysensitized subjects
Of the 126 children with food allergies, 38 children (30.2%) were monosensitized and 88 children (69.8%) were polysensitized. Polysensitized children were more likely to have been born in summer or fall, as opposed to monosensitized children in spring or winter, although the difference was not statistically significant (P=0.057). Polysensitized children were more likely to have parents with allergic rhinitis (43.8% vs. 20.6%, P=0.019) and to have been exclusively breastfed during the first 6 months of life when compared with monosensitized children (62.2% vs. 32.4%, P=0.005) (Table 3). The percentage of children with comorbidities, such as atopic dermatitis, allergic rhinitis-like symptoms, and asthma, was 63.6% in the polysensitized group and 42.4% in the monosensitized group (P=0.039). Polysensitized children showed higher total IgE levels when compared with monosensitized children, although the difference was not statistically significant (299.1±491.3 IU/mL vs. 180.1±345.9 IU/mL, P=0.195) (Table 3).
4. Risk factors for polysensitization to food allergens in young children with food allergies
The multivariate logistic regression analysis was performed to determine independent relationships between polysensitization and clinical parameters in children with food allergies. The results suggest that a parental history of allergic diseases (i.e., allergic rhinitis) (adjusted odds ratio [aOR], 6.28; 95% confidence interval [CI], 1.78-22.13; P=0.004), season of birth (summer/fall) (aOR, 3.10; 95% CI, 1.10-8.79; P=0.033), and exclusive breastfeeding within the first 6 months of age (aOR, 3.51; 95% CI, 1.20-10.25; P=0.022) were significantly associated with the development of polysensitization to common food allergens in young children with immediate-type food allergies (Table 4).
Discussion
This study shows that a parental history of allergic diseases (i.e., allergic rhinitis), season of birth (i.e., summer/fall), and exclusive breastfeeding within the first 6 months of age are significantly associated with the development of polysensitization to food allergens in young children with immediate-type food allergies. To the best of our knowledge, this is the first study to determine clinical risk factors for the development of polysensitization to common food allergens in young children with immediate-type food allergies.
The results of the present study correspond well with previous studies showing that polysensitized subjects tend to have a higher incidence of a parental history of allergic disease compared to monosensitized subjects414). It is not clear why subjects become sensitized to one or more classes of allergens, although genetic and environmental factors have been implicated. There is a significant difference in clinical characteristics between monosensitized and polysensitized groups, such that polysensitized children tend to demonstrate more severe symptoms34) and have a lower health-related quality of life15) than monosensitized children. Considering that the regulation of specific IgE synthesis is coordinated by the skewness of antigen-presenting cells in response to microbial exposure via toll-like receptors, it can be inferred that environmental exposure to microorganisms plays an important role in the evolution of polysensitization through increasing the tendency to produce IgE. This hypothesis was supported by a previous study of an analysis of specific IgE tests in children 0-18 years of age showing a strong association between total serum IgE levels and the degree of polysensitization16).
Previous studies have suggested that season of birth is associated with the risk of the development of food allergies71718). We found that the season of birth, namely summer or fall, was a risk factor for polysensitization in children with food allergies. Our results correspond in part with previous studies demonstrating fall birth being associated with increased risk of food allergies719) and sensitization to food allergens18). These results may support the hypothesis that food allergens and environmental exposure, according to different seasons during fetal period, may be risk factors for the development of allergic diseases in offspring7). Studies have suggested that many cytokine responses, specifically interferon (IFN)-α and IFN-γ, vary by season of birth20). In utero timing and its relationship to seasonal differences in viral and other prenatal factors might be crucial in regulating the effects of these factors on immune evolution of offspring2122). Collectively, it is possible that various seasonal factors, such as microbial exposure, viral infection, allergen exposure, 25-hydroxyvitamin D concentration, or pollution, etc., could have a significant effect on the development of sensitization to various food allergens.
It is generally accepted that exclusive breastfeeding has a preventive effect on the early development of allergic diseases, including food allergies; however this preventive strategy has recently been called into question. A recent birth cohort study, which followed children through 5 years of age, found that breastfeeding for any duration was significantly associated with the development of food allergies and sensitization in the children8). Another prospective birth cohort study of 970 children demonstrated that children who were ever breastfed (including exclusively breastfed children) were at 1.5 times higher risk of developing food sensitization than never breastfed children; this positive association was modified by rs425648 in the gene encoding interleukin-12 receptor β123). In line with these previous studies, we found that exclusive breastfeeding increased the risk of polysensitization to common food allergens. There is no clear explanation as to why exclusive breastfeeding increased the risk of polysensitization to food allergens in our study subjects. One possible mechanism for this finding is that food allergens delivered via breast milk can promote sensitization to food allergens in exclusively breastfed infants, generating a T cell-mediated allergen-specific immune response24). Although we did not measure Th1 or Th2 lymphocytes or perform genotyping of the study subjects, it is plausible that various food allergens ingested by mothers during lactation may have been passed via breast milk, resulting in Th2-skewed immune modulation of offspring. Further research with a larger sample size is warranted to expand and delineate the relationship between exclusive breastfeeding and the development of polysensitization to food allergens.
Children with food allergies present with various signs and symptoms, with skin reaction being the most common7). In line with previous studies, we found that skin reaction was the most prevalent. Contrary to a previous study7), the present study showed significant proportions of subjects with gastrointestinal reactions, respiratory reactions, angioedema, oropharyngeal reactions, and anaphylaxis. This finding may be ascribed to the fact that the present study included subjects who visited a Pediatric Allergy and Immunology Clinic at general hospitals, as opposed to the previous study, which included subjects from the general population. Based on our results, we suggest that clinicians inquire into each individual's various manifestations, not only of skin reactions, but also of reactions affecting other organs, when examining patients presenting with signs and symptoms of food allergies.
Limitations of our study include a relatively small number of subjects, retrospective study design, and the fact that a double-blind placebo-controlled food challenge was not performed to confirm food allergies in the study subjects. A prospective study with a large sample size is needed to confirm the findings suggested by the present study.
In conclusion, the present study found that there are significant clinical differences between children with monosensitization and those with polysensitization to common food allergens and that a parental history of allergic diseases (i.e., allergic rhinitis), season of birth (i.e., summer/fall), and exclusive breastfeeding within the first 6 months of age are significantly associated with the development of polysensitization to common food allergens in young children with immediate-type food allergies. Clinicians should take these clinical risk factors into consideration when evaluating, counseling, treating, and monitoring young children with food allergies.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.