Clinical characteristics of lung abscess in children: 15-year experience at two university hospitals
Article information
Abstract
Purpose
Information on the clinical features of lung abscess, which is uncommon in children, at hospitalizationis helpful to anticipate the disease course and management. There is no report concerning lung abscess in Korean children. We aimed to identify the clinical characteristics of pediatric lung abscess and compare the difference between primary and secondary abscess groups.
Methods
The medical records of 11 lung abscess patients (7 males and 4 females) from March 1998 to August 2011 at two university hospitals were retrospectively reviewed. The clinical characteristics, symptoms, underlying disease, laboratory and radiologic findings, microbiological results, and treatments were examined.
Results
Six patients had underlying structural-related problems (e.g., skeletal anomalies). No immunologic or hematologic problem was recorded. The mean ages of the primary and secondary groups were 2.4 and 5.3 years, respectively, but the difference was not statistically significant. The mean length of hospital stay was similar in both groups (22.8 days vs. 21.4 days). Immunologic studies were performed in 3 patients; the results were within the normal range. Most patients had prominent leukocytosis. Seven and 4 patients had right and left lung abscess, respectively. Staphylococcus aureus, Streptococcus pneumoniae, and antimycoplasma antibodies were detected in both groups. Two patients with primary lung abscess were administered antibiotics in the absence of other procedures, while 8 underwent interventional procedures, including 5 with secondary abscess.
Conclusion
The most common symptoms were fever and cough. All patients in the primary group were younger than 3 years. Structural problems were dominant. Most patients required interventional procedures and antibiotics.
Introduction
Lung abscess is a thick-walled cavity in the pulmonary parenchyma that contains purulent material and is initiated or complicated by infectious organisms1). Lung abscess is classified as primary or secondary depending on underlying conditions. Primary lung abscess occurs in the absence of a specific lung disease, while secondary lung abscess occurs in the presence of predisposing structural or functional lung diseases including congenital lung disorders, ciliary dyskinesia, and cystic fibrosis, systemic diseases such as neuro-developmental abnormalities and congenital immunodeficiencies that may lead to aspiration or infection12). It is known that primary and secondary lung abscesses present differences in causative organisms, progression, and prognosis34).
The introduction of antimicrobials into clinical practice has improved the prognosis of lung abscess, but the literature from 1969 to 2005 reported mortality rates ranging from 2.0%-38.2%5). Pediatric lung abscess can occur at any age and morbidity is lower than that in adults12). There are few published articles regarding the prevalence and clinical course of pediatric lung abscess in children12), and in Korea, there have been only a few reports of cases associated with congenital cystic adenomatoid malformation or necrotizing pneumonia678). The aim of this study is to understand clinical characteristics and to compare the difference between primary and secondary lung abscess for effective evaluation and treatments for lung abscess in Korean children. For these, data from patients with lung abscess at two university hospitals during 15 years were collected and information on clinical manifestations, management, and outcomes was reviewed.
Materials and methods
1. Patients
In this study, the diagnosis of lung abscess satisfied the following criteria: (1) air-fluid level on chest radiographs; (2) thick-walled cavities containing suppurative material and destruction of lung parenchyma on chest computed tomography (CT); (3) radiologist readings that confirmed lung abscess at the time of hospitalization if no radiographs or CT images were available in the record. We excluded cases of pneumonia, necrotizing pneumonia, and empyema without definite abscess formation on radiologic images. We retrospectively reviewed medical records from March 1997 to August 2011. Patients who were discharged from the Pediatric Department, Kyung Hee University Hospital at Gangdong, and Kyung Hee University Medical Center with an International Classification of Disease-9 diagnosis code for lung abscess were selected. After reviewing the medical records, we identified a total of 11 patients under 16 years of age whose radiologic findings were consistent with lung abscess. The patients were categorized into primary and secondary abscess groups in accordance with the presence of underlying disease.
2. Methods
Patient characteristics, clinical symptoms and signs, time to defervescence and recovery, length of hospital stay, and the presence of underlying disease were investigated. Laboratory findings were examined for inflammatory responses and microbiological tests, including blood, sputum, urine, or thoracic fluid cultures and specific antigen or antibody reaction in serum and urine were examined for causative organisms. We reviewed treatment regimens including antibiotic therapy and interventional invasive procedures, designated as percutaneous drainage and surgical procedures including chest tube insertion (thoracostomy), thoracotomy, or lobectomy. Recovery from disease was defined as one of the following: radiologic resolution, clinical symptom improvement, or defervescence (maintenance of body temperature below 38℃ for at least 24 hours)910). We characterized the lung lesions by location and size of abscess, pneumothorax, pleural effusion, and spherical mass or cyst on chest radiographs and chest CT images.
3. Statistical analysis
The patients were classified into primary and secondary abscess groups depending on the presence of underlying disease. Differences between 2 groups were examined using the Mann-Whitney U test for continuous variables and Fisher chi-square test for dichotomous outcomes (SPSS ver. 15, SPSS Inc., Chicago, IL, USA). Continuous variables were expressed as mean±standard deviation and dichotomous outcomes were described as number of patients or percentages (%). P values of <0.05 were considered statistically significant.
Results
1. Patient data, underlying diseases, and radiologic and laboratory findings (Table 1)
A total of 11 patients with lung abscess were recruited (male: female=7:4). Male patients tended to have primary lung abscess (male:female=4:1 vs. 3:3, primary and secondary, respectively). The age of the patients ranged from 1 to 16 years. The mean age of the primary abscess group was younger than that of the secondary abscess group (2.4±0.5 years vs. 5.3±6.0 years, P=0.976), although this was not statistically significant. All patients in the primary abscess group were younger than 36 months.
Five patients with primary lung abscess had no history of choking or aspiration and 6 patients in the secondary group had underlying disease without aspiration. The underlying conditions in patients with secondary abscess were neonatal respiratory distress syndrome (1 patient), congenital cystic adenomatoid malformation (CCAM, 2 patients), pectus excavatum (2 patients), and Tetralogy of Fallot (1 patient). The abscess was located in cysts in patient with CCAM (Fig. 1). One of 2 patients with pectus excavatum had a medical history of incompletely treated pulmonary tuberculosis and thoracic scoliosis. The other patient had developmental delay. The patient with Tetralogy of Fallot had a history of treatment for wound infection after Blalock-Taussing shunt and total correction. Immunologic tests were performed in 2 patients in the primary group and 1 patient in the secondary group. The findings of immunologic studies were with normal ranges.
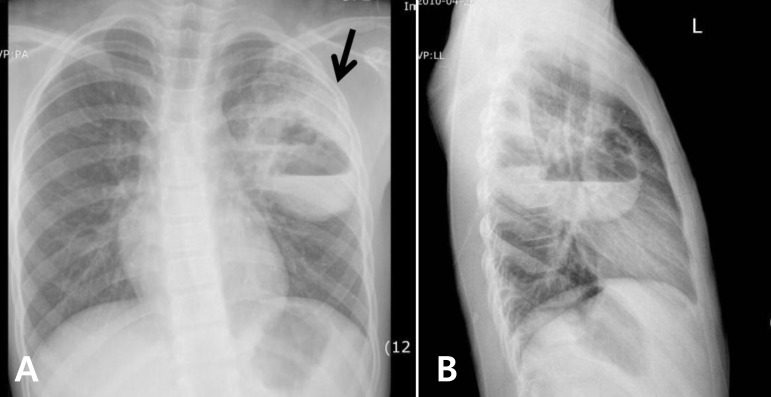
The chest radiography of a typical secondary lung abscess with congenital cystic adenomatoid malformation in patient 7 shows two cysts with an air-fluid level (arrow), respectively, on postero-anterior view (A) and lateral view (B).
On chest radiographs, pneumonia was the most common finding associated with lung abscess (10 patients), followed by atelectasis, pneumatocele, pleural effusion, thoracic mass or cyst (3 patients), and pneumothorax (2 patients). The locations of the lung abscesses were varied on chest CT. In patients with primary abscess, 2 were located in the right lung and 3 were in the left lung. Two patients exhibited involvement of more than two pulmonary lobes, one with abscess in left upper and lower lobes and the other with lung abscess in the right upper and middle lobes. The lung abscesses were >20 mm in diameter, and the size was not significantly different between primary and secondary groups (38±15.7 mm vs. 42±19.4 mm, respectively, P=0.833).
White blood cell counts, C-reactive protein (CRP) and erythrocyte sedimentation rates (ESRs) on admission were elevated in 10 of 11 patients, and there were no difference between 2 groups: complete blood cell count (22,170/µL vs. 14,904/µL), CRP (11.7 mg/dL vs. 14.5 mg/dL) and ESR (46.2 mm/hr vs. 59.6 mm/hr). Nine patients presented with a left shift in the leukocyte count; 2 patients were excluded due to missing or incomplete medical records.
2. Clinical manifestations and laboratory data
Fever was the most common symptom, and was reported in all 11 patients (100%) at the time of admission. Ten patients (91%) presented with cough and sputum. Rhinorrhea and dyspnea were reported in 3 (27%) and 2 patients (18%), respectively. A variety of symptoms such as chest pain, weight loss, abdominal pain, lethargy, and shoulder pain were also present (Table 2).
The mean duration of fever before hospitalization was 9.1±8.3 days in all 11 patients without significance between 2 groups (9.6±8.0 days vs 8.7±9.2 days, P=0.8). There were no differences between primary and secondary abscess groups in terms of length of hospital stay (21.4±9.9 days vs. 22.8±11.4 days, P=0.9), mean time to defervescence (17.4±7.6 days vs. 12.0±7.2 days, P=0.353), hospital days before invasive procedure, including thoracostomy, thoracotomy, or surgery (12.3±11.2 days vs. 19.2±9.4 days, P=0.393), and time to recovery or discharge (24.7±6.5 days vs. 14.8±7.4 days, P=0.161).
3. Etiology and treatments
Putative microbiologic results were found for 6 patients (55%) from specimens of blood, sputum, urine, and thoracic fluid (Table 3). Staphylococcus aureus was isolated from pleural culture in 1 patient and Streptococcus pneumoniae was isolated in 3 patients, from culture of abscess specimen, blood culture with pleural culture, and urine antigen test, respectively. Antimycoplasma antibody tests were performed in 8 patients and were positive response in 2 patients. There was no evidence of viral infection in any patient. No microbial pathogens were detected in the other 5 patients.
Two patients in the primary abscess group were improved with antibiotic therapy alone. One patient who had recurrent fever and rash suggestive of Kawasaki disease was treated with intravenous immunoglobulin. One patient with S. pneumoniae pneumonia who had had persistent fever after discharge from the hospital was diagnosed with lung abscess by chest x-ray performed in the outpatient clinic, and showed improvement in clinical symptoms and radiologic findings upon treatment with a third generation oral cephalosporin.
Eight patients were treated with invasive procedures in combination with antibiotic therapy including third-generation cephalosporins, clarithromycin, clindamycin, vancomycin, and beta-lactam/beta-lactamase complexes. Third generation cephalosporins (8 patients) and clindamycin (7 patients) were used most commonly. The antibiotic regimens were similar in the primary and secondary groups. Pleural injection of urokinase and imipenem via the chest tube was tried in 1 patient who had serological confirmation of Mycoplasma pneumoniae. There was no significant difference between groups in the mean duration of intravenous antibiotics administration during hospitalization (19.8±10.9 days vs. 22.3±10.6 days, P=0.762) or in the time to defervescence after antibiotics use (8.8±8.0 days vs. 6.2±3.8 days, P=0.755).
Three patients in the primary abscess group and 5 in the secondary abscess group required invasive procedures (60% vs. 80%). One patient with CCAM (Fig. 1) and one with primary abscess due to multidrug resistant S. aureus underwent segmentectomy after the acute inflammatory phase. Histologic findings in the patient with primary lung abscess due to S. aureus revealed acute and chronic inflammation with fibrosis consistent with abscess and including hemorrhage and edema and focal peripheral emphysematous change. The other patient was diagnosed with type II CCAM with organizing pneumonia. Three patients in the primary abscess group required thoracostomy. The infecting organisms in these patients were S. aureus in 1, S. pneumoniae in 1, and M. pneumoniae in 1. Four patients in the secondary abscess group required thoracostomy and 1 underwent fluoroscopy-guided thoracotomy. All of these patients had favorable outcomes without any complications.
Discussion
In this study, there were several findings that differ from those of previous studies. First, the patients with primary lung abscess were around 2 years of age, and were younger than those with secondary lung abscess, although this did not reach statistical significance because the sample size was too small. The finding that all of the patients in the primary group were younger than 3 years has not been reported in other studies. Second, in the secondary group, predisposing factors related to structural problems such as skeletal anomalies were dominant. Third, in previous reports, percutaneous aspiration was a preferred intervention when needed, while in the present series the majority of patients underwent interventional procedures that included thoracostomy and segmentectomy, and in all such cases, the timely interventional procedures appeared to be valuable. Lastly, in the present series, there were no reported sequelae in any patients; all were completely cured.
While all patients in the present series had fever, none presented with gastrointestinal signs or symptoms or hemoptysis1481112). One patient, who had penicillin resistant S. aureus in pleural effusion, reported shoulder pain. Overall, in the present study, there was no significant difference in clinical manifestations between primary and secondary lung abscess groups.
Previous studies have reported that duration of hospitalization ranged from 13 days to 28 days in patients with primary lung abscess and was longer for patients with secondary lung abscess4). However, in the present study, the duration of hospital stay did not differ between the two groups. The discordance may be because of the small number of patients, and, in addition, the types of underlying or accompanying conditions. Conditions such as leukemia, congenital heart disease, central nervous system abnormalities, and immune compromise have been reported as common predisposing factors in cases of secondary lung abscess141112). We confirmed underlying lung diseases in 4 patients, including respiratory distress syndrome, partially treated pulmonary tuberculosis, and CCAM, while 2 patients had structural abnormalities (pectus excavatum and scoliosis). Pectus excavatum and scoliosis are musculoskeletal disorders that influence lung function by means of restrictive lung disease caused by decreased intrathoracic capacity, atelectasis caused by cardiac displacement with subsequent left lung compression, and, in severe cases, paradoxical respiration caused by disturbed mechanical forces1013). These mechanical problems in the lung, rather than a lack of pulmonary immunological defense, may have contributed to abscess formation. It should also be noted that predisposing underlying factors may have differed as a result of the prevalence of primary immune deficiencies and trends of antibiotics use in Korea1415).
Aspiration plays a major role of lung abscess formation which is related with dependent segments16). In our series, 6 patients including 1 patient with primary abscess and S. aureus pneumonia, and 1 with secondary abscess and CCAM required segmentectomy had abscess in superior or posterior segments of lower lobes and posterior segments of upper lobes. However, there was no history of aspiration in our patients.
In contrast to lung abscess in adults111718), primary and secondary lung abscess in children is frequently caused by S. pneumoniae, S. aureus, and Pseudomonas aeruginosa117). Because of a reluctance to perform invasive procedures, such as transtracheal aspiration and percutaneous lung needle biopsy, it may be difficult to verify the pathogens in lung abscess. Only 3 patients had pathogens (S. pneumoniae in 2 and S. aureus in 1) isolated in bacterial cultures512), and several patients had findings suggestive of recent infection by M. pneumoniae and S. pneumoniae, i.e., high antimycoplasma antibody titer and positive rapid antigen urine test. Only a few cases of pulmonary abscess in children with M. pneumoniae infection have been described in the literature, and because false-positive test results are common, the detection of pneumococcal antigen in urine by Binax Now is not recommended for the diagnosis of pneumococcal pneumonia in children19). In this study, detection of the antipneumococcal antigen in urine may have meant only a low possibility of S. pneumoniae as a pathogen.
Administration of parenteral antibiotics for 2-3 weeks followed by oral therapy is recommended as treatment for lung abscess678), and beta-lactam/beta-lactamase complex is regarded as the treatment of choice for primary lung abscess20). Other studies have reported the use of broad-spectrum antibiotics including third-generation cephalosporins and flucloxacillin or fluoroquinolones for coverage of aerobic and anaerobic bacteria and penicillin-resistant strains167820). In our series, third generation cephalosporins and clindamycin were commonly used, and no patients were treated with fluoroquinolones.
Abscess drainage is necessary in 20% of cases. The primary indications for drainage are failure to respond to medical therapy alone and the presence of factors such as significant hemoptysis, suspected neoplasm, fever persisting beyond 7-10 days121), or abscess size >6 cm1721). Several authors have reported that left untreated, lung abscesses can lead to irreversible changes including bronchiectasis and fibrosis within 6 to 12 weeks2122). Management decisions in patients with lung abscess may be affected by the nature of the underlying disease. In our patients, thoracostomy was common, which was a different approach from previous studies that have reported percutaneous aspiration as treatment for abscess associated with pneumonia and effusion.
In conclusion, lung abscess in children can occur over a wide range of ages, but an age of <3 years may be influential. Structural problems that cause chest wall deformities or mechanical changes are predominant factors in secondary lung abscess. The combination of antibiotics treatment and interventional procedures may result in a more favorable clinical course for patients with lung abscess in the presence of any aggravating condition. In the present series, the rate of identification of pathogens was low and attempted identification of pathogens was lacking.
Acknowledgment
This study was exempt from Institutional Review Board oversight in the aspect that all patients had been hospitalized in a conventional therapeutic setting and cases were reported before 2011.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.





