A practical view of immunotherapy for food allergy
Article information
Abstract
Food allergy is common and sometimes life threatening for Korean children. The current standard treatment of allergen avoidance and self-injectable epinephrine does not change the natural course of food allergy. Recently, oral, sublingual, and epicutaneous immunotherapies have been studied for their effectiveness against food allergy. While various rates of desensitization (36% to 100%) and tolerance (28% to 75%) have been induced by immunotherapies for food allergy, no single established protocol has been shown to be both effective and safe. In some studies, immunologic changes after immunotherapy for food allergy have been revealed. Adverse reactions to these immunotherapies have usually been localized, but severe systemic reactions have been observed in some cases. Although immunotherapy cannot be recommended for routine practice yet, results from recent studies demonstrate that immunotherapies are promising for the treatment of food allergy.
Introduction
Food allergy is common among Korean children, with 5%–7% prevalence in the Korean population12). The current standard of treatment for food allergy is allergen avoidance coupled with ready access to self-injectable epinephrine and antihistamines3). Although packaged food in Korea have the allergen labeling system since 20044) and this system has been extended to school lunches, complete avoidance of the allergen is difficult. Accidental exposure often occurs, and recently, there was a case of severe anaphylaxis resulting in brain death due to the unexpected presence of a food allergen in school lunch. Changing the natural course of disease in patients with food allergy is a hot topic of research. Recent research in food allergy treatment has focused on developing safe and effective therapies, and the most active area of research for food allergy involves immunotherapy5).
Allergen immunotherapy has been used to treat allergic diseases since the early 1900s6). There is no controversy regarding the use of immunotherapy in the treatment of allergic rhinitis and allergic asthma, but the indications for immunotherapy are not well defined for atopic dermatitis or food allergy6). Early studies of subcutaneous immunotherapy (SCIT) in patients with peanut allergy were discontinued owing to a high rate of anaphylactic reactions6). Recently, a hypoallergenic mutant of fish parvalbumin has entered a first safety trial in SCIT for fish allergy7). However, for food allergy, the major forms of immunotherapy are oral immunotherapy (OIT), sublingual immunotherapy (SLIT), and epicutaneous immunotherapy (EPIT)8).
The first successful use of OIT to treat a food allergy was reported in 1908 in a child with severe egg-induced anaphylaxis9). After this first successful trial, no additional trials of OIT for food allergy were reported until Patriarca et al.10) published results of a successful OIT for milk, egg, fish, and orange allergies in 1984. Several studies on immunotherapies for food allergy were reported in the 2000s1112) and significant progress has been made in the field in the past 5 years, particularly with regards to allergen-specific immunotherapies8). Studies on OIT or SLIT in patients allergic to peanuts, milk, and eggs are yielding valuable findings1314151617). Other recent studies include the use of EPIT or OIT with anti-IgE treatment1819).
In this study, protocols, immunologic mechanisms, efficacies, adverse reactions, and detailed practical information according to clinical experiences with OIT, SLIT, and EPIT are reviewed.
Mechanism of action and immunologic changes
With OIT, there is evidence that activation of gut mucosal dendritic cells affects the allergic response through immunomodulation of tissue-resident and circulating effector cells20). The modulation of IgE responses is an important immunologic change in OIT8). Previous OIT studies demonstrated a decrease in the Th2 cytokines such as interleukin (IL)-4, IL-5, and IL-132122), changes in specific IgE amount and diversity232425), and an increase in IgG4212425) and regulatory T (Treg) cell numbers21), particularly in allergen-specific FoxP3 Treg cells21). In addition, suppression of basophils has been observed26). In a mouse model, clinical protection induced by OIT was localized to the gastrointestinal tract and was associated with significant changes in intestinal gene expression27).
The mechanism of action in SLIT involves the interaction of allergens with protolerogenic Langerhans cells in the oral mucosa, resulting in the suppression of an allergic response2829). In addition, significant decreases in allergen-specific basophil activation and skin prick test titrations30) were shown in previous SLIT studies.
Studies on the mechanism of EPIT demonstrate that allergen capture by Langerhans cells in the epidermis results in expression of cytotoxic T lymphocyte-associated antigen 4 by a subpopulation of dendritic cells. These dendritic cells then migrate to regional lymph nodes, leading to the downregulation of effector cell responses293132). Further studies of EPIT indicate that levels of specific IgG2a increased, whereas the overall IgE/IgG2a ratio decreased33), and that ultimately EPIT induces a specific and possibly long-lasting population of Treg cells34). There are currently no biomarkers to predict the response to immunotherapies for food allergy6). However, several studies have indicated that lower levels of specific IgE, as well as basophil activation, reduced skin prick test responses, and higher IgG4 levels are all suggestive of successful treatment2425).
Protocols for OIT
OIT protocols usually involve daily administration of a food allergen mixed with a food vehicle in gradually increasing doses (varying from milligrams to grams) over the course of several months to years5). However, owing to variations in the preparation of food allergens, updosing, maintenance dose, and oral food challenge (OFC) procedures used by diverse research groups, no single established OIT protocol has been shown to be both effective and safe6).
In the United States, OIT protocols for food allergy typically comprise three phases: (1) an initial dose escalation or modified rush desensitization that takes place over 1–2 days with 6–8 doses of the allergen given, (2) a build-up phase that consists of weekly to biweekly dose escalations performed over 6–12 months until a target dose is reached, and (3) a maintenance phase with daily home dosing that occurs over the course of several months or years8). According to the author's experiences with OIT at the Consortium of Food Allergy Research (CoFAR), patients who completed screening tests, such as providing a detailed history, physical examination, serum specific IgE quantification, skin prick test, spirometry, peak flow meter visit research clinic for baseline OFC on day 0. Initial dose escalation begins in the research clinic on day 1, and patients eat their maximum tolerated dose of a food allergen, followed by 2 hours of observation in the research clinic on day 2. Patients continue to eat the same maximum tolerated dose daily at home for 2 weeks. At the end of the 2-week period, patients return to the research clinic to eat the next increased dose. After patients reach the target dose, they continue to eat the same dose daily at home and return for regular follow-up visits at the research clinic (e.g., once every 4 months).
Daily home dosing can be difficult, and young children may refuse to swallow distasteful food allergens. Therefore, food vehicles such as applesauce, pudding, and ice cream are usually recommended for mixing with doses. In the author's experiences using OIT, other creative and attractive food vehicles for successful administration of food allergens include melted peanut powder with banana, a sandwich of two chocolate bars with a filling of melted peanut powder, crackers with peanut extract topping, and gummy bear candies with a peanut powder topping.
The starting doses for patients participating in OIT are selected to be low enough not to cause reactions, and are either chosen for each subject according to a threshold identified in an initial OFC or are fixed for the entire study population35). OFC is used to assess the allergen reactivity threshold during evaluation of clinical desensitization (assessed during therapy) and functional tolerance (assessed while off therapy on a restricted diet)8). In general, the maximum dose used in OIT protocols is higher in the United States than in Europe35). In the United States, daily OIT doses during the maintenance portion of a protocol vary, but are usually in the range of 300–4,000 mg of protein. At the end of the study, participants are encouraged to continue daily consumption of the food allergen16).
In contrast, conventional OIT protocols in Europe include daily administration of the food allergen, with daily to biweekly increases in dose until the maximum tolerated dose is reached. This maximum tolerated dose is then maintained over the study period36). Alternatives to conventional European OIT protocols include rush protocols, in which the food allergen is administered in increasing doses several times per day for several days3738). An Italian study demonstrated that a maintenance regimen with milk given twice weekly was as effective as a regimen requiring daily administration of milk39). In Japan, the most common OIT protocol consists of three steps: (1) an initial build-up phase that occurs while the patient is in the hospital, (2) a slow build-up phase that occurs in the home, and (3) a final maintenance phase40).
Partially defatted peanut flour and dried egg powder are often used as food allergens in OIT procedures. Studies have demonstrated that the allergenicity of commercially available dried egg powder is equivalent to raw egg whites, and that the processing involved in producing dried egg powder does not affect the allergenicity of egg proteins41). In the University of North Carolina OIT program, substances used as food allergens are screened for contamination by mold, yeast, Salmonella spp., Escherichia coli, and aflatoxin using appropriate bioassays. Whole, crushed roasted peanuts were used as a food allergen in a European study22). Diluted whole milk1242) and dry nonfat powdered milk43) have been used in OIT procedures for patients with allergies to milk. Recently, preparation of heated allergens in OIT for milk and/or egg allergy was evaluated based on evidence of temperature-associated changes in protein conformation and reduced IgE binding to heated allergens8). An ongoing CoFAR study comparing the use of traditional OIT and OIT using a baked egg preparation for patients with egg allergies will provide important information about the treatment effects of therapies using heat-treated allergens8). According to the recipe book used in the CoFAR study, patients can eat several foods prepared with baked egg during OIT, including muffins, French toast, meatballs, savory potato bakes, and products prepared using boxed mixes. Wheat powder was used in OIT protocols as a wheat allergen in a Japanese study40), and the efficacy of multiallergen OIT protocols with simultaneous administration of multiple foods are also under investigation8).
During the dose escalation phase of OIT programs, patients are often contacted by phone or e-mail after the first week of home dosing to assess symptoms and compliance. Recently, a Web site-based reporting system incorporating a detailed questionnaire to collect pertinent data, including the dose consumed, the occurrence and details of treatment of adverse reactions, and relevant potential exacerbating factors was developed and used successfully44).
Protocols for SLIT
SLIT involves the administration of small drops of allergen extract (in doses ranging from micrograms to milligrams) under the tongue, which is held for 2 minutes and then swallowed545). SLIT protocols for the treatment of food allergy typically comprise 2 phases: (1) a build-up phase consisting of weekly to biweekly dose escalations administered until a target dose is reached (similar to the build-up phase of OIT), and (2) a maintenance phase with daily home dosing that occurs over the course of months or years45). Unlike OIT protocols, there is no initial escalation phase consisting of the administration of six to eight doses of allergen over a period of 1–2 days. With SLIT protocols, patients are observed for 30 minutes after administration of the dose. If an adverse reaction is observed, the observation time will be extended; otherwise, the patients are discharged.
Doses of food allergens in SLIT are approximately 1,000 times less than those used in OIT protocols5), with daily doses in the maintenance regimen often within the range of 2–7 mg of protein8). Dilutions (e.g., 1/1,000, 1/100, 1/10, and full concentration) of food allergens or the number of pumps such as 1 to 16 times can be changed during the dose escalation phase. SLIT has been utilized for the treatment of patients with several common food allergies, including peanut, milk, kiwi, hazelnut, and peach allergies1415464748). For patients with peanut allergies, peanut extract in a diluent (e.g., glycerin) can be administered. Drops of the peanut extract used in SLIT are flavorless, and most patients treated in the clinic did not complain of a disagreeable taste.
Protocols for EPIT
EPIT involves the application of an allergen-containing patch to the skin surface8). In a 3-month pilot study for the treatment of milk allergy, treatment consisted of three 48-hour applications on the patient's back per week of patches containing skimmed milk powder as the active substance18). In an ongoing CoFAR study of EPIT in children, there is no dose escalation phase as in OIT and SLIT protocols. Instead, graduated application times are used during the first 21 days of therapy. Patches are applied for 24 hours on rotating sites on the intrascapular area of the back. Daily doses during the maintenance regimen in EPIT usually contain 50–500 µg of protein8).
Efficacy of immunotherapy for food allergy
Two immune states can be achieved through food allergen immunotherapy: desensitization and tolerance5). Desensitization occurs when the daily allergen exposure increases the threshold of clinical reactivity to the food and can be lost when daily dosing is discontinued5). Tolerance refers to the ability of the patient to ingest the food allergen without allergic symptoms even after discontinuation of the therapy5).
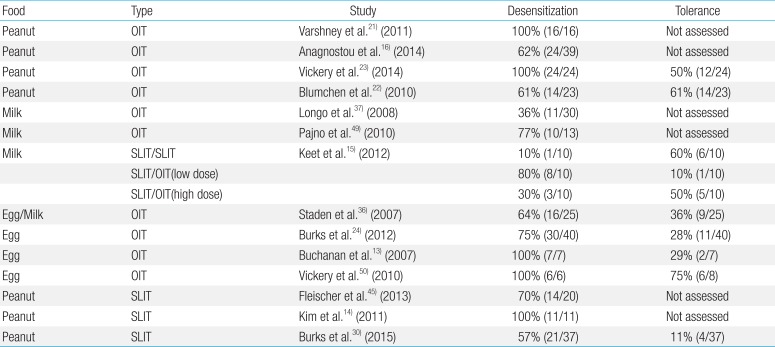
In previous studies, the success rate for desensitization after OIT ranged from 36% to 100%, and the rate of tolerance ranged from 28% to 75% (Table 1)13151621222324374950). Many patients passed an OFC after 1 to 4 years of OIT with a 20- to 100-fold increase in threshold reactivity6). In a meta-analysis of studies on OIT for milk allergy, desensitization is 10.2 times more likely in OIT-treated patients than in non–OIT-treated patients51). Although the lowest rate of desensitization after OIT was reported in a study of severely milk-allergic subjects with a history of anaphylaxis in response to milk ingestion, a recent review article discussed a successful Korean OIT study resulting in the successful desensitization of patients with a history of anaphylaxis following milk exposure52).
To date, available evidence suggests that SLIT is less effective than OIT in inducing desensitization, but has a better safety profile (Table 1)1314151621222324303745495053). A 3-month pilot study of EPIT suggested an acceptable safety profile with encouraging clinical findings18), and multicenter EPIT studies are currently ongoing in the United States and Europe8). Very recently, the first trial evaluating a novel regimen consisting of coadministration of a probiotic with the allergen in an OIT protocol for peanut allergy demonstrated sustained unresponsiveness in 82.1% of patients54).
Adverse reactions and dose adjustment
Adverse reactions in most OIT protocols were localized oropharyngeal symptoms consisting primarily of pruritus and tingling sensations and were easily treated212437). Gastrointestinal side effects, including abdominal pain, cramping, nausea, and vomiting, occurred in 10% to 20% of subjects receiving OIT, and ultimately led to the discontinuation of therapy55). In addition, there are recent reports of the induction of possible eosinophilic esophagitis in some patients56). Studies of OIT in patients with severe milk allergy have shown a higher incidence of adverse reactions than that observed in studies of OIT for other food allergens3740). It is important to note that reactions requiring treatment with epinephrine, such as generalized urticaria/angioedema, wheezing/respiratory distress, laryngeal edema, repetitive emesis, and anaphylaxis, were observed in up to 25% of participants68). It is of particular importance that systemic reactions in OIT participants occurred not only during the dose escalation phase, but also during home administration2157). Therefore, food immunotherapy is not recommended for routine clinical use (level III, grade D). Food immunotherapy procedures should be performed only in highly specialized centers with adequate equipment under the care of expert staff, and in accordance with clinical protocols approved by local ethics committees5859).
Decreased reaction thresholds have been observed during OIT protocols when doses are ingested by patients with concurrent illness, uncontrolled asthma, during menses, or in those patients who engage in physical exercise shortly after dosing60). In a long-term follow-up study, patients who had completed OIT and passed a tolerance OFC reported limiting milk consumption due to symptoms related to exercise (25%) and illness (6%)61). Therefore, temporary discontinuation of OIT during acute illnesses is recommended22). If fewer than 3 doses are missed, patients may resume dosing at home60). However, if 3 to 5 doses are missed, patients resume dosing at the research clinic. If more than five doses are missed, significant dose reduction or repeat desensitization may be required60). Asthma and allergic rhinitis should be well controlled and closely monitored60). In patients with exercise-induced symptoms, activity should be limited for 2 hours after dosing. In addition, patients should be closely monitored during administration of doses during their menstrual cycle, particularly when menses are coupled with infection or exercise. Food ingestion before dose administration decreases the frequency of adverse reactions; therefore, patients are advised to take their daily OIT dose with a meal or snack60).
To improve the safety profile of immunotherapies for food allergy, SLIT, EPIT, and adjunct administration of recombinant monoclonal anti-IgE therapy during OIT have been tested. Omalizumab treatment before and during OIT has been associated with a reduction in adverse events and reduced time to the target dose in some studies19). In studies of SLIT for food allergy, side effects, primarily oropharyngeal, were minimal, and treatment was not commonly required9). While 90% of participants in an EPIT study experienced mild or moderate local adverse reactions, systemic reactions were mild and transient, with no severe adverse events and no administration of epinephrine required62).
Conclusions
Patients with food allergy are at risk of potentially life-threatening reactions resulting from accidental ingestion of food allergens. Allergen avoidance and self-injectable epinephrine, the current standard of treatment for food allergy, do not change the natural course of food allergy. Recent studies have explored the efficacy of immunotherapies such as OIT, SLIT, and EPIT in the treatment of food allergy. Different research groups have used diverse protocols for the preparation of food allergens, dose escalation, maintenance dose regimens, and OFC procedures, and no single, established protocol has been demonstrated to be both effective and safe.
Recent studies in food allergen immunotherapies have reported successes in desensitization and tolerance, and some mechanisms underlying immunologic changes after immunotherapy have been revealed. In studies of OIT, adverse reactions were usually localized, but severe systemic reactions were observed in certain populations. Studies of SLIT have demonstrated minimal side effects, but overall efficacy is lower than that seen with OIT. Clinical findings from a pilot EPIT study are encouraging. Although immunotherapy shows promise as an effective therapy for food allergies, additional studies to increase treatment safety and demonstrate long-term tolerance are needed before immunotherapy can be used as a routine treatment for food allergies.
Acknowledgments
This work was supported by a grant from Inje University, 2008. Thanks to all the members of the food allergy research team at the University of North Carolina Hospital, who helped the author gain clinical experience in the use of immunotherapies for the treatment of food allergy.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.