Apparent life-threatening event in infancy
Article information
Abstract
An apparent life-threatening event (ALTE) is defined as the combination of clinical presentations such as apnea, marked change in skin and muscle tone, gagging, or choking. It is a frightening event, and it predominantly occurs during infancy at a mean age of 1–3 months. The causes of ALTE are categorized into problems that are: gastrointestinal (50%), neurological (30%), respiratory (20%), cardiovascular (5%), metabolic and endocrine (2%–5%), or others such as child abuse. Up to 50% of ALTEs are idiopathic, where the cause cannot be diagnosed. Infants with an ALTE are often asymptomatic at hospital and there is no standard workup protocol for ALTE. Therefore, a detailed initial history and physical examination are important to determine the extent of the medical evaluation and treatment. Regardless of the cause of an ALTE, all infants with an ALTE should require hospitalization and continuous cardiorespiratory monitoring and evaluation for at least 24 hours. The natural course of ALTEs has seemed benign, and the outcome is generally associated with the affected infants' underlying disease. In conclusion, systemic diagnostic evaluation and adequate treatment increases the survival and quality of life for most affected infants.
Introduction
It is not uncommon for clinicians to meet anxious parents in the Emergency Department (ED) who are frightened by the abrupt changes in the health of their baby. Since the 1970s, there were reports about episodes occurring in infants characterized by an acute and unexpected change in conduct, either with or without apnea. These episodes were mentioned to as "near-misses" for sudden infant death syndrome (SIDS)1), and were thus believed to be a possible cause of SIDS. However, in recent times, these episodes have been defined as apparent life-threatening events (ALTEs)2). ALTEs are an ongoing challenge for clinicians because these events have vague and heterogeneous clinical presentations.
Definition
SIDS is defined as the sudden death of an infant <1 year of age, where there is no explanation for death even after thorough investigations including: complete autopsy, examination of the death scene and review of the clinical history3). In contrast, the diagnosis of an ALTE is based on symptomatology rather than pathophysiology. In 1986, the National Institutes of Health consensus conference defined an ALTE as "an episode that is characterized by some combination of apnea (centrally or occasionally obstructive), color change (usually cyanotic or pallid, but occasionally erythematous or plethoric), marked change in muscle tone (usually marked limpness), choking, or gagging2).
Up to now, it has not been confirmed that ALTEs are really near-miss SIDS events. Many experts do not accept the association between ALTEs and SIDS. The lack of association between ALTEs and SIDS is supported by the following facts: (1) the incidence of SIDS has decreased since the 1994 "Back to Sleep Campaign", whereas the incidence of ALTEs has not; (2) half of ALTEs occur during wakefulness, whereas SIDS occurs mainly during sleep; (3) apnea and bradycardia events in ALTEs are less common during the early morning hours, when SIDS tends to occur; (4) apnea and bradycardia events are more common in Asians who are at lower risk for SIDS; (5) the age of mothers whose infants die of SIDS is younger compared with the age of mothers whose infants experience an ALTE; (6) incidence of ALTEs is equally distributed between boys and girls, whereas SIDS occurs more frequently in boys45).
Epidemiology
ALTEs occur predominantly in infancy at a mean age of 1–3 months4), and equally between boys and girls5). The incidence of ALTE was reported as 0.6–2.46 per 1,000 live births, 0.6%–1.7% of all ED visits for infants younger than 1 year of age, and 0.5%–6% of all infant visits56789). The actual prevalence of ALTE may be higher than these figures. ALTE is associated with a 0%–7.6% mortality rate25).
Clinical presentation
ALTE is a diagnostic term based on clinical presentation. However, infants who experience an ALTE are often asymptomatic upon arrival at the hospital. Therefore, the first important step is to determine whether the individual symptoms qualify as ALTE criteria. In regards to the symptoms of apnea, shallow breathing, short episodes of central apnea lasting less than 30 seconds, and periodic breathing of the newborn could be normal events, if they are not associated with cardiac instability. Cyanosis, flushing, or acrocyanosis could also be reflective of normal changes in perfusion5).
Some infants with an ALTE often appeared healthy when they arrived at the ED or outpatient department, while other infants required immediate cardio-pulmonary resuscitation. This heterogeneity of ALTE presentation makes it difficult for clinicians to decide on how to assess and manage infants with an ALTE.
Evaluation
1. History
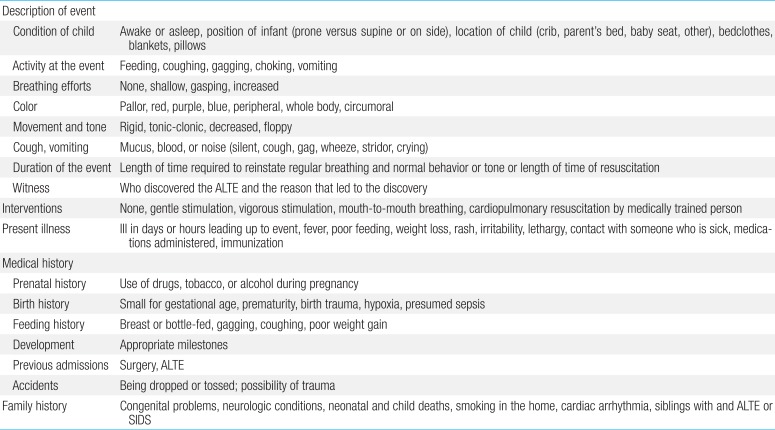
It is essential that a very thorough and detailed history is provided by a witness. We can assess the severity of the event and the underlying diagnosis by reviewing the patient's history. Caregivers may overestimate or underestimate the events because of their anxiousness after frightening events. The collected information should contain the following facts in Table 11011).
2. Physical examination
Infants may have no signs or symptoms of significant illness after an ALTE. When infants with ALTE underwent physical examination by paramedics in the prehospital setting, 83% of the inants had no abnormal findings, 13.3% showed mild distress, and 3.3% showed moderate distress12). Infants who had abnormal findings during the initial clinical examination after an ALTE were more likely to have either recurrent ALTE or a definitive diagnosis7).
A physical examination should include the review of general appearance, vital signs, weight, height, and head circumference measurements. We need to be observant for neurological, respiratory, or cardiac abnormalities during the examination.
3. Further evaluation
Further evaluation of the patient with an ALTE is determined on the basis of their initial history and physical examination. There is no standard workup protocol, and the clinician should decide on the appropriate investigations depending on the circumstances of each individual case. The diagnostic procedures for ALTE infants are summarized in Table 21011), and it is only a guideline for clinicians to refer to.
Tieder et al.13) demonstrated that tests for gastroesophageal reflux (GER), neurologic/hematologic/metabolic abnormalities, infections, ingestions of toxic materials, and cardiac dysrhythmias were the most frequently performed. In 2009, the Dutch Pediatric Association offered the first evidence-based consensus pathway for the diagnosis, management, and follow-up of children with an ALTE14). They recommend initial diagnostic tests for ALTEs that include the following: complete blood cell count with differential count, C-reactive protein, serum glucose, arterial blood gas analysis, urine analysis, electrocardiography, and assessments for seasonal virus such as Bordetella pertussis and respiratory syncytial virus (RSV). These tests are relatively inexpensive, sensitive, specific, and easy to perform. However, there is large inter-hospital diversity for the care of ALTE, including the costs of care.
Underlying etiology
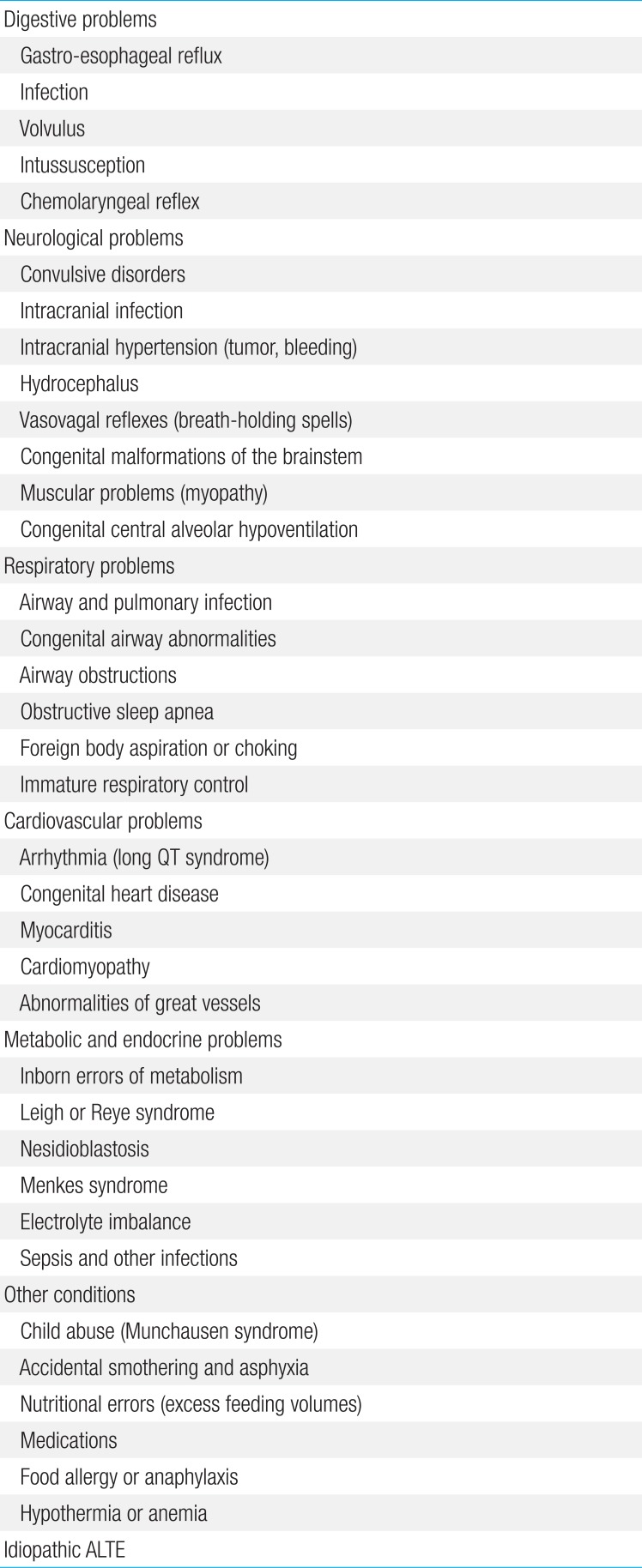
There are several potentially dangerous or treatable conditions associated with ALTEs. The causes of ALTEs are divided into problems that are: gastrointestinal (GI) (50%), neurological (30%), respiratory (20%), cardiovascular (5%), metabolic and endocrine (2%–5%), and others such as child abuse (Table 3)101115).
1. Digestive problems
The most common diagnosis is GI disease, including GER. However, an important consideration is that half of all normal infants aged 0–3 months may have daily regurgitation, so caution should be exercised before concluding GER to be a final diagnosis of an ALTE516). Upper GI series is neither sensitive nor specific17). The gold standard used in the diagnosis of GER is the 24-hour esophageal pH test, because it can demonstrate an association between GER and ALTEs. In addition, the intraluminal impedance helps to identify nonacid gastric reflux. However, these tests for GER are uncomfortable for infants and relatively expensive. Therefore, routine GER testing is not recommended for all infants with an ALTE18). GER tests should be considered for infants with: a history of frequent GER, an ALTE that occurs during or immediately after feeding, or gastric contents in their mouth of nose during an ALTE10).
2. Neurologic problems
Seizure is the most common neurologic disorder associated with ALTEs. Although electroencephalography (EEG) is first choice investigation for seizure, the sensitivity of EEG for diagnosing epilepsy is only 15%. Only 3.6% of infants with an ALTE were diagnosed with chronic epilepsy and in 71% of ALTE cases, a recurrent ALTE occurred within 1 month19). Thus, the use of EEG is considered for the evaluation of infants with recurrent ALTEs15). If EEG recordings are nondiagnostic, repeated EEGs or analysis of clinical history is important for diagnosing seizure20). Neurologic imaging, including cranial computed tomography (CT), magnetic resonance imaging, diffusion weighted imaging, and ultrasonography can help to diagnose chronic epilepsy, but it has a low sensitivity4).
One of notable cause of an ALTE is breath-holding spells, which typically have an emotional precipitant and usually occur while awake, and crying21). A rare cause of ALTEs is congenital central hypoventilation syndrome which usually occurs during sleep.
3. Respiratory problems
Obstructive sleep apnea, in association with anatomical abnormalities, infections, allergies or medications can induce ALTEs. Obstructive sleep apnea frequently occurs in premature babies, and obstructions are usually developed at the laryngeal level22). One of the common respiratory causes of ALTEs is infection, especially bronchiolitis caused by RSV23). An recent study showed that the age-group at high risk for apnea is: <1 month for full-term babies, and <48 weeks after conception for preterm babies24). Pertussis has been also identified as a cause of ALTEs7).
4. Cardiovascular problems
Cardiovascular problems are divided into 2 categories; structural heart disease and structurally normal hearts with arrhythmia, myocarditis, or cardiomyopathy. Electrocardiography is the important initial test for infants with an ALTE, and 24-hour continuous Holter monitoring can provide additional information for arrhythmias, such as long QT syndrome or paroxysmal tachycardia25).
5. Metabolic and endocrine problems
ALTEs can be an initial presentation of metabolic disorders. Clinicians should suspect an inborn error of metabolism if a patient with an ALTE has: (1) an atypical age (>1 year), (2) a failure to thrive, developmental delay, or seizures, (3) a family history of ALTEs, seizure disorders or SIDS, (4) laboratory abnormalities such as hyperammonemia, hypoglycemia, metabolic acidosis, elevated liver enzymes, or abnormal hemostasispatient1015). Various metabolic abnormalities have been reported, including anomalies of mitochondrial fatty acid oxidation (medium chain acyl-CoA dehydrogenase deficiency), urea cycle defects (arginase deficiency), organic acidemias, and galactosemias2627). Serum chemistry tests, including tests for sodium, potassium, urea, calcium, magnesium, ammonia, lactate, and pyruvate are inexpensive and simple, or sole diagnostic tools in some cases. Hence, we recommend these tests for the initial evaluation of ALTE.
Among the several infectious causes of ALTE, the prevalence were reported to be about 9%–82% for bronchiolitis, 0%–10% for lower respiratory tract infection, 0%–7.6% for urinary tract infection, 0%–2.5% for bacteremia, and 0%–1.6% for meningitis28293031).
6. Other conditions
One of most difficult and challenging diagnoses in infants with an ALTE is nonaccidental trauma. Although only less than 3% of ALTEs are related to child abuse21), the mortality associated with child abuse is high32). A clinician should keep in view the possibility of child abuse such as shaken baby syndrome and Munchausen by proxy. Several factors that may suggest abuse are recurrent ALTEs: previous occurrences of SIDS, fresh blood in the nose or mouth, delay in seeking medical care, a confusing or changing history, and the need for vigorous resuscitation during events33). A funduscopic examination should be included in the initial examination for retinal hemorrhage, and covert video surveillance can be used in suspicious cases3435). Neurologic imaging, such as head CT can be used to identify head trauma, and should be considered for suspicious cases of abuse, to avoid unnecessary irradiation34).
Management
1. Criteria of admission
One study found that 13.6% of ALTEs had a subsequent extreme event, 85% of which occurred within the first 24 hours of hospitalization37). In another prospective study, 12% of infants had recurrent episodes within 24 hours in hospital, 9% required moderate stimulation, and 3% required resuscitation38). In a Korean study, Choi and Kim39) found that repeated ALTEs occurred in 69% of in-hospital infants that have experienced an ALTE. Therefore, regardless of the cause of the ALTE, all infants with an ALTE should require hospitalization, continuous cardiorespiratory monitoring and evaluation within at least 24 hours. The admission rate for ALTEs is usually 75%–100%33363740), which follows the recommendations of many centers. However, in some countries, the hospital charges cannot be ignored. Mittal et al.36) proposed a clinical decision rule and identified the risk factors for hospitalization: prematurity, cyanosis, abnormal findings at initial examination, and the absence of a history of choking and upper respiratory infection (URI) symptoms. Also, other studies suggested that the major indicators of admission and further evaluation were prematurity, an age <30 days or >60 days, history of combined underlying illnesses, multiple ALTEs occurring within 24 hours, and an abnormal result in the initial examination73340). In Korea, the economic burden of admission is relatively low, so we strongly recommend that all infants with an ALTE should be admitted within 24 hours.
2. Treatment for individual causes
Appropriate medical or surgical treatment should be conducted for a specific cause of an ALTE. If GER is diagnosed as cause of an ALTE, interventions for GER such as feeding management, antireflux drugs, and surgical intervention may resolve further events11).
3. Education of caregivers
It is also important to educate the families. All caregivers of infants with an ALTE should be informed about preventative and emergency management (such as standard cardiopulmonary resuscitation techniques) for further episodes10). For prevention of an ALTE, safe sleep position (including the supine position, with the face free, in an adequately heated room) and avoiding exposure to tobacco smoke will be beneficial41).
4. Home monitoring
Cardiorespiratory monitors are the preferred devices for apnea monitoring. Although the effect of oxygen saturation monitoring alone is controversial, oxygen monitors have been used as an alternative to cardiorespiratory monitoring424344). Home cardiorespiratory monitors help to alert caregivers to apnea and bradycardia. However, there is no evidence that apnea monitoring can prevent SIDS after an ALTE. Routine monitoring of all infants with an ALTE is not generally recommended. Although there are no accepted criteria to determine which patient should be home monitored, some publications recommended home monitoring for infants with an idiopathic ALTE or those who needed vigorous resuscitation4245). Moreover, monitoring may be considered for infants with airway abnormalities (upper airway malformation or tracheostomy), idiopathic dysfunction of their respiratory center (CCHS), and chronic lung disease requiring oxygen supplementation and mechanical airway support4246).
During home monitoring, continuous medical, psychological, and technical support will be needed for infants with ALTE and their caregivers. Home monitoring is usually stopped after a 6-week event-free period. For a preterm infant, usually it may be discontinued after 46 weeks' postmenstrual age4246).
5. Follow-up
Recurrent ALTEs tend to occur during the first month after discharge4647). Kant et al.48) reported that the mortality rate after discharge was 1.1% (2 deaths/174 infants) during 34 months of follow-up, and 2 cases of death occurred within 15 days of discharge. The other study of ALTE recurrence showed that 71% of the infants with an initial ALTE revisited the hospital with a second event within 1 month. Therefore, infants with an ALTE should be followed up at least within a month after discharge.
Prognosis and risk factors (for significant disease)
Recently, the natural course and prognosis of ALTEs has been more benign42), and the outcome usually depends on the associated underlying disease49). For infants with an idiopathic ALTE, the outcome is unpredictable10). In previous studies of ALTE prognosis after discharge, the mortality rate was reported to be 0%–1.1% during 12–60 months of follow-up619334850). However, Oren et al.51) reported that the risk of death was over 25% for infants in high-risk groups of ALTE, such as in cases where: (1) the events occurred during sleep, (2) resuscitation was needed, (3) there were recurrent episodes, (4) the infants were siblings of SIDS infants, and (5) the patient had a seizure disorder.
Many studies have investigated potential predictors of subsequent adverse events in infants with an ALTE, and they are similar to those for the indication that the patient was admitted to hospital. The most commonly mentioned risk factors are a history of prematurity and multiple ALTEs333740). Some reports showed that infants with an age <30 days or infants that were born <43 weeks after conception were more likely to experience subsequent events3740). In contrast, other studies found that an age >2 months was a factor that was associated with higher risk of recurrent ALTEs733). In regards to URI symptoms, one study reported an increased risk of subsequent ALTEs in infants that have URI symptoms37), whereas another study reported that there were more cases of investigation for ALTEs in infants with no URI symptoms, compared with the infants with URI symptoms36). In a Korean study conducted by Choi and Kim39), it was found that the infants with ALTEs that occurred during wakefulness and with URI symptoms had a higher risk of significant intervention.
Most infants with an idiopathic ALTE showed normal development during preadolescence52). However, some reports found that 4.9%–7.1% 4 of infants with ALTE developed adverse neurological outcomes, including chronic epilepsy and developmental delays1953). In a Korean study, 15.4% of the infants showed developmental abnormalities during the 6-month follow-up period39). Inpatient neurologic evaluation of infants with a first ALTE has low sensitivity for adverse neurologic outcomes, and perinatal characteristics, birth status, recurrent apnea, and family history of seizures may be correlated with growth and developmental outcomes1954). Long-term follow-up may be decided on an individual-case basis according to the underlying status of the infants.
Conclusions
Considering that ALTEs include a wide range of clinical presentations, ALTEs are an ongoing diagnostic dilemma for clinicians. A thorough, detailed history, and physical examination are the most important aspects of patient evaluation, and the clinician should decide appropriate further investigations on an individual-case basis. We recommend that all infants with an ALTE undergo inpatient clinical observation and evaluation, with at least 24 hours of cardiorespiratory monitoring. In addition, infants with an ALTE should be followed up at least within a month after discharge. The use of home monitoring and long-term follow-up activities should be decided on an individual basis according to the underlying status of the infants.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.