Enterovirus 71 infection and neurological complications
Article information
Abstract
Since the outbreak of the enterovirus 71 (EV71) infection in Malaysia in 1997, large epidemics of EV71 have occurred in the Asia-Pacific region. Many children and infants have died from serious neurological complications during these epidemics, and EV71 infection has become a serious public health problem in these areas. EV71 infection causes hand, foot and mouth disease (HFMD) in children, and usually resolves spontaneously. However, EV71 occasionally involves the central nervous system (CNS), and induces diverse neurological complications such as brainstem encephalitis, aseptic meningitis, and acute flaccid paralysis. Among those complications, brainstem encephalitis is the most critical neurological manifestation because it can cause neurogenic pulmonary hemorrhage/edema leading to death. The characteristic clinical symptoms such as myoclonus and ataxia, cerebrospinal fluid (CSF) pleocytosis, and brainstem lesions on magnetic resonance imaging, in conjunction with the skin rash of HFMD and the isolation of EV71 from a stool, throat-swab, or CSF sample are typical findings indicating CNS involvement of EV71 infection. Treatment with intravenous immunoglobulin and milrinone are recommended in cases with severe neurological complications from EV71 infection, such as brainstem encephalitis. Despite the recent discovery of receptors for EV71 in human cells, such as the scavenger receptor B2 and P-selection glycoprotein ligand 1, it is not known why EV71 infection predominantly involves the brainstem. Recently, 3 companies in China have completed phase III clinical trials of EV71 vaccines. However, the promotion and approval of these vaccines in various countries are problems yet to be resolved.
Introduction
Enterovirus 71 (EV71) is one of the main causative pathogens of hand, foot and mouth disease (HFMD). Since EV71 occasionally involves the central nervous system (CNS) and can causes serious and potentially fatal neurological complications, it has emerged as a major concern among pediatric infectious diseases, particularly in the Asia-Pacific region12). EV71 is a single-stranded RNA virus that belongs to the human enterovirus A species of the Picornaviridae family. EV71 was first identified in California in 1969 and described by Schmidt et al. in 19743). Epidemic outbreaks with high mortality rates occurred in Europe in the 1970s (Bulgaria in 1975 and Hungary in 1978)45). The first major EV71 outbreak in the Asia-Pacific region occurred in 1997 in Malaysia and caused 41 child deaths6). Since then, large-scale epidemics of EV71 have been reported in many Asia-Pacific countries including Taiwan, Australia, China, Singapore, Vietnam, and Cambodia, and have caused many fatalities7891011121314). In 1998, a major epidemic of EV71 in Taiwan caused 1.5 million infections, 405 with severe neurological complications, and 78 child deaths78). More than 7 million HFMD cases and 2,457 deaths were reported in China during EV71 epidemics between 2008 and 2012910). Recently, EV71 epidemics have been reported in the USA and European countries outside the Asia-Pacific region, such as the Netherlands, France, Norway, the UK, Hungary, and Greece15161718192021). In Korea, epidemics of EV71 infection occurred between 2009 and 2013 and included fatal cases. According to one report22), which compared the viral pathogens and clinical features of HFMD between 2008 and 2009 in Korea using data from a nationwide surveillance system, the main causative viruses were coxsackievirus A10 and echovirus 30 in 2008, whereas the chief pathogen in 2009 was EV71. During this period, the prevalence of accompanying meningoencephalitis increased considerably, from 4.0% to 15.2%. The main subgenotype of EV71 detected during 2009 and 2012 in Korea was C4a, which is nearly identical to the EV71 genotype detected in China in 200823).
In this review, the author will discuss the clinical features and neurological manifestations of EV71 infection, focusing on brainstem encephalitis, the magnetic resonance imaging (MRI) findings for neurological complications, the pathophysiology, diagnosis, treatment, and prognosis for EV71 infection with CNS involvement, and the development of new vaccines.
Clinical features of EV71 infection
As mentioned above, EV71 infection causes HFMD in children, and this usually resolves spontaneously. However, EV71 can cause more severe neurological complications compared with other enterovirus serotypes, including brainstem encephalitis and acute flaccid paralysis224). According to clinical studies conducted in northern Taiwan252627), symptomatic EV71 infection is divided into 4 stages: HFMD/herpangina (stage 1), CNS involvement (stage 2), cardio¬pulmonary failure (stage 3), and convalescence (stage 4). Most EV71 cases remain at stage 1, some progress to stage 2, and a few advance to the most severe condition, stage 3. Some survivors of stage 3 have long-term sequelae during convalescence (stage 4).
The majority of patients with neurological complications of EV71 infection have been under the age of 5 years2829). The peak seasons for the disease are late spring to summer, although infections occur with high incidence throughout the year in tropical areas. The patients usually have a high fever above 38℃, unlike HFMD caused by other enterovirus serotypes such as coxsackievirus A1630). Neurological symptoms or signs appear within 3 to 5 days after the onset of fever or skin lesions31). Some patients show neurological manifestations without the skin or oral mucosal lesions typical of HFMD2). Therefore, during EV71 epidemics, the neurological complications of EV71 infection should always be considered in children who develop neurological diseases, even when patients show no skin lesions characteristic of HFMD. EV71 can be transmitted via contaminated hands; either directly from vesicles on the hands, secretions from the oropharynx, or feces32). The EV71 transmission rate to household contacts is approximately 50%27). Transmission rates are approximately 80% between siblings and cousins33). A total of 50% of infected adults are asymptomatic, but infected adults often spread the disease to preschool children. It is estimated that approximately 0.2%–1% of children with EV71 infection develop neurological complications34).
Neurological manifestations of EV71 infection
1. Brainstem encephalitis
Brainstem encephalitis is the most common neurological presentation, accounting for 58% of neurological manifestations, followed by aseptic meningitis (36%), and brainstem encephalitis with cardiorespiratory dysfunction (4%)29). Despite the recent discovery of receptors for EV71 in human cells3536), the reason for the predominant involvement of the brainstem in EV71 infection is currently unknown. EV71 brainstem encephalitis occasionally induces autonomic dysfunction, such as fluctuating blood pressure and pulmonary hemorrhage/edema (Fig. 1). Most deaths caused by pulmonary hemorrhage in patients with EV71 brainstem encephalitis usually occur within 24 hours after admission because the disease rapidly progresses to the critical stage237). Therefore, early diagnosis of EV71 infection with neurological involvement and prompt, appropriate management is crucial. EV71 brainstem encephalitis has been defined as an illness characterized by myoclonus, ataxia, nystagmus, oculomotor palsies, and bulbar palsy, and various combinations of these, with or without confirmation by neuroimaging, in conjunction with virus isolation from at least one site (throat swab, stool, cerebrospinal fluid [CSF], or other)2938). According to one Taiwanese report, the most prominent neurological presentations for EV71 CNS involvement are myoclonic jerk (68%), vomiting (53%), ataxia (35%), and tremor (21%)29). Myoclonus in patients with EV71 brainstem encephalitis occurs during wakefulness and deep sleep, as well as during light sleep, and may appear very frequently, unlike sleep myoclonus3039). Myoclonus is not only the most common symptom, but also an early indicator of brainstem involvement in EV71 infection224). However, physicians and parents often overlook myoclonus as a nonspecific symptom of febrile illnesses in children with HFMD due to EV71 infection, which may possibly lead to the misdiagnosis of brainstem encephalitis as a benign condition. Hence, all patients with suspected EV71 infection should be carefully observed for all clinical symptoms, including myoclonus and ataxia that are the characteristic clinical features of brainstem encephalitis. Ataxia is also a frequent neurological feature in EV71 brainstem encephalitis2429). Although ataxia has been sometimes reported as a main clinical feature of acute cerebellar ataxia due to EV71 infection29), it more often appears together with other clinical features of brainstem encephalitis, such as myoclonus and tremor29). In addition, patients with EV71 brainstem encephalitis frequently reveal concurrent lesions of the cerebellum and brainstem on brain MRI.
2. Aseptic meningitis
Aseptic meningitis is also a main neurological presentation in EV71 infection. Some studies have noted that aseptic meningitis is the most common neurological complication of EV71 infection3040), although many other studies have reported brainstem encephalitis as the most common neurological complication2429). Aseptic meningitis from EV71 is clinically indistinguishable from that of other viruses that present with headache, fever, and recurrent emesis without any other neurological manifestations. Although EV71 aseptic meningitis is usually considered a more benign condition compared with brainstem encephalitis, patients with clinical aseptic meningitis from EV71 infection may show brainstem lesions on MRI31).
3. Acute flaccid paralysis
Acute flaccid paralysis is also one of the major presenting features among several neurological syndromes caused by EV71 infection, along with brainstem encephalitis and aseptic meningitis. It usually presents like poliomyelitis with acute motor weakness of the extremities, but unlike poliomyelitis, the recovery rate is relatively high2). Guillain-Barré syndrome and transverse myelitis have also been reported in patients with acute motor weakness of the extremities and EV71 infection9).
MRI findings of neurological complications
The characteristic MRI findings of EV71 brainstem encephalitis are high signal intensities on T2-weighted and fluid-attenuated inversion recovery images in the posterior region of the pons, medulla oblongata, midbrain, and bilateral dentate nuclei of the cerebellum (Fig. 2), although MR images may show normal findings241). Rarely, some MRI reports have demonstrated the involvement of the cerebral cortex, subcortical white matter, thalamus, putamen, corpus callosum, and hippocampus instead of the brainstem in patients with EV71 infection42434445). Although the clinical features are positively correlated with the MRI findings4144), they are not necessarily consistent31). In patients with acute flaccid paralysis, MRI typically shows high-signal lesions in the anterior horn cells of the spinal cord on T2-weighted images, and contrast enhancement in the ventral root on T1-weighted images (Fig. 3)4344).
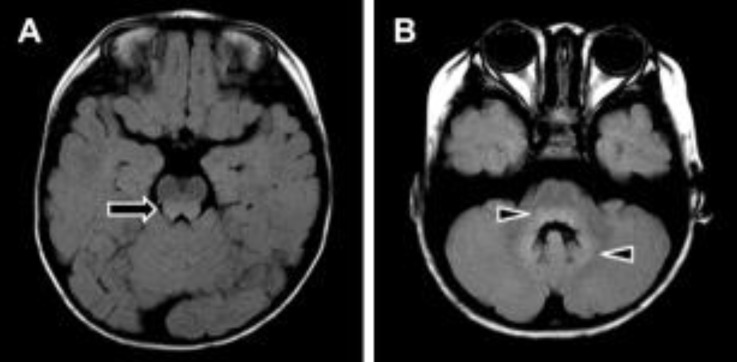
Brain magnetic resonance imaging findings in a patient with enterovirus 71 brainstem encephalitis. (A) Note the high signal-intensity lesion in the posterior aspect of the midbrain (arrow). (B) Note the high signal-intensity lesion in the posterior aspect of the pons and the bilateral dentate nuclei of the cerebellum (arrowheads).
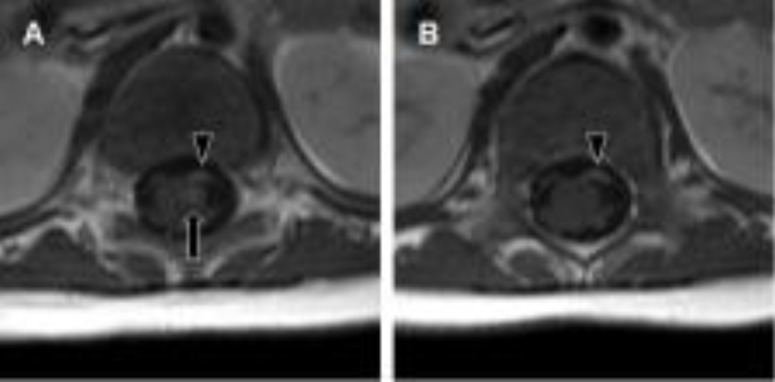
Spine magnetic resonance imaging findings in a 4-month-old infant. The patient presented with acute motor weakness of the left lower extremity along with enterovirus 71 infection. (A, B) Note the strong enhancement of the left anterior horn of the spinal cord (arrow) and the left ventral nerve roots (arrowhead) on gadolinium-enhanced T1-weighted images.
Pathophysiology of pulmonary hemorrhage/edema in EV71 brainstem encephalitis
Pathophysiologically, pulmonary hemorrhage/edema in EV71 brainstem encephalitis results from injury to the vasomotor center of the brainstem24), which increases sympathetic outflow, and vasoconstriction leads to a shift of blood from the highly resistant systemic circulation to the less-resistant pulmonary circulation. Hydrodynamic studies of patients with pulmonary edema have demonstrated normal cardiac function and normal pulmonary hydrostatic pressure24). Pathology studies revealed no necrosis or calcification in the myocardium24). Meanwhile, some studies have shown that the serum and CSF levels of proinflammatory cytokines (interleukin [IL]-6, tumor necrosis factor-α, IL-1β, and interferon-γ) are significantly higher in patients with brainstem encephalitis accompanied by pulmonary edema than in those with uncomplicated brainstem encephalitis464748). These findings suggest that pulmonary hemorrhage/edema might be the result not only of direct hydrostatic force by systemic vasoconstriction resulting from brainstem injury, but also increased pulmonary vascular permeability caused by a systemic inflammatory response.
Recently, several molecules that act as cell surface receptors for EV71 have been identified, such as scavenger receptor B2 (SCARB2), P-selection glycoprotein ligand 1 (PSGL-1), annexin II (Anx2), sialylated glycan, and heparan sulfate353649). SCARB2 plays major roles in attachment, viral entry, and uncoating, and it can enable effective EV71 infection35). In addition, SCARB2 plays key roles in the development of EV71 neurological disease in vivo. PSGL-1, Anx2, sialylated glycan, and heparan sulfate are attachment receptors, which potentiate viral infection3649). However, despite the discovery of these receptors, the reason for EV71 neurotropism on the brainstem is still unknown. A study using an orally infected EV71 murine model has suggested that EV71 enters the CNS via the active retrograde axonal-transport system50). This implies the probability that mechanisms other than receptors for EV71 elicit EV71 brainstem encephalitis.
Virological diagnosis
Although the gold standard for the diagnosis of enterovirus infection is virus isolation via viral culture, this takes more than 7–10 days, and nowadays a molecular serotyping approach is usually employed for the virological diagnosis of EV71 using polymerase chain reaction and sequencing of the VP1 gene2). In patients with neurological complications, isolation of the virus from CSF is the most ideal approach for diagnosing EV71 infection. However, the detection rate for EV71 in CSF obtained from patients with neurological disease is very low (0%–5%)2). EV71 is isolated mainly from throat or stool specimens, and occasionally from skin-vesicle fluid, rather than CSF234). A Taiwan study showed that EV71 can be detected in the throat up to 2 weeks after recovery from HFMD or herpangina, and can be detected in stool samples up to 11 weeks after recovery51). Nevertheless, CSF examination is essential in patients with EV71 infection who have suspected CNS involvement to identify the presence not only of the virus but also pleocytosis in the CSF. A mild lymphocytic pleocytosis of 10–100 cells per µL is typical, although occasionally pleocytosis is not observed231).
Treatment and prognosis
Regarding the treatment of EV71 infection, antiviral therapy is currently ineffective despite efforts to develop new antiviral agents52). A disease-management program developed in Taiwan in 2000 recommended the use of intravenous immunoglobulin and milrinone for the treatment of EV71 brainstem encephalitis24). Intravenous immunoglobulin therapy provides neutralizing antibodies, decreases sympathetic outflow, and attenuates cytokine production. If the patient has a persistent heart rate of more than 180/min and even a high blood pressure, milrinone can be administered simultaneously24). Milrinone is a drug for congestive heart failure, and has both inotropic and vasodilator properties53). Milrinone also has anti-inflammatory effects54). A recent prospective, open-label, randomized controlled study demonstrated that patients who were treated with intravenous milrinone (0.5 µg/kg/min) and intravenous immunoglobulin had a lower 1-week mortality rate compared with patients who were treated with dopamine or dobutamine and intravenous immunoglobulin (18.2% vs. 57.9%)55).
CNS involvement with cardiopulmonary failure is associated with a high mortality rate (about 30%–40%) during the acute stage of the infection2656). In regard to the long-term outcome, one study conducted follow-up of 142 children after EV71 infection with CNS involvement, including 28 cases of cardiopulmonary failure (median follow-up of 2.9 years), and showed that CNS involvement with cardiopulmonary failure is associated with neurological sequelae (limb weakness and atrophy in 64% of patients, and a requirement for tube feeding in 61% and ventilator support in 57%), delayed neurodevelopment (75% of patients), and reduced cognitive function. By contrast, only 1 of 20 children (5%) with CNS involvement without cardiopulmonary failure showed delayed neurodevelopment57).
Development of new vaccines
Recently, 3 companies have completed phase III clinical trials of inactivated EV71 whole-virus vaccines. More than 30,000 infants and children aged 6–71 months from 3 different regions of China were included in those clinical trials585960). The results demonstrated the high safety and immunogenicity of the EV71 vaccines. Protective efficacies were over 90% for EV71-associated HFMD and over 80% for serious EV71-associated diseases585960). The most common adverse reaction was fever. There were no critical vaccine-associated side effects or immunopathological responses during the study period585960). Despite the development of new vaccines, the promotion and approval of these vaccines in various countries are problems yet to be resolved.
Conclusions
Epidemics of EV71 infection have caused many fatalities from serious neurological complications in the Asia-Pacific region since 1997, and have become a serious public health problem in these areas. Among the diverse neurological complications of EV71 infection, brainstem encephalitis is the most critical neurological manifestation, because it can cause pulmonary hemorrhage leading to death. During EV71 epidemics, the neurological complications of EV71 infection always should be considered in the differential diagnosis in children with neurological diseases. Early diagnosis and treatment with intravenous immunoglobulin and milrinone can reduce mortality and morbidity in patients with CNS involvement relating to EV71 infection. Recently, phase III clinical trials of 3 new EV71 vaccines were completed in China. However, it seems to take time for the promotion and approval of these vaccines to take effect in various countries.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
