Endovascular stenting of tracheoinnominate fistula after tracheostomy in a 14-year-old boy
Article information
Abstract
Tracheoinnominate artery fistula is a rare, fatal complication of tracheostomy, and prompt diagnosis and management are imperative. We report the case of tracheoinnominate artery fistula after tracheostomy in a 14-year-old boy with a history of severe periventricular leukomalacia, hydrocephalus, cerebral palsy, and epilepsy. The tracheoinnominate artery fistula was successfully treated with a stent graft insertion via the right common femoral artery. Endovascular repair of the tracheoinnominate artery fistula via stent grafting is a safe, effective, and minimally invasive treatment for patients in poor clinical conditions and is an alternative to traditional open surgical treatment.
Introduction
Tracheostomy has been used widely in prolonged respiratory support for pediatric patients with neuromuscular or respiratory dysfunction, or airway obstructions resulting from anatomical abnormalities and subglottic stenosis12). However, tracheostomy is associated with some complications especially in children3). Tracheoinnominate artery fistula (TIF) is an uncommon and potentially fatal complication of tracheostomy and is associated with high morbidity and mortality, therefore prompt diagnosis and treatment are essential4). TIF usually develops 7–14 days after tracheostomy and the overall incidence is 0.1%–1%56). Although TIF is primarily treated surgically with the ligation of the innominate artery and repair of the TIF, the survival rate after surgical treatment of TIF has been reported to be 25%–50%7).
Endovascular techniques have significantly advanced, providing physicians with an alternative treatment to a traditional open-surgical treatment in selected cases. We report a case of TIF in a 14-year-old boy that was successfully treated by the endovascular stent grafting of the innominate artery.
Case report
A 14-year-old boy visited the Emergency Department with respiratory failure and cyanosis. The patient was delivered via cesarean section at gestational age 33 weeks with birth weight of 1,660 g. He had a history of severe periventricular leukomalacia, cystic encephalomalacia, and hydrocephalus with a ventriculoperitoneal shunt. His height was 130 cm, and body weight was 18 kg. He had been bedridden since birth and had motor and intellectual disabilities. He was diagnosed with aspiration pneumonia and admitted to the intensive care unit. In the last 6 months, he had developed aspiration pneumonia three times. He needed prolonged ventilator care because of the frequent bouts of aspiration pneumonia and severe inspiratory stridor. Tracheostomy operation was performed on the 7th hospital day. On the 6th day after the tracheostomy, a small amount of fresh blood was found in the tracheostomy tube, and on the 8th day, the tracheostomy tube was removed accidentally by the patient's coughing. Copious intratracheal bleeding was noted from the trachea stoma. His vital signs became unstable. His blood pressure dropped below 70/30 mmHg, heart rate 60 beats/min, and oxygen saturation 40%–50%. He was in shock and cardiopulmonary resuscitation was performed for 5 minutes.
Endotracheal intubation was performed, and the hemorrhage was controlled temporarily by the hyperinflation of the cuff of the endotracheal tube. Chest radiographs showed no signs of pulmonary hemorrhage. Laboratory tests revealed markedly decreased hemoglobin levels but there was no feature suggestive of disseminated intravascular coagulation (white blood cell, 16,540/mm3; hemoglobin, 5.5 g/dL; hematocrit, 16.1%; platelet count, 158,000/µL; prothrombin time, 1.19 international normalized ratio; activated partial thromboplastin time, 40.4 seconds; fibrinogen, 254 mg/dL; d-dimer, 0.98 mg/L). He received transfusions of packed red blood cell and inotropics, such as dopamine and dobutamine. A few hours later, the patient's heart rate and blood pressure improved. However, massive bleeding from the trachea was noted on the next day. Portable flexible bronchoscopy could not identify the source of the hemorrhage at the trachea. Contrast-enhanced thoracic computed tomography (CT) demonstrated that the innominate artery was abutting on the adjacent tracheostomy tube (Fig. 1). Suspecting TIF, the patient was considered to be at high risk for open surgery. Emergency angiography was performed, and an 8-Fr sheath was inserted into the right femoral artery. Right innominate arteriogram showed that the endotracheal tube was close to the innominate artery, and the undulation of contrast medium around the innominate arterial wall revealed injuries to the arteries (Fig. 2). The diameter and length of the innominate artery were 7.3 mm and 48 mm, respectively, on contrast enhanced CT. The 6–12 mm/58 mm Jo-stent-graft (JOSTENT, Abbott Vascular Ltd., Rangendingen, Germany) was selected to match the measured innominate artery diameter. The Jo-stent-graft mounted on the 6/80 mm balloon catheter (FOXCROSS PTA catheter, Abbott Vascular Ltd., Baar, Switzerland) was placed through the innominate artery from the right common carotid artery. The balloon was inflated with the 8/40 mm balloon (FOXCROSS PTA catheter, Abbott Vascular Ltd., Baar, Switzerland) for attaching the innominate artery and Jo-stent-graft. Because the injured artery was adjacent to the bifurcation of the right carotid artery and the right subclavian artery, the stent graft was deployed through the innominate artery from the right common carotid artery (Fig. 3). The ruptured vessel wall was sealed and reconstructed by inserting a Jo-Stent-graft. Angiography performed after the stent placement demonstrated no extravasation of contrast medium or occlusion of the innominate artery. The right subclavian artery was covered and occluded by the stent graft, and it was refilled with significant retrograde flow from right vertebral artery, indicating subclavian steal (Fig. 4).

Contrast-enhanced axial slice computed tomography image of the upper chest region shows the tracheostomy tube (arrowhead) and the innominate artery (arrow). The tracheostomy tube was tightly attached to the innominate artery.

Right innominate arteriogram reveals the endotracheal tube abutting on the innominate artery (arrowhead). The undulation of contrast medium around the innominate arterial wall (arrow) indicates injury to the arteries.
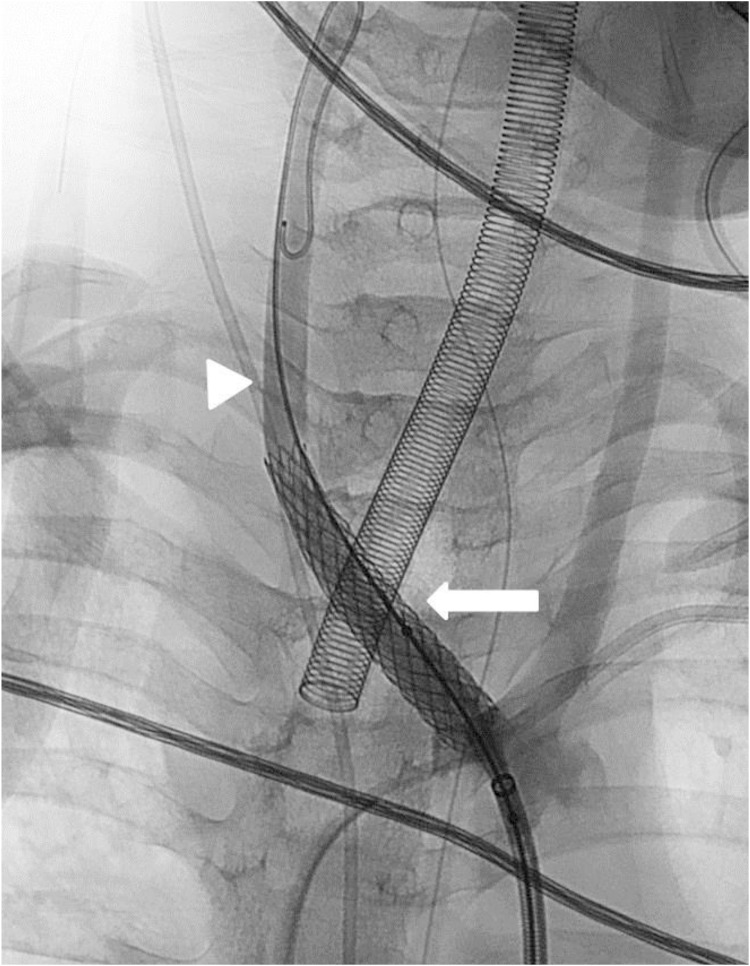
Post-stent-graft arteriogram reveals that the stent-graft (arrow) was placed in the innominate artery via the right common carotid artery (arrowhead).
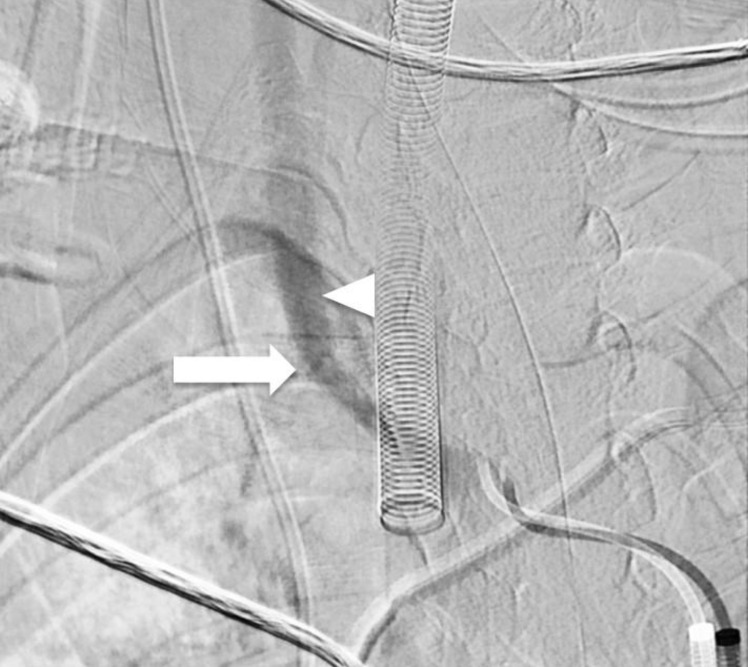
Vertebral angiogram demonstrating the right subclavian artery (arrowhead), occluded by the stent graft, refilled with significant retrograde flow (arrow) from the right vertebral artery, which is referred to as subclavian steal.
The patient recovered without any complications, such as sepsis, local infection, neurologic and right upper limb deficits of the subclavian steal syndrome. He was discharged from the hospital in 1 month after the endovascular repair. Twenty-four months after the endovascular repair, no ischemic complications had developed, and the patient had no clinical symptoms such as hemoptysis.
Discussion
TIF is a rare but usually life-threatening complication of tracheostomy, and can be fatal in the absence of prompt management such as a surgical operation. The reported incidence is 0.1%–1%, and it usually develops 7–14 days after tracheostomy. However, TIF can occur at any time after the procedure56). The innominate artery is close to the anterior tracheal wall8). The innominate artery commonly traverses the trachea at the level of the 9th tracheal ring, but the cross can occur anywhere between the 6th and 13th tracheal rings6). A tracheostomy is performed at the level between the 2nd and 4th tracheal rings in adults and at the 3rd and 4th tracheal rings in children9). A high-located innominate artery, especially in thin and young patients is a possible risk factor for fistula formation4).
The mechanism of injury is likely to be pressure necrosis of the anterior tracheal wall leading to erosion of the posterior aspect of the innominate artery caused by the tracheostomy cuff10). This is due to the mechanical force generated by the cuff or tip of the tracheostomy tube. The necrosis of the trachea can occur by a low-lying tracheostomy tube below the 3rd to 4rd trachea rings, overinflated cuffs, high-riding innominate artery, local infections by the tracheal defects, prolonged tracheostomy, or neck and chest deformities41112). In our case, the tracheostomy site was located below the 4th tracheal ring, and the innominate artery was located at midtrachea. Contrast-enhanced thoracic CT showed that the tracheostomy tube was adjacent to the innominate artery (Fig. 1).
Early diagnosis is the most important factor in the successful treatment of TIF. When unexpected bleeding occurs around a tracheostomy site between 3 days and 6 weeks following the tracheostomy, the clinician should consider that the bleeding could be associated with TIF. Sentinel bleeding is reported in more than 50% of patients who develop massive hemorrhage in TIF12). Thus, even a small amount of fresh bleeding should not be ignored. In our patient, a small amount of fresh blood was aspirated while suctioning through the tracheostomy site, but it was ignored. A few days later, acute massive bleeding occurred, and the patient developed potentially fatal hypovolemic shock.
Several techniques have been used for the temporary management of acute massive bleeding. The first maneuver is to overinflate a tracheostomy cuff or endotracheal tube cuff. If this maneuver fails to stop the bleeding, direct digital compression can be applied to the anterior tracheal wall through the stoma6). In pediatric patients, such digital compression may not be possible because of their small airways. A practical pediatric strategy is the inflation of a tracheostomy or endotracheal tube cuff13).
The main treatment of TIF is a surgical procedure with ligation of the innominate artery and bypass grafting of the distal innominate artery14). Morbidity and mortality rates are high after surgical operations for TIF. The mortality rate for emergency surgery has been reported to be more than 50%7). Recently, endovascular procedures involving stent graft implantation or endovascular embolization have significantly improved, and can be safely performed as an alternative to the traditional open surgical method in selected circumstances15). Cavalcante et al.10) described in 2015 the case of TIF successfully treated with a stent graft in a 4-year-old boy but first endovascular procedure (coil embolization) was not successful. Although endovascular stenting does not guarantee the complete elimination of TIF and it has some complications of graft infection, graft occlusion, and rebleeding due to tracheal erosion, it may be less invasive and more expeditious than surgical exploration7).
We decided to perform an endovascular treatment because open surgery was too dangerous due to several existing comorbidities. Endovascular stent grafting was done instead of transarterial embolization of the innominate artery because the entire occlusion of the innominate artery carries the high risk of cerebrovascular insufficiency. There were no complications such as stent graft infection, occlusion, or rebleeding for 2 years. Therefore, endovascular graft stenting of the innominate artery can be feasible, safe, and less invasive for the treatment of TIF in pediatric cases.
Acknowledgments
This study was supported by the Pusan National University Hospital (2016 research grant).
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.