Successful treatment of tubulointerstitial nephritis and uveitis with steroid and azathioprine in a 12-year-old boy
Article information
Abstract
Tubulointerstitial nephritis and uveitis (TINU) syndrome is a rare disease, often underdiagnosed or misdiagnosed in children. We describe the case of a 12-year-old boy who presented to Severance Hospital with a 1-month history of bilateral conjunctival injection. He was first evaluated by an Ophthalmologist in another hospital and diagnosed with panuveitis. Laboratory tests indicated renal failure, and a renal biopsy confirmed the diagnosis of acute tubulointerstitial nephritis. An extensive exclusion of all possible causes allowed a diagnosis of TINU syndrome. The patient was treated with a systemic corticosteroid (initially prednisolone, 2 mg/kg and later deflazacort 1 mg/kg) and topical steroid drops for 1 month. Azathioprine was later added to the treatment regimen and the systemic steroid was slowly tapered. The final outcome of renal-ocular disease was favorable in the patient. However, long-term follow-up is necessary to properly manage frequent relapses and incomplete renal recovery. TINU should be considered as a differential diagnosis in children with uveitis or acute renal failure.
Introduction
Tubulointerstitial nephritis and uveitis (TINU) syndrome is a rare disease that affects the renal tubular cells and uvea, causing tubulointerstitial nephritis and bilateral or unilateral uveitis. First described in 1975 by Dobrin et al.1), TINU usually occurs in adolescents and young women. Till date, approximately 200 cases have been reported worldwide; 5 cases have been reported in Korean literature, of which 2 were pediatric patients23456). We report the third case of TINU syndrome in pediatric patients and that was firstly treated with azathioprine in Korea.
Case report
A 12-year-old boy presented to Severance Hospital with a 1-month history of bilateral injected conjunctiva. He was initially evaluated by an Opthalmologist in another hospital and diagnosed with uveitis. Laboratory tests showed elevated blood urea nitrogen and creatinine levels; 36.0 and 3.07 mg/dL, respectively. He was therefore transferred to our hospital for further evaluation and management. He did not have generalized edema or costovertebral angle tenderness. His temperature was 36.9℃, and his blood pressure was 123/67 mmHg. He had anemia, hemoglobin was 9.7 g/dL (range, 14–18 g/dL). Serum sodium and potassium was 140/3.4 mmol/L and albumin was 4.2 g/dL (range, 3.8–5.4 g/dL). Estimated glomerular filtration rate was 30.9 mL/min/1.73 m2. Spot urinary protein to creatinine ratio was elevated to 1.27. Low-molecular-weight proteinuria, including urinary β2 microglobulin level was increased to 6.68 mg/L (range, 0.0–0.25 mg/L), suggesting low-molecular-weight proteinuria due to proximal tubule injury.
IgG and IgE were slightly elevated to 1,547 mg/dL (range, 639–1,349 mg/dL) and 232 mg/dL (range 0–230 mg/dL). On admission, CD3 and CD20 were 50.7% (range, 56%–84%) and 31.7% (range, 0%–20%), respectively. CD20 was decreased to 7.8% after 3 months. Immunologic tests, including antinuclear antibody, anti-ds DNA antibody, rheumatoid factor, and antineutrophil cytoplasmic antibody, were all negative. Human leukocyte antigen (HLA) B27 and HLA B51 genotyping were also negative.
Abdominal ultrasonography was unremarkable except for mild pelvic ascites. A dimercaptosuccinic acid renal scan demonstrated mildly decreased uptake in the upper pole of the left kidney with renal function of 62.59% and 37.41% in the right and left kidney, respectively. Renal biopsy findings showed interstitial inflammation and tubular atrophy (Fig. 1).
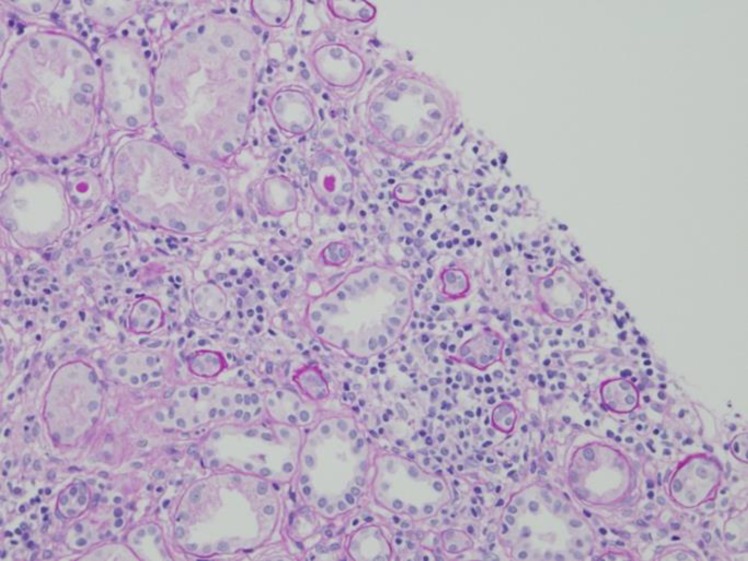
Renal biopsy specimen showing mononuclear cell infiltration of the interstitium and tubular atrophy and necrosis (H&E, ×100).
The patient was treated with a systemic oral glucocorticoid (prednisolone, 2 mg/kg daily). The acute renal failure and uveitis (Fig. 2) gradually improved. After 4 weeks of treatment, abdominal striae appeared as a side effect of prednisolone, and therefore, treatment was changed from prednisolone to deflazacort, which has fewer side effects. After 8 weeks of systemic steroid treatment, the deflazacort was slowly tapered. An immunosuppressant, azathioprine, was added at week 16 and maintained 1.7 mg/kg daily. We reduced the dose of azathiprine to 0.86 mg/kg daily at the 68th week of treatment, and the creatinine level had decreased to 0.93 mg/dL at last follow-up (Fig. 3). Spot urinary protein to creatinine ratio was also maintained for values less than 1.0. The patient's uveitis was treated with topical steroid and antibiotic drops. The final outcomes of both the renal and ocular manifestations of the disease were favorable.

Fundoscopy of the right eye (A) and the left eye (B). Both fundoscopy images showing inflammation of retina (arrows).
Discussion
Although the pathogenesis of TINU syndrome remains elusive, TINU syndrome is thought to be an immune disorder and associated with HLA genotype7). This is supported by the high levels of immune activation markers such as soluble tumor-necrosis factor receptors, soluble interleukin-2 receptors, and neopterine found in patients with TINU7). Additionally, the ratio of CD4+ to CD8+ peripheral blood lymphocytes is reduced, and, on renal biopsy, the majority of cells infiltrating the interstitium are T-lymphocytes on renal biopsy7). Infectious agents such as Epstein-Barr virus and Chlamydia trachomatis, have been linked to some cases of TINU89); drugs such as nonsteroidal anti-inflammatory agents and antibiotics are regarded as important triggers in other cases10). However, our patient did not have any of these triggers.
Some studies suggest that modified C-reactive protein (mCRP) may be involved in the pathogenesis of TINU. The mCRP results from dissociation of CRP under conditions such as altered pH, high urea concentration, or low calcium concentration11). Tan et al.11) reported that anti-mCRP autoantibodies were detected in all TINU patients, renal biopsies revealed upregulated expression of mCRP, and IgG was colocalized with mCRP in human renal and uveal tissues.
Patients with TINU syndrome usually present with vague symptoms such as anorexia, fever, weight loss, fatigue, and polyuria, with or without uveitis12). Multisystem involvement, including hyperthyroidism and diabetes mellitus, may occur13); however, in most patients diagnosed with acute tubulointerstitial nephritis (ATN), endocrine and ophthalmic examination is not performed. Many cases show that TINU did not have typical symptoms, and the timing of uveitis was variable. Therefore, all patients with ATN should undergo a slit-lamp examination for uveitis.
Patients with TINU syndrome have been treated successfully with corticosteroids14), but the use of systemic steroids may be restricted in patients with significant tubulointerstitial injury. However, uveitis must be treated because of its poor prognosis. Some patients require additional immunosuppressive drugs such as azathioprine, methotrexate, or cyclosporine if steroid resistance, recurrence of uveitis, or significant steroidal side-effects occur15). In our case, the patient developed Cushingoid feature, abdominal striae. To our knowledge, this is the first case that was treated with azathiprione in pediatric patients with TINU in Korea.
To date, 2 cases of pediatric TINU syndrome have been reported in the Korean literature. The first case was a 14-year old girl and her nephritis resolved spontaneously, but her uveitis, which was treated with topical steroids, had a remitting and relapsing course2). The second case was a 9-year-old boy with severe immunologic dysregulation, especially T cell5). He was treated with systemic steroid, oral prednisolone (2 mg/kg), but his uveitis was not responsive to high dose systemic prednisolone but responded to cyclosporine A5). In second case, Lee et al.5) suggested that T cells had most important role in pathogenesis of TINU syndrome. However, our patient showed CD20 elevation and normal CD3 level which means B cells activation. And he responded to azathioprine, which inhibit T cells and B cells proliferation. To our knowledge, ours is the first patient in Korea treated with azathioprine for pediatric TINU syndrome and he was successfully treated. The outcome of renal involvement of TINU is excellent in most cases; however, up to 48.6% patients experience symptomatic ocular complications14).
TINU syndrome is very rare, but it is important to consider it in young patients with vague symptoms. Early recognition is vital for a better prognosis. Therefore, this diagnosis should be considered when evaluating patients with tubulointerstitial nephritis or uveitis. Further studies are necessary to determine accurate pathophysiology and universal recommendation of treatment for TINU syndrome.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
