High antistreptolysin O titer is associated with coronary artery lesions in patients with Kawasaki disease
Article information
Abstract
Purpose
In Kawasaki disease (KD) patients, coronary artery complications, incomplete and refractory types occur more frequently in patients with streptococcal or other bacterial/viral infections. Recently, we observed a higher incidence of coronary lesions in KD patients with high anti-streptolysin O (ASO) titer. Therefore, we hypothesized that KD patients diagnosed with concurrent streptococcal infection have poor prognoses, with respect to treatment response and development of coronary artery lesions.
Methods
A retrospective review was performed in 723 patients with KD who were admitted to 2 major hospitals between June 2010 and September 2017.
Results
Among 723 patients with KD, 11 initially showed an elevated ASO titer (>320 IU/mL) or elevated follow-up ASO titer after treatment. Of these patients, 5 showed no response to the first intravenous immunoglobulin treatment, 3 had abnormalities of the coronary arteries. This is a significantly higher proportion of patients with a high ASO titer (n=3, 27.3%) than those with a normal ASO titer (n=53 [7.4%], P=0.047). A severe clinical course was seen in 81.8% of patients in the high ASO group versus 14.5% of patients in the normal ASO group.
Conclusion
It is not certain whether acute streptococcal infection may cause KD, but this study revealed that KD with high ASO titers showed higher rates of severe clinical course. It may be helpful to analyze concurrent streptococcal infection in patients with a severe clinical course.
Introduction
Kawasaki disease (KD) is an acute systemic inflammatory disease involving multiple organs and tissues [1]. Children <5 years old of age are most susceptible to KD [2]. The diagnosis of KD depends on the clinical manifestations according to the defined criteria of the presence of fever for at least 5 days, with at least 4 of the 5 following clinical features: (1) erythema and changes in the lips and oral mucosa, (2) bilateral nonexudative bulbar conjunctival injection, (3) polymorphous maculopapular rash (not petechial, bullous, or vesicular lesions), (4) changes in the extremities, including erythema and edema of the hands and feet in the acute phase and/or desquamation starting around the nail bed, and (5) cervical lymphadenopathy, usually unilateral (diameter>1.5 cm) [2-4]. Incomplete KD is defined as prolonged unexplained fever without meeting at least three of the above five criteria [2].
Despite many investigations and many candidates, no unique infectious agents have been identified as the sole etiologic agent responsible for KD. The role of viral infections in the pathogenesis of KD has been controversial [5-7]. The association with super antigens such as staphylococci or streptococci has been constantly argued [8-10]. In KD, incomplete type of KD and coronary artery complications occur more frequently in patients with streptococcal or other bacterial/viral infections [11-13]. Some reports have stated that systemic inflammation is linked to acute coronary events, including endothelial dysfunction [14,15]. We hypothesized that KD patients diagnosed with streptococcal infection have poor prognosis, especially in terms of treatment response and the development of coronary artery lesions.
Here, we investigated the coronary artery lesions and response to intravenous immunoglobulin (IVIG) in relation to the level of anti-streptolysin O (ASO) in patients with KD.
Materials and methods
1. Study participants
We retrospectively reviewed KD patients admitted to Kyung Hee University Medical Center and Kyung Hee University Hospital at Gangdong between June 2010 and September 2017. The clinical data of a total 723 KD patients were reviewed. Only patients for whom ASO titer and echocardiography data were available were included in the study. The Institutional Review Board of Kyung Hee University Hospital at Gangdong approved this study (approval number: 2018-08-047) and waived the need for written informed consent.
2. Laboratory data and echocardiography
Laboratory data including microbiology results, imaging studies, and echocardiography examinations were collected and reviewed. A standardized set of laboratory tests was performed before and 36 hours after the end of IVIG infusion, including complete blood count, white blood cell differential count, erythrocyte sedimentation rate, C-reactive protein, albumin, alanine aminotransferase, aspartate aminotransferase, bilirubin, creatinine, ASO, and urine analysis. All except one patient diagnosed with KD received IVIG (2 g/kg) for 12 hours and these blood tests were performed 36 hours after the end of treatment. Only 1 patient did not receive IVIG, because he was referred to our hospital without a fever. Blood culture, throat swab, respiratory viral polymerase chain reaction (PCR), and serum Mycoplasma antibody tests were performed in patients who were suspected of having an infection. Respiratory viral PCR can detect 12 respiratory viruses and subtypes included the following: adenovirus, respiratory syncytial viruses A and B, influenza viruses A and B, parainfluenza 1,2, and 3, rhinovirus, metapneumovirus, and coronaviruses 229E, NL63, OC43, and HKU1. Serial echocardiography exams were performed during hospitalization by an expert pediatric cardiologist. By correcting for BSA, a z score system provided by Kobayashi et al. [16] was used in our study. In this study, z score ≥2.5 was regarded as a coronary artery abnormality.
3. Diagnostic criteria
The diagnosis of KD depends on the clinical manifestations according to the defined criteria of the presence of fever for at least 5 days, with at least 4 of the 5 principal clinical features [2]. Incomplete KD is defined as prolonged unexplained fever without meeting up to three of the 5 criteria [2].
We enrolled patients if their ASO titer had increased 4 fold in 2 measurements [17]. This is generally accepted as significant in clinical practice. However, if the ASO titer could be measured only once, we enrolled >320 IU/mL, which is the upper normal limit presented in a recent study and many other studies [18-20]. If the peak ASO titer was <320 IU/mL in a patient who was measured twice, the patient was excluded from the study group. Patients who were discharged or transferred without appropriate treatment were also excluded.
A good clinical course group is defined as fever subsiding within 36 hours after the end of first IVIG treatment without any coronary artery abnormalities. On the other hand, relatively severe KD groups were defined as follows; (1) no response to the first IVIG treatment, and a second IVIG treatment or methylprednisolone (MPD) pulse therapy were required, or (2) KD patients with coronary artery abnormalities.
4. Statistical analysis
Fisher exact test was used to compare data using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). and values of P< 0.05 were considered statistically significant.
Results
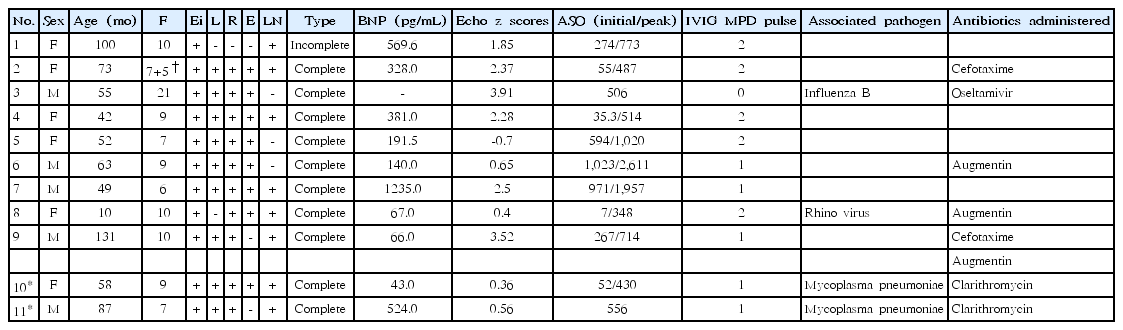
A total of 723 patients were diagnosed with KD between June 2010 and September 2017. Patients were admitted to the hospital on average 5.9 days after the onset of fever. These patients’ clinical data are summarized in Table 1. Of them, 9 (81.8%) had a severe clinical course. Only 2 patients (18.2%) had a relatively good clinical course.
Of the 11 KD patients with elevated ASO levels, 5 were boys and 4 were girls (ratio, 0.83:1), with a mean age of 65.5 months (range, 10–131 months) at the time of the KD diagnosis. Ten patients had complete KD, while 1 had incomplete KD. One of the patients (female, 73 months) experienced a KD relapse 15 days after the first treatment.
At the time of diagnosis, all 11 patients had a fever, (mean duration, 9.2 days; range, 5–21 days) and a nonexudative eye injection. 10 patients (90.9%) had a polymorphous rash, 9 patients (81.8%) displayed noticeable changes in the lips or oral mucosa, 8 patients (72.7%) had erythema and edema of the extremities, and 7 patients (63.6%) had cervical lymphadenopathy. The mean fever duration was 9.4 days in the severe KD group and 8 days in the good clinical course group. All patients in the good clinical course group had complete KD, fevers that subsided within 36 hours after the first IVIG treatment, and normal coronary arteries. At the time of diagnosis, 4 patients (36.4%) had a confirmed concurrent infection, the most common pathogens being Mycoplasma pneumoniae (n=2), rhinovirus (n=1), and influenza B (n=1), confirmed by respiratory viral PCR. Only 1 patient was confirmed to have Streptococcus pyogenes, by a throat culture at diagnosis. Blood cultures were all negative in these 11 patients.
Four patients with a high ASO titer did not receive any antibiotics despite a sustained fever, whereas the other 7 did receive antibiotics. However, the prevalence of coronary artery lesions did not differ between them.
As for seasonal patterns, 4 cases were diagnosed in early summer (2 in May, 1 in June, and 1 in July), while 3 were diagnosed in winter (1 in January, 2 in February). No cases were diagnosed in the fall.
Table 2 shows the numbers and percentages of patients by group. Those with a severe clinical course developed coronary lesions, received a second round of IVIG, or required MPD pulse therapy. A severe clinical course was seen in 81.8% of patients in the high ASO group versus 14.5% of patients in the normal ASO group.
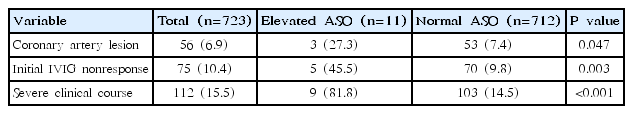
Comparisons of clinical outcomes of patients with Kawasaki disease having a high versus normal ASO titer
Cardiac involvement was screened for in all patients using echocardiography. A significantly higher proportion of patients with a high ASO titer (n=3, 27.3%) than those with a normal ASO titer (n= 53; 7.4%) showed abnormalities of the coronary arteries (P=0.047). A second round of IVIG was administered in more patients with an elevated ASO titer (45.5%) than patients in the normal ASO group (9.8%).
Discussion
Here we reported the severity of KD with streptococcal infections among 723 KD patients. Among them, 11 had elevated ASO levels before or after IVIG treatment. Of those, 9 had high ASO titers or 4-fold increased titers, and clinical findings for them were worse than those for the other KD patient. Five patients showed no response to the first IVIG treatment (45.5%, P=0.003), 3 had abnormalities of the coronary arteries (27.3%, P=0.047). A severe clinical course was seen in 81.8% of patients in the high ASO group versus 14.5% of patients in the normal ASO group (P<0.001).
Jordan-Villegas et al. [11] reported that patients with KD who also had respiratory viruses have a higher frequency of coronary artery dilatation and were more often diagnosed with incomplete KD. Other researchers have linked streptococcal infection and the KD [21,22]. In particular, the reason might be clinical overlap between streptococcal infection and the KD, such as persistent fever, a desquamative rash, and erythema of the mucous membranes in streptococcal toxic shock syndrome. A superantigen-mediated process might be related to this process [8]. Matsubara and Fukaya [8] suggest that KD is a response to superantigens in genetically susceptible individuals. These all support our results that KD with streptococcal infection had a severe clinical course.
In temperate climates, the incidence of group A streptococcal infection peaks during the winter and early spring. In Japan, several group A streptococcal serotypes showed a bimodal distribution, with peaks in December to February and again in May to June and a prominent nadir of infections in September [23]. In Korea, a seasonal pattern was observed in which KD occurred more often in early summer (May, June, and July) and winter (January and February), and occurred less often in the spring and fall [24]. Of the 11 KD diagnoses, 4 were made in early summer (2 in May, 1 in June, and 1 in July), and 3 were made in winter (1 in January, 2 in February). No patients were diagnosed in the fall. This may imply that infectious agents might be the trigger of KD and that Streptococcus is one of the possible agents is the possible agents.
Measurement of ASO is relatively inexpensive and easy to perform because the proceeds, along with other blood tests. However, there are significant difficulties assigning a “normal” ASO titer value. The only upper normal limit is >320 IU/mL, presented in a recent study and many other studies [20]. Also, ASO titer does not always indicate a recent streptococcal infection. Therefore, an increase in an ASO titer is indicative of a preceding group A Streptococcus infection, so sequential measurements are recommended [17-19]. We attempted to obtain 2 sequential measurements, but only a single sampling was performed in some patients. IVIG contains the pooled immunoglobulins from the plasma of approximately a thousand or more blood donors. As a cocktail of different antibodies against various virulence factors including Streptococcus, it can be provided to the patients. In this study, among 11 patients, 5 patients’ ASO titer was high (range, 506–1,023) at the time of diagnosis, and 6 patients’ ASO titer elevated after IVIG treatment.
In our study, 4 of the 11 patients with a high ASO titer did not receive any antibiotics despite a sustained fever, whereas the other 7 did receive antibiotics. However, the prevalence of coronary artery lesions did not differ between them. In 2018, Han and Lee [25] report the anbibiotics used in 140 KD patients. The KD patients with antibiotics experienced more hospital days (P=0.045). On the other hand, there was no difference in unresponsiveness to IVIG and development of coronary abnormalities between the 2 groups.
Despite its many limitations, our study’s main strength is that we treated all patients using a relatively constant protocol. A series of blood tests was performed at the time of diagnosis, including the ASO titer, because the tests are simple and do not require additional specimens. IVIG 2 g/kg was administered slowly over 12 hours as soon as KD was diagnosed and discontinued whenever a patient’s temperature exceeded 38°C. Thirty-six hours after the end of the IVIG administration, the blood tests, including the ASO titer, were repeated to exclude acute streptococcal infection and the fever pattern was closely observed. In addition, echocardiography was performed by an expert pediatric cardiologist at the admission, 2–3 weeks later, 2 months later, or 1 year later depending on each patient’s status to monitor for coronary artery or other transient lesions.
In this study, we do not know whether acute streptococcal infection or past infection caused the KD. However, in KD with acute streptococcal infection, the fever duration was longer than average and the frequency of coronary artery aneurysms was higher. In cases of incomplete KD or prolonged fever, it may be necessary to diagnose acute streptococcal infection using ASO titer or culture; therefore, more aggressive therapy is needed to prevent coronary artery lesions. Prospective studies with larger samples are needed to further examine the relationship between KD with coronary lesions and elevated ASO titers.
Notes
No potential conflict of interest relevant to this article was reported.