Reality of Kawasaki disease epidemiology
Article information
Abstract
Epidemiologic studies of Kawasaki disease (KD) have shown a new pattern or change of its occurrence suggestive of its pathophysiology or risk factors from the first patient with KD reported in 1961. The incidence of KD in Northeast Asian countries including Japan, South Korea, China, and Taiwan is 10–30 times higher than that in the United States and Europe. Knowing the true epidemiology of KD in each country and the availability of publications of KD epidemiology also could benefit general health care providers and general population. This would enable the early detection and treatment of KD, ultimately reducing the incidence of coronary artery complications and mortality. Therefore, efforts to investigate the true epidemiology of KD should be continued in every country using a questionnaire survey, National Health Insurance system data, or combined methods depending on each country’s medical environment to ensure high-quality care of patients with KD.
Graphical Abstract
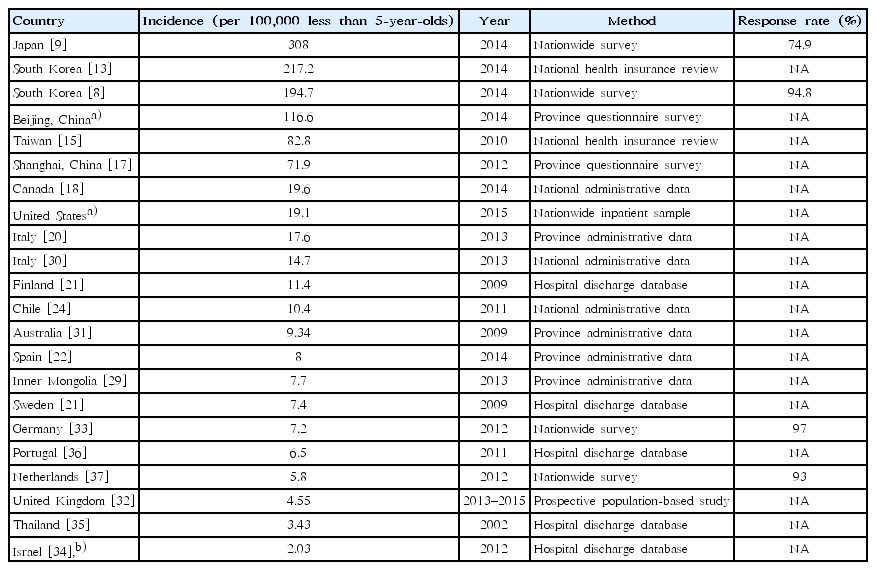
The incidence of Kawasaki disease (KD) worldwide. The incidence of KD per 100,000 less than 5-year-olds has various geographic occurrence patterns. It is much higher in Northeast Asian countries including Japan, South Korea, China, and Taiwan, 10–30 times higher than that of KD in North America and Europe.
Introduction
Kawasaki disease (KD) is an acute febrile systemic vasculitis that predominantly occurs in children younger than 5 years of age and the most common acquired heart disease during childhood in most industrialized countries [1]. Coronary artery abnormalities, the well-known complication of KD, occur in up to 15%–25% of patients if KD is not treated on time [2,3]. However, the etiology of KD remains unclear, and many researchers worldwide seek to identify the exact pathophysiology of, genetic profiles of, and new treatment strategies for KD.
What is the benefit of elucidating the epidemiology of KD? Knowing the true epidemiology of any disease is basic to understanding it. It also enables the identification of new patterns or changes in disease occurrence and infers its pathophysiology or risk factors. Unfortunately, a large number of children with KD are still being misdiagnosed with other infectious diseases in many developing countries, including South Korea [4]. Knowing the true epidemiology of KD in each country could be beneficial to general health care providers including pediatricians and also elucidate the KD burden in acute treatment settings and the prevalence of long-term adult coronary artery disease [4,5]. Therefore, efforts to investigate the true epidemiology of KD should be continued in every country to ensure high-quality care of affected patients.
History of KD epidemiology
From the first patient with KD reported in 1961 and the 50 patients published in 1967 by Dr. Tomisaku Kawasaki over the following 5 years, KD has been known to Japanese doctors [6]. From these case series, a nationwide epidemiologic survey has been performed every 2 years in Japan since 1970; to date, more than 300,000 patients have been reported [7]. KD cases were recognized on every continent by the 1980s. To date, KD has been reported from more than 60 countries across all continents and has been recognized and published increasingly in developing countries [4,7]. In South Korea, nationwide surveys for KD started in 1994 using KD patient data from all resident-training hospitals in 1991–1993 and have been conducted every 3 years since [8]. Taiwan started a national surveillance program for KD in 1995 using data collected from the National Health Insurance database, which is separate from those of Japan and South Korea.
Method of assessing KD epidemiology
Methods used to determine KD epidemiology differ among countries according to each country’s medical environment; therefore, epidemiological comparisons among countries should consider differences in epidemiological methods and the completeness of diagnostic ascertainment and patient reporting [2]. The most frequently used method involves using active nationwide surveys as in Japan and South Korea [8,9]. The definite merit of this modality is that we can obtain various and detailed data of KD occurrence including laboratory data, coronary artery complications, and detailed other complications from the tailored questionnaire. From the detailed data, we can infer the pathophysiology and risk factors of KD occurrence and complications. The most important factors in obtaining an accurate incidence are recruiting hospitals to treat as many KD patients as possible and improve the nationwide survey response rate. The survey’s success depends on each hospital’s active participation and principal investigator’s effort to obtain the data. The response rate in Japan was 71.6% from the 2011–2012 nationwide survey and 74.9% from the 2013–2014 nationwide survey [9,10]. In South Korea, the response rate was 87% from the 2009–2011 nationwide survey and 94.8% from the 2012–2014 nationwide survey [8,11]. These factors that affect the incidence of KD are inborn drawbacks of a nationwide survey. The other problem is that the diagnostic accuracies of KD among hospitals could be quite diverse. Some hospitals tend to overdiagnose KD, whereas others underdiagnose it. Therefore, a nationwide survey cannot reflect the true incidence of KD despite its traditional value and merit to provide clues about its pathophysiology and risk factors.
The other method of obtaining KD incidence data involves using national health insurance system data as in Taiwan and South Korea [12-15]. Its main strength is that it includes the entire population of each country. Because the national health insurance programs of Taiwan and South Korea cover more than 99% of the population due to mandatory subscription, their use can represent the incidence of KD since they include all patients treated at all hospitals. In South Korea, researchers used the data of patients who received intravenous immunoglobulin under the diagnosis of KD (ICD-10 [International Statistical Classification of Diseases and Related Health Problems, 10th ed], M30.3) [13]. This method provides much more incidence data of KD compared with nationwide survey method because of the former’s imperfect response rate; however, it is also not free of the possibility of the over- or underdiagnosis of KD in the real world. The demerit of this system is that the collected data are mostly simple and usually confined to incidence, age distribution, sex ratio, province distribution, and seasonal variations. Among national health insurance data, some patients with KD who did not receive intravenous immunoglobulin could be missed. For example, 4.6% of patients with KD were not treated with intravenous immunoglobulin from the nationwide survey data in 2012–2014 in South Korea, which means that 4.6% of patients with KD were not included in the national health insurance data [8].
Other modalities can reveal the incidence of KD depending on each country’s medical system. For example, researchers in the United States have used passive national surveillance data reported to the Centers for Disease Control and Prevention, kids’ inpatient database, or nationwide inpatient samples since the mid-1970s [12,16]. In China, considering the huge population, a nationwide survey is quite difficult; therefore, they use questionnaire surveys of the KD incidence in each local province questionnaire survey, especially Beijing and Shanghai [17].
Global incidence of KD
Diverse epidemiological patterns of KD of each country are described in Table 1. The incidence of KD differs among countries. The incidence of KD in Northeast Asian countries including Japan, South Korea, China, and Taiwan are 10–30 times higher than that in the United Stated or Europe [8,9,16]. The other unique finding is that the incidence of KD is increasing continuously in Northeast Asian countries [8,9]; however, it is stationary in North America [18] and Europe [16].
The incidence of KD in Japan is increasing continuously; the last known figure was 308 per 100,000 in less than 5-year-olds in 2014 [9], while that in South Korea is also increasing continuously (194.7 per 100,000 in less than 5-year-olds in 2014) [8]. In China, an epidemiologic study was performed in Beijing and Shanghai using a questionnaire survey, and the incidence of KD was reported as 111.6 and 71.9 per 100,000 less than 5-year-old children, respectively [17]. Researchers in Taiwan used a national health insurance review in an KD epidemiology study and reported an incidence of KD of 82.8 per 100,000 less than 5-year-old children in 2010 [15].
Outside Northeast Asian countries, the incidence of KD is significantly lower. In North America, KD epidemiological studies have been performed using administrative data, and the incidence of KD in the United States was 19.1 per 100,000 less than 5-year-old children in 2015, while those in Canada were 19.6 per 100,000 less than 5-year-old children in 2014 [18]. Compared with the incidence of KD in Northeast Asia, the incidence of KD was stationary without significant increases or decreases over several decades [4,16]. An interesting finding of KD epidemiology in the Unites States is that children of Asia-Pacific Islander descent had the highest incidence of KD among various ethnicities. Especially in Hawaii, the incidence of KD in Japanese Americans was similar to that in Japan (greater than 200 per 100,000 less than 5-year-old children), which suggests an in-depth genetic susceptibility of KD occurrence [4,19].
Epidemiologic studies are rare in most European countries, and the incidence of KD has been reported as less than 17.6 per 100,000 less than 5-year-olds [20], remaining stationary without significant increases or decreases as in North America [4,21,22]. In Latin America, no systematic epidemiological study of KD has been performed in each country, although the incidence of KD has been reported sporadically in several countries [23,24]. The recently founded Latin American Kawasaki Disease Network (REKAMLATINA) is expected to improve the understanding of KD epidemiology in Latin America. Twenty Latin American countries joined in this project and have been using this multinational database since 2013 [25].
What KD epidemiology suggests clinical meaning?
National KD epidemiologic studies have shown diverse disease patterns and changes of KD symptoms, signs, and laboratory findings for several decades. These historical changes modified the diagnostic criteria of KD over time. For example, the 2017 American Heart Association guideline suggested that in the presence of greater than 4 principal clinical symptoms, particularly when the patient shows redness and swelling of the hands and feet, the diagnosis of KD may be made with only 4 days of fever [2]. They also suggested that experienced clinicians who have treated many KD patients may make the diagnosis of KD in rare instances with only 3 days of fever in the presence of classic clinical symptoms and signs [2].
KD epidemiological studies examined the pathophysiology of or risk factors for KD. Seasonal variations in different countries have been the major findings of KD epidemiological studies. Regions in the extratropical northern hemisphere including Japan, South Korea, and the United States have experienced a peak in KD in the winter and a second peak in the summer in Japan and South Korea and in the spring in the United States [2,8,9,19]. However, seasonal variation in the tropics and the extratropical southern hemisphere is not evident [2]. Several epidemiological studies demonstrated that KD is associated with preceding respiratory illness [2,26,27].
The other important fact of KD epidemiology is that it occurs predominantly in Northeast Asians and Japanese Americans also showed a high incidence in the United States as in Japan [4,19] These 2 unique findings in the KD epidemiological studies of seasonal variation and geographical patterns of occurrence have been suggested since many infectious agents activate innate and adaptive immune system and provoke KD in genetically susceptible patients [2,7,28].
Knowing the true epidemiology of KD in each country and the availability of related publications could also benefit general health care providers including pediatricians and parents of KD patients. KD vigilance in general health care providers and the general population definitely could encourage the early detection and treatment of KD, subsequently reducing coronary artery complication and mortality rates [4,5]. For example, the incidence of giant aneurysm decreased from 0.26% in the 2009–2011 nationwide survey to 0.16% in the 2012–2014 nationwide survey in South Korea, accompanied by the increased KD incidence [8,11].
What could be the best epidemiological study of KD?
As mentioned above, the success of epidemiological studies depends on the completeness of KD diagnostic evaluation and patient reporting. In the nationwide survey of KD, the most important point is achieving a 100% response rate from all hospitals treating acute KD. However, achieving a 100% response rate is impossible in the real world because a nationwide survey requires very active participation from each hospital. For an epidemiological study using national health insurance system data, the most critical point is recruiting all KD patients treated with or without intravenous immunoglobulin and gathering as much epidemiologically detailed data as possible.
Regarding basic epidemiological data including KD incidence, age, sex distribution, and seasonality, an epidemiological study using National Health Insurance system would be the best modality if we could access the data of all KD patients. Detailed epidemiologic data including each patient’s symptoms, signs, laboratory findings, echocardiographic findings, and other combined morbidities; thus, the nationwide questionnaire survey has strong benefits of revealing disease changes and the possible pathogenesis of KD. Therefore, these 2 epidemiologic modalities should be combined to reveal the true epidemiology of KD.
Conclusions
Epidemiological studies of KD have shown new patterns of or changes to KD occurrence and supported to infer pathophysiology or risk factors of KD. Therefore, the effort to investigate true epidemiology of KD should be continued in every country to ensure high-quality care of patients with KD using questionnaire surveys, national health insurance system data, or combined methods depending on each country’s medical environment.
Notes
No potential conflict of interest relevant to this article was reported.