Thyroid disturbances in children treated with combined pegylated interferon-alpha and ribavirin for chronic hepatitis C
Article information
Abstract
Background
Immunomodulatory properties of interferon (IFN) have been documented. It may induce autoimmune diseases such as autoimmune thyroiditis with hypo- or hyperthyroidism. In addition, it may impair thyroid hormone synthesis through affecting iodide organification in thyroid gland.
Purpose
The aim of this study was to describe thyroid function tests disturbances in children with chronic hepatitis C (CHC) receiving pegylated interferon-alpha (PEG IFN-α) plus ribavirin.
Methods
Fifty children with CHC virus infection who received combined pegylated interferon-alpha with ribavirin were selected. Other 50 apparently healthy children of matched age and sex (considered as control group) were selected. All children (100) were subject to liver function tests, virological studies, and follow-up of thyroid function test during and after the treatment course.
Results
Our study showed that 28% of children received combined PEG IFN-α plus ribavirin showed subclinical hypothyroidism. After 24 weeks treatment with combined therapy of IFN plus ribavirin, the mean level of thyroid stimulating hormone (TSH) was 3.23±88 mU/mL, while TSH was 1.16± 0.77 mU/mL before starting treatment. On the other hand, mean TSH was 1.09±0.92 mU/mL in normal control group.
Conclusion
This study revealed an association between subclinical thyroid dysfunction and treatment with IFN-alpha and ribavirin in children. Further studies on larger number of patients and longer follow-up duration are recommended for further confirmation.
Introduction
Hepatitis C virus (HCV) infection is a world health problem, affecting over 160 million people worldwide. Liver cirrhosis (LC) and hepatocellular carcinoma (HCC) are well-known complications related to chronic hepatitis C (CHC) infection [1]. Accurate incidence of chronic HCV infection in Egyptian children is not properly known [2].
Transmission of HCV differs in different areas of the world. Intranatal transmission is common in well-developed countries while horizontal transmission is common while in developing countries [3]. Some factors can increase the morbidity of HCV infection in as obesity, malignant tumors, chronic hemolytic anemia needed recurrent blood transfusions, and coinfected with human immunodeficiency virus or hepatitis B virus (HBV) [4]. Complications like hepatocellular damage and LC are rare in children in comparison to adults [5].
Until recently, pegylated interferon with ribavirin is the only recommended treatment of CHC, first approved in December 2008 [6]. Early treatment in children prevents the long-term complications of chronic HCV infection [5]. Such treatment may induce autoimmune diseases as autoimmune thyroiditis, with hypo- or hyperthyroidism and interfere with the organification of iodide leading to impairment of thyroid hormone synthesis [7].
The aim of this study was to describe disturbances of thyroid function tests in children with CHC receiving pegylated interferon-alpha (PEG IFN-α) plus ribavirin.
Methods
Fifty children with chronic HCV infection, followed-up from June 2010 till April 2016 were included in the primary selection. Fifty healthy children of the same age and sex considered as a control group submitted for follow-up and thyroid function tests. The study was revised and approved by the local ethical committee and Institutional Review Board (IRB) of National Liver Institute (IRB00003413). Legal guards of participants provided informed consent to participate in the study. Patients with the following conditions were excluded: (1) coinfection with HBV, (2) peripheral blood neutrophils count <1.5×103/mL, platelet count <70×103/mL or hemoglobin level lower than 10 g/dL, (3) concomitant serious medical illnesses, such as; malignancy, autoimmune diseases, severe cardiopulmonary disease, uncontrolled diabetes mel-litus, or thyroid diseases.
All patients and healthy control children had:
(1) Liver function tests (aspartate aminotransferase, alanine aminotransferase [ALT], alkaline phosphatase, gamma glutamyl-transferase, total bilirubin direct bilirubin, total proteins, and albumin). Tests were carried out using Integra 400 auto analyzer (Roche diagnostics Corp., Hague Road, IN, USA).
(2) Viral markers, using enzyme-linked immunosorbent assay (ELISA) technique. HCV antibodies for both groups were done by kit from Inngenetics (Ghent, Belgium; Pawlotsky, 2002). HBV surface antigen and HBV core antibodies (HBcIgM and HBcIgG) were done by ELISA technique, by kit from Sorin Biomedica Co. (Spain).
(3) Detection of HCV-RNA in the sera (for positive HCV antibodies only). It was done using COBAS Ampliprep/COBAS TaqMan, Roche Molecular Systems, Inc. (Branchburg, NJ, USA). It is a nucleic acid amplification test for the quantification of HCV-RNA.
The diagnosis of CHC was made by a persistent or intermittent elevation of ALT, the upper limit of laboratory normal was 40 IU/L over a 6-month period, anti-HCV positivity and detection of HCV-RNA in the sera (for positive HCV antibodies only).
(4) Liver biopsy was done for the diseased group only, after sedation with midazolam (0.3 mg/kg/dose), by true cut needle before IFN therapy. Biopsy specimens were fixed in formalin-buffered saline, embedded in paraffin followed by a histological examination using hematoxylin and eosin stains, orcien stain and Periodic acid Schiff stain for routine histopathological evaluation. Hepatic necro-inflammatory activity and liver fibrosis were evaluated according to Ishak staging and grading scores.
(5) Thyroid stimulating hormone (TSH) was measured by (immotile 1000, Siemens, Pittsburgh, PA, USA), while free thyroxin (FT4) and free triiodothyronine (FT3) were done before starting treatment and at the end of treatment for the diseased group were measured by radioimmunoassay using an automated system (Roche Diagnostics). Reference range for TSH was 0.4–4.0 mU/L, for FT3 was 3.5–5.5 pmol/L, and for FT4 was 10.0–26.0 pmol/L.
(6) Antithyroglobulin antibodies and antithyroid peroxidase in case of clinical thyroiditis.
Patients with chronic HCV infection (50), received antiviral therapy consisting of PEG IFN-α 2b in a dose of 60 μg/1.73 m2/wk subcutaneously (PEG-interferon, Schering-Plough Brinny, Kenilworth, NJ, USA) plus ribavirin 15 mg/kg/day orally.
According to sustained virological response (SVR) (undetectable HCV-RNA at 24 weeks after treatment completion), patients were classified into 2 groups, responders and nonresponders.
Data were analyzed using the IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Qualitative data were expressed as frequency and percentage.
The study was revised and approved by the local ethical committee and Institutional Review Board (IRB) of National Liver Institute (IRB No. 00003413).
Results
Hundred children divided into 2 groups, chronic HCV group and normal control group, each group was 50 children.
(1) The first group includes children with chronic HCV, 32 males (64%) and 18 females (36%) were further subdivided in 2 subgroups:
(a) Responders: who achieved SVR, were 29 patients, 19 males and 10 females.
(b) Nonresponders: who did not achieve SVR, were 21 patients, 13 males and 8 females.
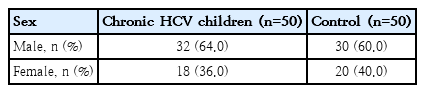
(2) Healthy control group. Fifty healthy children (30 males and 20 females), with matched age were considered as control group (Table 1).
The mean age was 11.35±3.13 years among patients group with CHC, while in normal control group the mean age was 11.47±4.12 years. Body mass index (BMI) was 19.1±3.3 kg/m2 in diseased group while control group has BMI of 19.6±2.9 kg/m2 (Table 2).
At the end of 24 weeks treatment with combined therapy of IFN plus ribavirin, the mean level of FT3 was 4.24±0.33 pmol/L (range, 3.5–5.5 pmol/L), FT4 was 17.05±29.00 pmol/L (range, 10.0–26.0 pmol/L), TSH was 3.23±88.00 mU/mL (range, 0.4–4.0 mU/L), while the basal level (before starting treatment) FT3 was 4.42±0.50 pmol/L, FT4 was 17.44±0.24 pmol/L, and TSH was 1.16±0.77 mU/mL (Table 3).
TSH level at the end of treatment (patient group) was less than 4 mU/ml in 36 patients, 4 to <10 mU/mL in 13 patients and >10 mU/mL in one patient only. Then mean TSH was 3.23±88 mU/mL in Pegylated interferon treated children at the end of treatment, while its mean value was 1.09±0.92 mU/ml in control group, P value <0.01 (Table 4), also in the same treated group mean TSH was 1.16±0.77 mU/mL before therapy and 3.23±88 mU/mL at the end of treatment, P-value <0.01(Table 3).
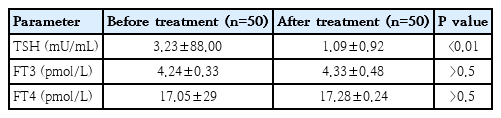
Serum TSH, FT3, and FT4 in the interferon treated group (at the end of treatment) compared with normal control group
In responders, at the end of therapy (24 weeks), FT3 was 4.6±0.33 pmol/L, FT4 was 17.53±0.61 pmol/L, and TSH was 3.34±0.74 mU/mL (Table 5). Nonresponders’ group at the end of therapy (24 weeks), FT3 was 4.51±0.52 pmol/L, FT4 was 17.67±0.50 pmol/L, and TSH was 3.29±0.82 mU/ml (Table 5).

Serum TSH, FT3, and FT4 of Interferon treatment responders and nonresponders at the end of treatment
Antithyroglobulin antibodies and antithyroid peroxidase antibodies were done only in 1 patient (TSH: 14 mU/mL). It was negative.
Hypothyroidism can be classified into grades I, II, and III. Grade1 (subclinical hypothyroidism), can be subclassified into grade IA (TSH >4.0 to <10 mU/L) and grade IB (≥10 mU/L). Grade II is characterized by elevated TSH associated with decreased FT4 level. Grade III is characterized by elevated TSH and decreased level of both FT4 and FT3.8)
Our study showed that 28% of children received combined PEG IFN-α plus ribavirin showed subclinical hypothyroidism. Those patients were referred to endocrinologists for follow-up. No one of our patients showed manifestations of hyperthyroidism.
Discussion
Thyroiditis is one of the most common side-effects of IFN-α therapy. In our study subclinical hypothyroidism was observed in 26% of children received combined PEG IFN-α plus ribavirin. TSH ranged between 4–10 mU/mL in 26%, while it was >10 mU/mL in 2%. This runs in harmony with other study [9], who reported subclinical hypothyroidism in 20%–40% of patients and clinical hypothyroidism in 5%–10%.
In our current study, the overall incidence of thyroid dysfunction was 28%. All affected cases showed hypothyroidism, most of them are subclinical. No cases were reported with hyperthyroidism or biphasic thyroiditis. That was different with Moncoucy et al. [10], who reported 2.8% of total patients (15% of positive cases) showed biphasic thyroiditis. This difference may be due to different age groups.
The pathogenesis of IFN-induced thyroid diseases is due to dysregulation of the immune system by IFN, as well as its direct effects on thyroid cells. Increased expression of IFN-γ and chemokine ligand 10 has also been reported in patients with autoimmune thyroiditis and hypothyroidism. Our study did not show any positive autoantibodies, in difference with other studies [11] that reported the incidence of interferon-induced thyroid autoimmunity from 2.5% to 42%. That may be due to the fact that he studied different age group. Most of our patients were pubertal males. Carella et al. [12] documented a genetic predisposition to thyroid autoimmune disease is probably necessary for the development of thyroid disease in patients treated with IFN.
Some studies demonstrated that HCV patients with positive autoantibodies at the initiation of therapy have an 80% probability of developing thyroid disease during or after therapy [13], while in our study only one patient investigated for autoantibodies.
Ribavirin is a synthetic guanoside nucleoside analog. It has immunomodulatory effects by inducing Th1 cytokines in the immune response against HCV infection (Tam RC). The mean incidence of thyroid dysfunction in patients treated with IFN-alpha plus ribavirin therapy is higher than in those treated with IFN alone. Ribavirin could induce hypothyroidism by Th1-dependent activation of CD8+ T lymphocytes which induce cellular destruction predominantly by the perforin pathway [14].
In the current study, patients received PEG IFN-α plus ribavirin had statistically significant difference regarding the level TSH at the end of treatment in comparison with normal control group (Table1). There was statistically significant difference in same patients group before starting treatment and at the end of treatment (Table 2). Fourteen patients showed elevated TSH level, with statistically significant difference (P<0.01). TSH level ranged from 4–10 mU/mL in 13 patients while it was more than 10 mU/mL in 1 patient only. Both FT4 and FT3 did not show any statistical difference between the 2 groups. So, 30% of children received combined PEG IFN-α plus ribavirin showed subclinical hypothyroidism. No one of our patients showed clinical hypothyroidism, thyroid antibodies, or manifestations of hyperthyroidism. These findings differ from other study report by Monzani et al. [15] He studied 31 patients with multiple sclerosis whom received 1-year interferon therapy. His results showed that 5 patients were affected by Hashimoto’s thyroiditis at baseline, 8 developed thyroid dysfunction and/or autoimmunity of various degrees during IFN-b1b treatment, while 18 did not develop any thyroid abnormality. This difference may be explained by different age group, duration of treatment in addition to different interferon used.
HCV is a leading cause of chronic hepatic disease, cirrhosis and HCC. Reports stated that almost 170 million persons all over the world are infected with HCV with a global prevalence of about 3%. Every year there are estimates of 3 to 4 million new cases of infection due to different causes of transmission. However, it is noticed that the incidence of HCV has either declined or stabilized in recent years [16].
Chronic HCV infection has an extrahepatic presentation including hematologic diseases, renal disease, dermatologic conditions (such as lichen planus), porphyria, cryoglobulinemia, lymphoma, autoimmune disorders (such as thyroiditis), and the presence of autoantibodies [17].
Antonelli et al. [18], reported that thyroid disorders are common in patients with chronic HCV, particularly women. Antithyroid antibodies were present in 5%–17% of patients. Thyroid diseases, primarily hypothyroidism, occur in 2% to 13% of patients and up to 25% have thyroid antibodies.
This study did not find any corelation between chronic HCV infection in children and thyroid disease as no one of our patients had any thyroid disturbance before initiating therapy. Other studies failed to show that HCV is an independent factor for thyroid diseases, although the rate of antithyroglobulin positivity in HCV patients was higher than healthy controls [19].
Further studies on larger number of patients and longer follow-up duration are recommended for further confirmation of our findings. It may be advisable to follow thyroid functions routinely in children treated with IFN-alpha and ribavirin every 3–6 months, to interfere early if hypothyroidism was detected.
Finally, this study concluded that there is an association between subclinical thyroid dysfunction and treatment with IFN-alpha and ribavirin in children.
Notes
No potential conflict of interest relevant to this article was reported.