Review of epidemiological studies on air pollution and health effects in children
Article information
Abstract
There is a growing body of literature on the adverse health effects of ambient air pollution. Children are more adversely affected by air pollution due to their biological susceptibility and exposure patterns. This review summarized the accumulated epidemiologic evidence with emphasis on studies conducted in Korea and heterogeneity in the literature. Based on systematic reviews and meta-analyses, there is consistent evidence on the association between exposure to ambient air pollution and children’s health, especially respiratory health and adverse birth outcomes, and growing evidence on neurodevelopmental outcomes. Despite these existing studies, the mechanism of the adverse health effects of air pollution and the critical window of susceptibility remain unclear. There is also a need to identify causes of heterogeneity between studies in terms of measurement of exposure/outcome, study design, and the differential characteristics of air pollutants and population.
Key message
This review summarized the accumulated epidemiologic evidence with emphasis on studies conducted in Korea and heterogeneity in the literature. Based on systematic reviews and meta-analyses, there is consistent evidence on the association between exposure to ambient air pollution and children’s health, especially respiratory health and adverse birth outcomes, and growing evidence on neurodevelopmental outcomes.
Introduction
There is a growing body of literature on the adverse health effects of ambient air pollution [1-3]. Epidemiological studies to date have consistently reported that chronic and acute exposure to ambient air pollutants is related to an increased risk of cardiopulmonary health. Some of these studies focused on a susceptible population at higher risk posed by air pollution, which raised concerns regarding child susceptibility. Children are more adversely affected by air pollution due to their immature immune systems, their underdeveloped lung and metabolic systems, and the co-occurrence of infection with respiratory pathogens [4,5]. Children are also susceptible to air pollution because they spend more time outdoors and are more physically active, which results in exposure to a higher concentration of air pollution and increased ventilation rates [6].
Numerous systematic reviews and meta-analyses have examined air pollution and children’s health, including the World Health Organization (WHO) reports published in 2005 and 2018 [5,7]. This review is in line with previous studies that summarized and evaluated the accumulated epidemiologic evidence but puts more emphasis on studies conducted in South Korea and discusses the causes of heterogeneity in the literature. In this context, we limited the scope of this review to ambient air pollution and the most commonly investigated health outcomes.
Respiratory health
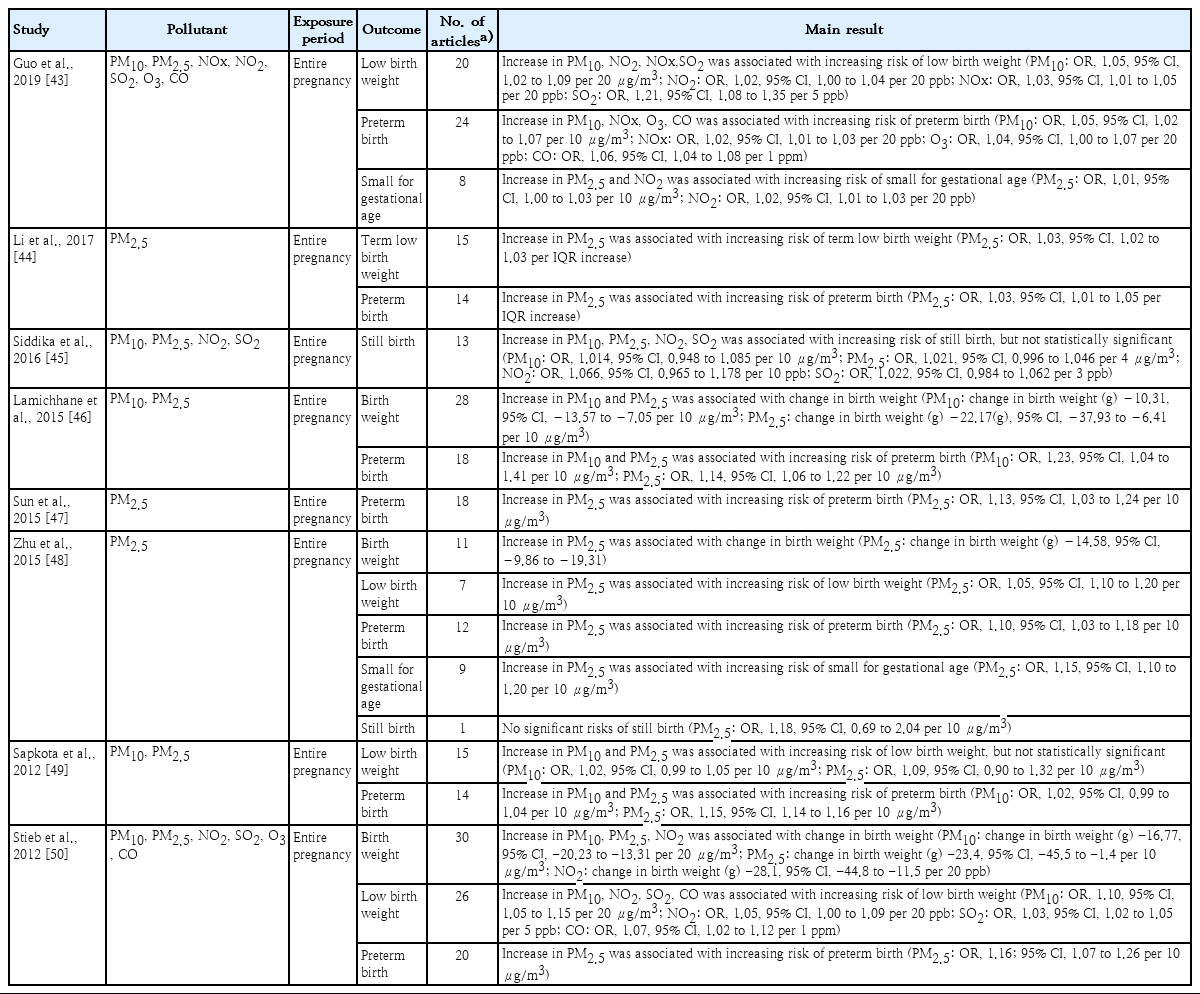
Since air pollution enters the human body through breathing, the respiratory system is primarily and directly exposed to air pollution. Numerous epidemiologic studies have investigated the respiratory effects of air pollution on children, including lung function and respiratory symptoms/diseases. The systematic reviews and meta-analyses on ambient air pollution and children’s respiratory health examined here are shown in Table 1 [8-21].
Summary of existing meta-analyses of correlation between air pollution and children’s respiratory health
Meta-analyses concluded that air pollution may adversely impact lung function. However, Ward and Ayres [8] suggested that the reliability of summary effect estimates is limited due to considerable heterogeneity and possible publication bias. They highlighted the need for further research on the causes of this heterogeneity, including an analytic approach, study population, and interactions between air pollutants. Studies on the Korean population have consistently suggested adverse effects of airborne particles on lung function [22-24]; however, making a direct comparison of the effect estimates between these studies was difficult since they used different study designs.
As concluded by the WHO report [5], the results of metaanalyses on asthma incidence and prevalence were inconsistent in terms of outcomes and individual pollutants. Anderson and colleagues conducted two meta-analyses on asthma incidence and prevalence and found that only NO2 was associated with the incidence of asthma [9,10]. In Korea, a prospective study of elementary school children showed that ambient O3 was positively associated with the 1-year prevalence of wheezing (odds ratio [OR], 1.372; 95% confidence interval [CI], 1.016–1.852; per 5 ppb) [25]. However, Yi et al. [26] did not find a significant association between traffic-related air pollution (TRAP) exposure and asthma prevalence in Seoul, Korea.
Emergency departments and hospital admissions for asthma have been used in many studies as a surrogate for asthma exacerbation. Several meta-analyses have consistently reported significant effects of air pollution on the increase in hospital utilization for asthma [11-14]. Fan et al. [11] and Zhang et al. [14] showed that the magnitude of the association between hospital utilization for asthma and exposure to air pollution was larger in children than in adults. Previous studies conducted in Korea also provided convincing evidence of the positive association of air pollutants with hospital admissions for asthma [27-32].
Studies on asthma incidence and prevalence varied in terms of exposure assessment methods, and outcome measurements were often made via questionnaire. The studies had different designs: cohort, case-control, and cross-sectional. On the other hand, every study on asthma exacerbation used hospital records to define health outcomes. They also used time-series analyses or case-crossover designs in common to evaluate the short-term effect. These differences may be the reason why evidence of the link between air pollution and asthma exacerbation is robust, while studies on asthma incidence and prevalence reported relatively large degrees of heterogeneity and inconsistent results.
One of the diseases mainly studied in relation to respiratory health is respiratory infections, including pneumonia. In a meta-analysis, Mehta et al. [15] showed that long-term ambient particulate matter (PM2.5) exposure was associated with an increased risk of acute lower respiratory infections. Short-term exposure to air pollution has also been reported to be associated with increased hospital admission or health care utilization for respiratory infections [33,34].
These respiratory health effects of air pollution can lead to school absenteeism for children. A study from Mexico City revealed that a high concentration of ambient ozone for 2 consecutive days increased the risk of school absenteeism for respiratory illness by about 20% [35]. Park et al. [36] showed that PM10, O3, and SO2 were associated with illness-related absenteeism in elementary school students in South Korea. However, the study of a cohort in southern California communities did not find a statistically significant association between school absenteeism and PM10 or NO2 [37]. Although studies on school absenteeism are limited in terms of outcome measure, these kinds of studies support the evidence that air pollution affects the respiratory health of children.
Several recent studies suggested seasonal variations in the association between air pollution and respiratory health in children. Stronger effects of air pollution were found during the cold season [34,38] or transient season [39]. These various effects of season might have been induced by a different meteorological condition affecting the distribution of air pollution or different outdoor behaviors of children affecting exposure pattern. Children’s respiratory health can also be affected by seasonal factors such as viral infections or allergens. Therefore, studies of air pollution and respiratory health for children must consider season as an important factor.
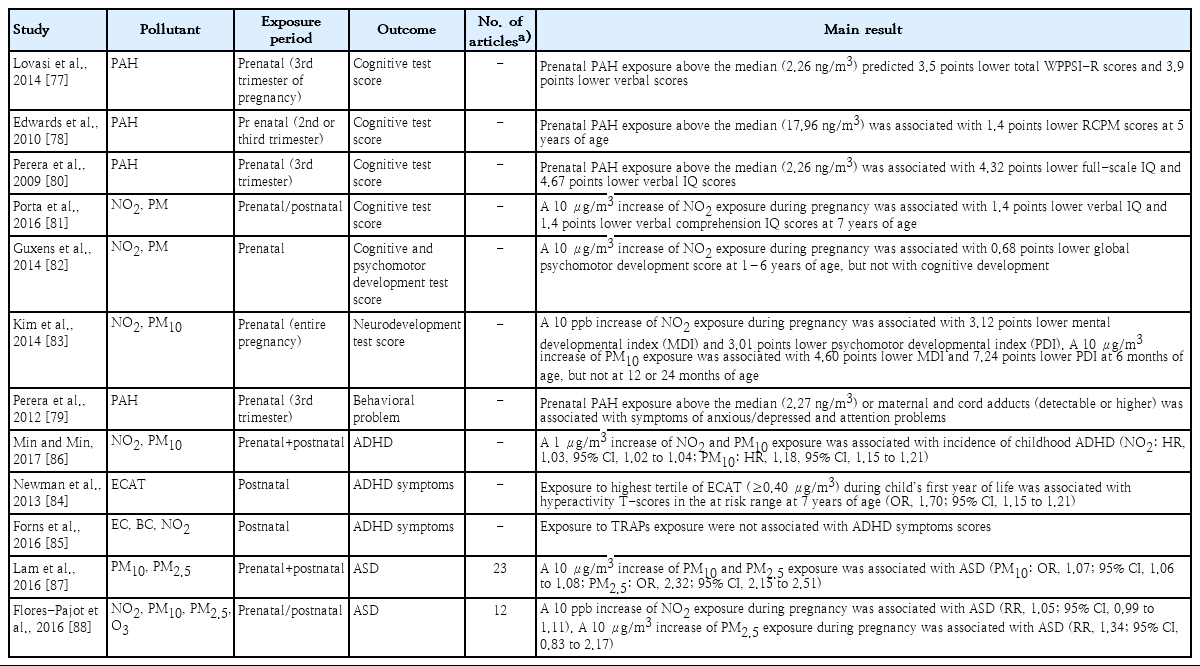
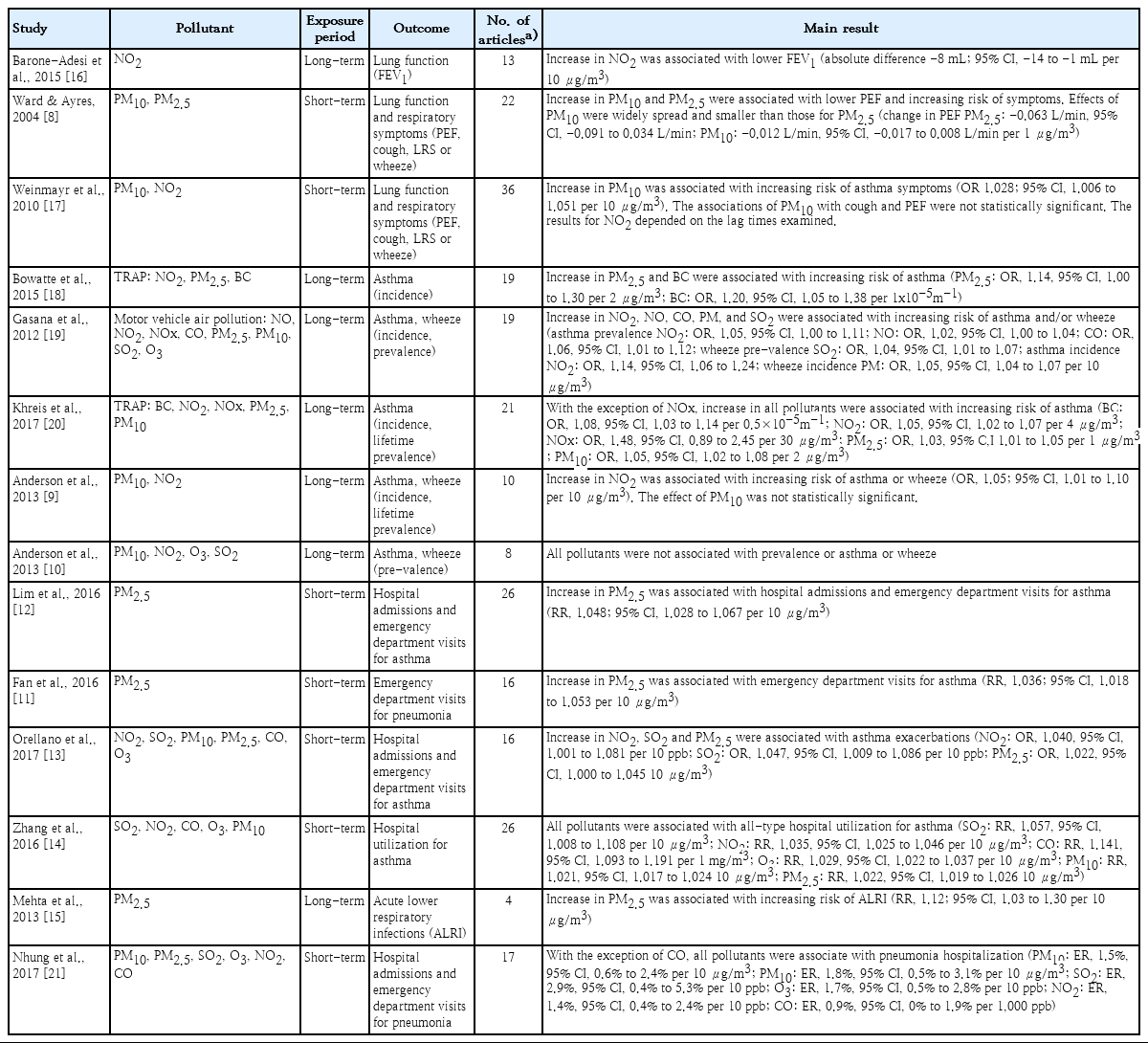
Adverse birth outcomes and early childhood mortality
Adverse birth outcomes are a matter of great concern because their effects influence health throughout life [40-42]. There is growing evidence of the associations between maternal exposure to ambient air pollution and adverse birth outcomes, including low birth weight (LBW), preterm birth (PTB), stillbirth (SB), and small for gestational age (SGA). The systematic reviews and meta-analyses considered here are shown in Table 2 [43-50]. Overall, there is compelling evidence that exposure to ambient air pollution, mainly PM, NO2, SO2, and CO, is associated with LBW, SGA, and PTB, but there is mixed evidence regarding its contributions to SB. Studies conducted in Korea also provided a consistent conclusion regarding the association between air pollution and LBW [51-53], PTB [54,55], and SB [56].
Recent studies have focused on the heterogeneity of the effects of air pollutants on adverse birth outcomes. Several studies investigated the effects of PM according to its chemical constituents to identify major contributors with detrimental health effects [57-59]. For example, a recent meta-analysis by Sun et al. [60] reported that zinc, nickel, titanium, vanadium, organic carbon, nitrate, and elemental carbon were associated with LBW. Other studies focused on population characteristics as causes of heterogeneity, such as a child’s sex [61] and maternal socioeconomic status [62]. Recent studies also considered area-level characteristics such as residential socioeconomic status [63,64] or greenness level. [65] For example, Yi et al. [66] reported that the effect of PM10 on PTB was stronger among mothers living in deprived areas after the adjustment for individual-level socioeconomic status in Seoul, Korea.
The results of previous studies regarding the critical exposure period vary according to the study population, location, and air pollutants. A recent meta-analysis showed that the association was the strongest for PM2.5 exposure in late pregnancy with LBW infants [60]. Another meta-analysis reported the highest pooled estimates for PM10 exposure in the first trimester with LBW or PTB but no notable differences for NO2 across pregnancy trimesters [43]. Studies in Korea reported the strongest associations between exposure to air pollutants in early to midpregnancy and LBW [51,52], while others reported the strongest associations between exposure to air pollution in the third trimester and PTB [54,67]. Several plausible mechanisms support early or late pregnancy as a critical period [60,68-70], but more evidence is needed to clarify the critical window of susceptibility and its biological mechanisms.
There is also strong evidence that exposure to ambient air pollution is associated with infant mortality, particularly respiratory deaths and sudden infant death syndrome (SIDS) [71-73]. In Korea, Ha et al. [74] and Hwang et al. [75] reported on the effects of acute exposure to PM10 on cause-specific mortality and SIDS, respectively. Most studies to date focused on short-term exposure to air pollution, and few have provided evidence of the effects of long-term exposure. For example, Son et al. [76] reported the association between long-term exposure to PM (total suspended particles, PM10, PM10-2.5, PM2.5) and infant mortality in Seoul, Korea.
Neurodevelopmental outcomes
Neurodevelopment is an emerging research area in air pollution and children’s health. Although evidence is still mounting, existing studies have suggested the potential associations between prenatal/postnatal exposure to ambient air pollution and neurodevelopmental effects such as cognitive development, autism spectrum disorder (ASD), and attention-deficit hyperactivity disorder (ADHD). A summary of individual studies and meta-analyses is provided in Table 3 [77-88]. There is growing evidence that exposure to air pollution, particularly TRAP, is related to cognitive and psychomotor development in children [89,90]. Several studies reported that pre- and postnatal exposure to polycyclic aromatic hydrocarbons (PAHs) [77-80,91], PM2.5, and NO2 [81,82] adversely affected cognitive development and behavior. Kim et al. [83] investigated the adverse effects of prenatal exposure to PM10 and NO2 on neurodevelopment over 24 months in Korean children. They found significant associations between PM10 and both cognitive and psychomotor development. Prenatal exposure to NO2 also adversely affected psychomotor but not cognitive development.
It is also noteworthy to highlight the association between air pollution and neurodevelopment disorders. A recent meta-analysis reported positive associations between prenatal exposures to PM10, PM2.5, NO2, and O3 with ASD. Postnatal exposure to PM2.5 and NO2 was associated with ASD. Relatively few studies investigated the associations between air pollution and ADHD; thus, those results are not yet conclusive. Newman et al. [84] found that exposure to elemental carbon attributed to traffic during the first year of life was related to higher scores of ADHD-related symptoms in children. Meanwhile, Forns et al. [85] examined the associations between exposure to TRAP, including elemental carbon, black carbon, and NO2, at school and ADHD-DSM-IV scores and found no significant associations with ADHD symptoms. In Korea, Min and Min [86] reported a significant association between exposure to PM10 and NO2 with childhood ADHD incidence, but further studies of different populations, the time window of exposure, and confounding are needed.
Overall, there is relatively consistent evidence of the associations between ambient air pollution and neurodevelopmental effects. However, there is a need to clarify the critical window of exposure in the pre- and postnatal periods. Moreover, further research must compare studies using different exposure/outcome measurements and investigate the effects of sex, age, and environmental and social conditions.
Discussion
Most studies investigating the health effects of ambient air pollution in children estimated the associations between individual air pollutants and specific health outcomes. One of the common limitations of these studies is that it is difficult to assess the effects of exposure to multiple pollutants simultaneously. In the real world, the population is exposed to a mixture of pollutants in the atmosphere, so the health effects of air pollution may have been caused by a combination of those various pollutants. However, as air pollutants are correlated and interact with each other, it remains a challenge to disentangle the independent effects of individual pollutants or comprehensively estimate the effects of mixed air pollution.
The mechanisms of the adverse health effects of air pollution on children are also complex and remain unclear. Nonetheless, the inflammatory response and oxidative stress are often suggested to play important roles. In a panel study of New York City schoolchildren, Patel et al. [92] reported that black carbo and NO2 were associated with pH and 8-isoprostane, exhaled biomarkers of airway inflammation and oxidative stress, respectively. Toxicological studies have suggested that PM may stimulate the formation of reactive oxygen species (ROS), and continuous ROS exposure can impair lung function through pulmonary inflammation [93]. It was recently suggested that epigenetic changes may be involved in mechanisms linking air pollution to health. Air toxicants may alter the methylation degree of candidate genes related to cardiovascular diseases, respiratory diseases, and cancer [94,95]. These epigenetic modifications are expected to help identify the causal correlation between air pollution exposure and children’s health.
Although the adverse effects of air pollution on health outcomes of children reviewed in this paper are generally well founded, different effect estimates or inconsistent results are often reported. There may be various reasons for heterogeneity between studies apart from analytical approaches, including study design and statistical methods. As mentioned before, air pollution is a mixture of various substances and individual air pollutants can interact with other air pollutants. The effects of individual pollutants can vary due to the different distribution of air pollutants between study areas. In particular, PM is a mixture of chemicals, unlike other gaseous pollutants. Since the toxicity of PM depends on chemical size and constituents [58,60,96,97], differences in PM characteristics between regions can be a major cause of heterogeneity among studies.
In addition to the properties of air pollution, population vulnerability can explain interstudy heterogeneity. Several studies have shown that individual sociodemographic characteristics or the local environment could modify the association between ambient air pollution and health [38,62,66]. Among various factors, age is one of the most important effect modifiers in the pediatric population. A child is usually defined as a person below the age of 18, but each study sets its own standard age. Even among populations under the age of 18, younger and older children may have different biological characteristics and outdoor activity patterns, resulting in inconsistent results between studies.
Accordingly, comparing existing studies requires an in-depth understanding of the characteristics of the study area and population. Related research has recently been underway in the Asian region and developing countries beyond the US and Europe. When researchers aggregate studies conducted in various regions, it will be important to explore how various heterogeneity factors can affect the study results. These efforts will help us understand the complex causal correlation between air pollution and children’s health, find gaps in existing research, and evolve to advanced research.
Epidemiological research on the health effects of air pollution provides scientific evidence for environmental health policy development. Environmental health policies should not only protect everyone’s health from air pollution, they should reduce the health inequality caused by air pollution. In terms of health inequality, it is essential to consider social determinants of health in relation to air pollution [98,99] because they can affect the level of exposure to air pollution and the vulnerability to air pollution. A Korean study showed that socioeconomic status measured at the individual and regional levels was correlated with air quality index [100]. Low socioeconomic status can also make individuals more vulnerable to air pollution exposure by limiting healthy behaviors or health care utilization. Therefore, future research on air pollution and children’s health should move toward considering various social contexts so that we can identify intervention points for reducing health inequality.
Conclusions
Review of the existing systematic reviews, meta-analyses, and recently updated studies revealed consistent evidence of the association between exposure to ambient air pollution and children’s health, especially respiratory health and adverse birth outcomes, and growing evidence on neurodevelopmental outcomes. Studies conducted in Korea also provided a consistent conclusion, although the number of studies remains limited.
Despite these existing studies, the mechanism of adverse health effects of air pollution and the critical window of susceptibility remain unclear. There is also a need to identify causes of heterogeneity between studies in terms of measuring exposure/outcome, study design, and differential characteristics of air pollutants and population.
Notes
No potential conflict of interest relevant to this article was reported.