Prevalence of methicillin-resistant Staphylococcus aureus in Iranian children: a systematic review and meta-analysis
Article information
Abstract
Background
Antibiotic resistance is associated with longer hospitalizations, higher treatment costs, and increased morbidity and mortality rates.
Purpose
This study aimed to determine the prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in Iranian children.
Methods
International databases, including Web of Science, PubMed, Embase, and Scopus, and Iranian databases, including Scientific Information Database (www.sid.ir), Magiran, and Iranian Database for Medical Literature (idml.research.ac.ir), were systematically searched for articles published between January 2000 and August 2019. Sources of heterogeneity were determined using subgroup analysis and meta-regression.
Results
Overall, 343 studies were identified; of them, 20 were included in the meta-analysis to estimate the pooled prevalence. The pooled prevalence of MRSA was 42% (95% confidence interval [CI], 29–55) among culture-positive cases of S. aureus, 51% (95% CI, 39–62) in hospitalized children, and 14% (95% CI, 0.05–27) in healthy children.
Conclusion
The overall pooled prevalence of MRSA in children was 42%. Appropriate infection control measures and effective antibiotic therapy are needed.
Key message
The pooled prevalence of methicillin-resistant Staphylococcus aureus (MRSA) was 42% among culture-positive cases of S. aureus, 51% in hospitalized children, and 14% in healthy children. The high prevalence of MRSA in Iranian children may be due to insufficient infection control measures in hospitals, inappropriate use of methicillin, inadequate staff training, and over-prescription of antibiotics in Iran.
Graphical abstract
Introduction
Staphylococcus aureus, a gram-positive coccus, is among the most common causes of bacterial infection in humans [1]. S. aureus is a common cause of nosocomial infection in children and adults [2]. This pathogen causes pneumonia; infections of the skin, soft tissue, and bloodstream; and invasive infections such as osteomyelitis and septic arthritis [1].
Methicillin is one of the best therapeutic choices for the treatment of S. aureus infection. However, studies have reported that the resistance of S. aureus to methicillin is increasing [3-5]. Methicillin-resistant S. aureus (MRSA) has become a major problem in children over the past few decades. Antibiotic resistance is associated with longer hospitalizations, higher treatment costs, and increased morbidity and mortality rates. Children are an important source of MRSA and may play a central role in its distribution in community and healthcare settings [6]. A study estimated that the incidence of MRSA infection in children increased 10-fold between 1999 and 2008 in the USA [7].
Several studies have reported the prevalence of MRSA in different parts of Iran; however, their results are conflicting and no comprehensive analysis has been performed to date. Therefore, a reliable study is needed to estimate the prevalence of MRSA infection in children and assist in its management in children. Thus, this study aimed to investigate the true prevalence of MRSA infection in Iranian children using a systematic review and meta-analysis.
Methods
1. Search strategy
International databases, including Web of Science, PubMed, Embase, and Scopus, and Iranian databases, including Scientific Information Database (www.sid.ir), Magiran, and Iranian Database for Medical Literature (idml.research.ac.ir), were systematically searched for relevant articles published between January 2000 and August 2019. The search was restricted to articles published in the English and Persian languages and conducted using the following keywords in the titles and abstracts: Staphylococcus aureus, S. aureus, resistance, methicillin, methicillin-resistant Staphylococcus aureus, MRSA, child*, pediatric, infant, Iran, Persian, and Persia. All keywords were searched electronically using 2 Boolean operators (AND, OR).
2. Inclusion and exclusion criteria
Two reviewers examined the search results. The article selection process consisted of 3 phases: title, abstract, and full-text. The inclusion criteria were as follows: (1) cross-sectional study, (2) use of standard methods to test methicillin resistance, (3) estimation of the prevalence of methicillin resistance, and (4) inclusion of children aged 1–14 years. The exclusion criteria were as follows: (1) interventional or other study type that did not use the cross-sectional method, (2) animal study, (3) review article, (4) consideration of other bacteria types, and (5) inclusion of individuals older than 14 years of age.
3. Quality assessment and risk of bias
The included studies were assessed for quality using the Joanna Briggs Institute Prevalence Critical Appraisal Tool [8]. This tool uses 9 items to examine the validity of the included studies in the meta-analysis. The evolution score ranged from 0 to 9, with <4 considered “low quality,” 4–6 considered “moderate quality,” and >6 considered “high quality.”
4. Data extraction
A data extraction form was designed to extract the following variables: (1) first author, (2) year of publication, (3) number of investigated patients, (4) number of S. aureus–infected individuals, (5) number of MRSA-infected individuals, (6) research environment, (7) MRSA diagnostic method, and (8) study location (province).
5. Statistical analysis
The Metaprop program was implemented to perform meta-analyses of proportions in Stata 12 (StataCorp LP., College Station, TX, USA) [9]. Heterogeneity between the included studies was quantified using the I2 statistic. Due to the high level of heterogeneity, a random-effects model was used to calculate the pooled prevalence. The estimated prevalence of MRSA is presented as percentages with 95% confidence intervals (CIs) in the forest plot.
Results
Overall, 343 studies were identified; however, after title and abstract screening and the removal of duplicate studies (n=121) and those not relevant to the prevalence of MRSA (n=179), the full-text of 41 reports was reviewed to assess for eligibility. Of those 41 studies, 21 were excluded and only 20 studies were included in the meta-analysis. The study selection and exclusion processes are presented in Fig. 1.
Flow diagram of the literature search and study selection processes. SID, Scientific Information Database; IDML, Iranian Database for Medical Literature.
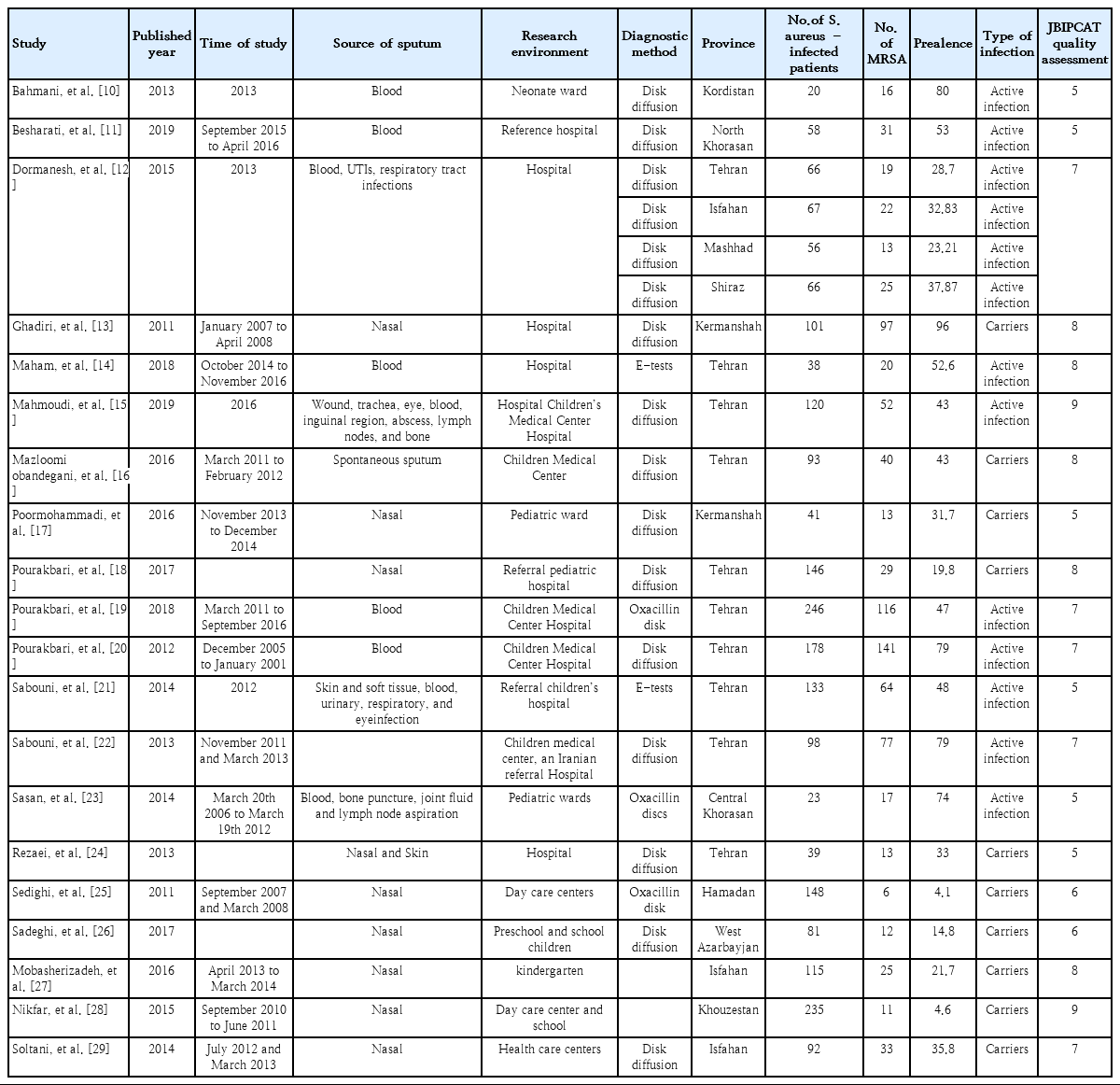
The 20 included studies were conducted in 10 provinces, including Tehran (n=9); Isfahan (n=2); Kermanshah (n=2); Tehran, Isfahan, Fars, and central Khorasan (n=1); and Hamedan, Kordistan, Azarbayjan, North Khorasan, and Khouzestan (n=6). Publication dates ranged from 2011 to 2019. The evaluation scores ranged from 4 to 9; none were scored ≤4, 8 were scored 4–6, and 12 were scored ≥7. General information and data of the articles are summarized in Table 1 [10-29].
Heterogeneity was found between studies (I2=95.36, P<0.001 for hospitalized children and I2=9415.2, P<0.001 for healthy children). The random-effects model was used in all analyses.
The prevalence of MRSA among culture-positive cases of S. aureus was 42% (95% CI, 29–55). The prevalence in hospitalized children was 51% (95% CI, 39–62), while that in healthy children was 14% (95% CI, 0.05–27) Fig. 2 shows forest plots of the prevalence of MRSA among Iranian children.
Meta-analysis of the prevalence of methicillin-resistant Staphylococcus aureus in Iranian children by research environment. ES, effect size; CI, confidence interval.
Subgroup analysis based on infection type (active or latent S. aureus infection) showed that the prevalence of MRSA in patients with active infection was 52% (95% CI, 41–63), while that of patients with latent infection was 29% (95% CI, 12–15) (Fig. 3).
Meta-analysis of the prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in Iranian children by infection type (active or latent). ES, effect size; CI, confidence interval.
A meta-regression method was used to identify the source of heterogeneity, including study period, sample source, study area, research environment (hospitalized or healthy children), and sample size. The results showed that the prevalence of MRSA was associated with the research environment (P=0.004) and study period (P=0.03).
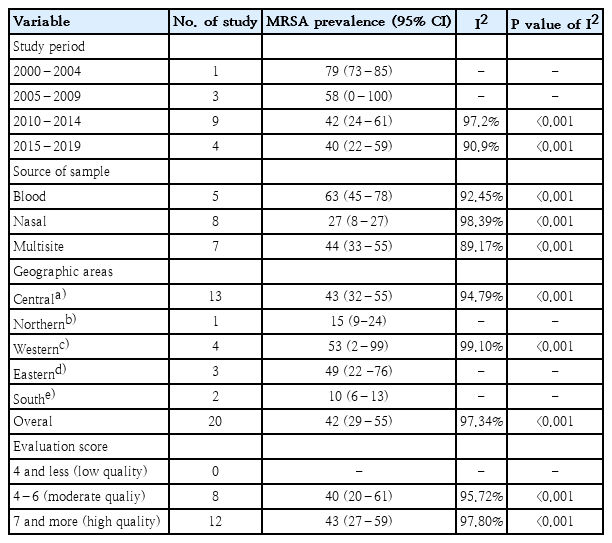
A subgroup analysis according to study period, sample source, geographic area, and evaluation score is shown in Table 2. The prevalence of MRSA decreased from the earliest to the most recent period, the prevalence in blood samples was the highest, and the prevalence of MRSA was the same in the high- and moderate-quality studies (Table 2).
Discussion
In this study, a meta-analysis was performed to determine and summarize the prevalence of MRSA in Iranian children. The prevalence of MRSA among culture-positive cases of S. aureus was 42% (95% CI, 29–55), that among hospitalized children was 51% (95% CI, 39–62), and that among healthy children was 14% (95% CI, 0.05–27).
This study revealed that the prevalence of MRSA was 14% among healthy children recruited from the community, which is much higher than the values reported in China (3.9%) [30], Vietnam (7.9%) [31], and Taiwan (3.5%–3.8%) [31] but lower than that reported in India (16.5–23.5) [31]. In addition, the prevalence of MRSA among children recruited in the hospitals was 51%, much higher than that reported in China (4.4%) and the Asia-Pacific region (0.7%–10.4%). The high prevalence of MRSA in Iranian children may be due to insufficient infection control measures in hospitals, inappropriate use of methicillin, inadequate staff training, and the over-prescription of antibiotics in Iran [32]. Another important reason for the high prevalence of MRSA in Iran is the lack of a good microbiology diagnostic facility for diagnosing infections. Most of the included studies in this meta-analysis used disk diffusion or the Kirby-Bauer method for MRSA detection. However, based on Clinical & Laboratory Standards Institute guidelines, this method is not accurate or reliable for MRSA detection [33,34].
Overlap of the prevalence of MRSA in Iranian children was 42%, the same as that in Iranian adults [35]. Nevertheless, in China, the prevalence of MRSA in adults [36] was higher than that in children [30].
The results of the subgroup analysis indicated that the prevalence of MRSA was much higher among hospitalized children than among healthy children, a result that is consistent with that of another study [30]. This can be explained by several factors such as the crowded hospital environment, increased contact between healthcare workers and patients, poor attention to infection control protocols, poor adherence to hand hygiene by healthcare workers, and placement of patients with MRSA infections with other patients in the same rooms, all of which increase the risk of MRSA transmission [37,38].
A subgroup analysis based on infection type (active versus latent) showed that the prevalence of MRSA in patients with active infection was 52%, while that in patients with latent infection was 29%. In this study, the prevalence of MRSA was lower in individuals with latent S. aureus infection than that in patients with active infection. Patients colonized with MRSA are at higher risk of developing subsequent infections [39-41] and serve as a reservoir for its transmission to others [42,43]. Therefore, active surveillance to identify MRSA carriers and eradicate MRSA colonization is essential. Subgroup analysis results showed that the prevalence of MRSA decreased from the earliest to the most recent period. One explanation for the decrease in the prevalence of MRSA in Iran is the small number of articles in 2000–2004 and 2005–2009, as only 4 studies on the subject were published before 2010.
In this study, another subgroup analysis was conducted by geographic area. The majority of the included studies in this meta-analysis were performed in Tehran (the capital of Iran located in the central part of Iran) since many referral hospitals are located in this city and many patients are referred to these hospitals from different parts of the country to seek diagnosis and treatment.
This study has several limitations. First, because the prevalence of MRSA was not studied in different regions of Iran, our results cannot indicate the nationwide prevalence of MRSA. Second, there was a potential for publication bias similar to that seen in other meta-analyses, and only published studies were included in this review. Third, there was significant heterogeneity among the included studies. Although the data were analyzed according to subgroups of geographic areas, study period, study sample, and sample size, the heterogeneity was not significantly decreased.
In conclusion, in this systematic review and meta-analysis, we summarized the high prevalence of MRSA in Iranian children. We found that the prevalence of MRSA was higher in hospitalized children than in healthy children and higher in individuals with active infection than in those with latent infection. These results highlight that infection control programs in Iran are ineffective and that appropriate infection control measures and effective antibiotic therapy are needed to control the spread of MRSA in Iran.
Notes
No potential conflict of interest relevant to this article was reported.