Effectiveness of obesity interventions among South Korean children and adolescents and importance of the type of intervention component: a meta-analysis
Article information
Abstract
Background
Various interventions have been tested to prevent or treat childhood obesity in South Korea. However, the overall effect of those interventions is unclear, as very few reviews and meta-analyses were specific to Korean children and adolescents.
Purpose
We aimed to examine the overall effect of obesity interventions among Korean children and adolescents, while also examining differences by sex, age group, baseline weight category, intervention duration, number of intervention components, and type of intervention components.
Methods
A meta-analysis was conducted for all intervention studies sampling Korean children and adolescents, with at least one control group and one month of follow-up, published between January 2000 and August 2020. Cohen d was calculated as an effect size for treatment effect, using the standardized difference between intervention group’s body mass index (BMI) change and control group’s BMI change.
Results
The final sample included 19 intervention studies with 2,140 Korean children (mean age, 12.2 years). Overall, interventions were strongly favored over their controls (d=1.61; 95% confidence interval [CI], 1.12–2.09). The subgroup analysis showed that interventions with at least one physical activity component (d=2.43; 95% CI, 1.63–3.24) were significantly better than those that did not include physical activity (d=0.02; 95% CI, -0.26 to 0.31).
Conclusion
Type of intervention component appeared important, though no differential association was observed by sex, age, baseline weight category, intervention duration, and number of intervention components. Korean and non-Korean interventions may be substantively different. Additional studies are needed to understand why and how Korean interventions differ from non-Korean interventions.
Key message
Question: What is the overall effect of obesity interventions among Korean children and what affects their effectiveness?
Finding: Interventions were strongly favored over controls. Interventions including at least one physical activity component were significantly better than those that did not. Sex, age, baseline weight category, intervention duration, and the number of intervention components were not significant.
Meaning: Future obesity interventions for Korean children must seek to include physical activity components.
Graphical abstract.
Introduction
The childhood obesity epidemic has become a major public health issue internationally [1]. According to the World Health Organization, more than 340 million children and adolescents in the world had overweight or obesity in 2016, and the global prevalence of childhood obesity has sharply increased in recent years [2]. The childhood obesity epidemic is of major concern not only to Western countries but also to Asian countries [3]. Research has shown that the prevalence of childhood obesity was highest in Asia among developing countries [4]. Among Asian countries, the prevalence of childhood obesity in South Korea (hereafter ‘Korea’) is high [5], and a sharp rise in the obesity prevalence among Korean children and adolescents (hereafter ‘children’) was noted over the last 3 decades [6]. Nationally representative data from the Korean National School Health Examination survey using self-reported height and weight of survey participants showed that the prevalence of childhood obesity in Korea increased from 8.7% in 2007 to 15.0% in 2017 [7].
Previous studies found that childhood obesity in Korea is associated with body dissatisfaction [6], lower self-esteem, depression [8], asthma [9], lower health-related quality of life [10], insulin resistance, and hypertension [6]. In addition to the childhood obesity-related health problems, children with overweight or obesity may be at a greater risk of excess weight during adulthood [11]. This could lead to an increased risk of cardiovascular disease [12] and several malignancies such as colorectal cancer [13] over an extended period of time.
Although various interventions have been performed to prevent or treat childhood obesity in Korea, the overall effect of those interventions remains unclear [14]. Pediatricians in Korean generally recommend multidisciplinary behavioral interventions for the treatment of childhood obesity [14], but evidence for such a recommendation is based on studies [15-18] conducted outside of Korea. In Western countries, many meta-analyses have been performed to investigate the effect of obesity interventions among adults [19-24] and children [15-18,25-27]. Very few meta-analyses [19,28] have been conducted in Korea. Furthermore, these studies included both children and adults in the meta-analyses. None of the meta-analyses solely focused on obesity interventions for Korean children. Although a recent meta-analysis [29] was performed to analyze effects of obesity interventions conducted between 2000 and 2010, many of the studies included in this meta-analysis were outdated and did not directly measure individuals’ adiposity. Moreover, the meta-analysis had an insufficient number of studies on adolescents (i.e., only 3 studies included middle and high-school students), was missing quality assessment of included studies, and was missing subgroup analyses by age and sex.
Given the lack of recent studies, the purpose of this meta-analysis was to address this gap in the literature by quantitatively investigating the effect of obesity interventions for Korean children and adolescents. We also explored possible sources of heterogeneity among interventions, by documenting how individual (e.g., sex, age group, and baseline weight category) and intervention characteristics (e.g., intervention duration, number of intervention components, and type of intervention components) affect interventions’ effectiveness. Surgical and pharmacological treatments are beyond the scope of this meta-analysis, as we have focused on interventions geared toward lifestyle and behavioral modification.
Methods
1. Search strategy
Systematic literature searches involved electronic keyword search of the following 8 databases, via EBSCOhost: MEDLINE; Science Citation Index; Science Direct; CINAHL Plus; Social Sciences Citation Index; APA PsychInfo; SPORTSDiscus; and Educational Resource Information Center. Search terms were a combination of obes*, overweight, fat, BMI, body, mass, weight*, Korea*, child*, adolescen*, youth, intervention, and trial. Manual search was conducted for a comprehensive coverage of the literature, by reviewing all references in eligible studies. A flowchart of study search and selection is shown in Fig. 1, using the template provided by the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline [30].
2. Inclusion and exclusion criteria
Studies were selected if they met all of the following inclusion criteria: (1) peer-reviewed primary studies with full-text availability, published in English or Korean language between January 2000 and August 2020; (2) sampling Korean children and adolescents, aged 2–21 years; (3) intervention studies with at least one control group and one month of follow-up; and (4) studies with data on mean body mass index (BMI) change between baseline and follow-up.
Studies were excluded if they met any of the following exclusion criteria: (1) studies with cross-sectional design, less than one month of follow-up, or no control group; (2) studies with data or cohort overlapping with another study; (3) studies with unclear demographics information, to assure that findings were applicable to the Korean population; and (4) studies that primarily sampled ungeneralizable populations (e.g., foreign individuals with Korean heritage, immigrants and visitors in Korea, and individuals who are incarcerated or hospitalized long term). We further excluded studies that reported only body mass, BMI percentile, BMI z score, or percent adiposity change, after sensitivity analysis found a significant difference between studies that directly reported BMI change and those that used estimated BMI change. We also excluded one study that used nonstandard formula to calculate BMI. As shown in Fig. 1, of the 382 identified articles that seemed to provide relevant information, 19 fulfilled the inclusion criteria and were thus included in this paper. The majority of included studies were randomized controlled trials, though three [31-33] were quasi-experimental by design, and one had unclear randomization protocol [34].
3. Data extraction
Studies were reviewed by investigators to extract and summarize relevant data. Data extracted from each study included: (1) general information, such as author names and year of publication; (2) study characteristics, such as study design, sample size, and length of follow-up; (3) participant characteristics, such as age and sex; and (4) estimates of BMI change and 95% confidence intervals (CIs), or numbers needed to calculate BMI change and 95% CI. When BMI values were not directly reported, they were manually calculated using the formula: BMI=weight (in kg)/height2 (in meters).
When there were multiple studies published from one research cohort, data were extracted from the study that reported more details and had more information for quality assessment. When there were more than one follow-up data point, the data point that immediately followed the end of the intervention was used.
Information on participants’ sex, age group, and baseline weight category were extracted for subgroup analysis. The number of intervention components, type of intervention components included, and intervention duration were also extracted for subgroup analysis. Sex (boy vs. girl), age group (children vs. adolescent), and baseline weight category (under/normal weight vs. overweight/obesity) were each recoded as dichotomous variables. Baseline weight category was taken directly from each study, all of which were determined by BMI percentile or clinical diagnosis. Type of intervention component included (physical activity, group education, counseling, family support, and other component) was recoded as 5 separate binary (yes vs. no) variables. The number of intervention components (1 vs. 2 vs. 3 vs. 5) and intervention duration (1–2 months vs. 3–4 months vs. 5 or more months) were respectively recoded as 4-category and 3-category variables.
When recoding participants’ age, definitions provided by the American Academy of Pediatrics were adapted to differentiate children and adolescents, such that children were individuals between ages 2–12 (typically attending pre- or elementary school), and adolescents were non-adults aged 13 or older (typically attending middle- or high school) [35].
4. Bias assessment
Risk of bias for each study was assessed using the Cochrane Collaboration tool [36], which guided interpretation of the study results. Criteria for assessment included: sequence, allocation, blinding-person, blinding-measurement, completion, and selection. Studies showing clear bias in any one of these criteria were marked with a minus (-) sign, while studies with practice that minimize bias were marked with a plus (+) sign. Studies were then assessed for overall quality, where studies with poor overall quality were excluded from final analysis. Studies included in final analysis were also tested for publication bias by plotting and visually inspecting precision funnel plot, followed by Begg test. Duval and Tweedie trim and fill were attempted for imputation and correcting publication bias.
5. Data analysis
Methods used for data analysis were modeled after an earlier meta-analysis [25]. Each study was used as a unit of analysis for the overall treatment effect. Cohen d was calculated as an effect size for treatment effect in each controlled study. Cohen d was computed by dividing mean differences of intervention and control groups by the average baseline standard deviation of the 2 groups [37]. Positive effect sizes mean favorable changes in comparison with the control group. Random effects model was used over fixed effects model due to relatively high degree of heterogeneity among studies. Heterogeneity was determined by conducting Cochran Q tests and examining I2 statistics, where I2 values of 25, 50, and 75 correspond to small, moderate, and large heterogeneity [38].
Subgroup analysis was performed among studies with available data to identify the potential source of heterogeneity. Sex, age group, baseline weight category, the number of intervention components, intervention duration, and type of intervention components were included as independent moderating variables for subgroup analysis. Each subgroup analysis included a test for between-groups heterogeneity [39]. All analyses were performed using Comprehensive Meta-Analysis software version 2.0 (Biostat Inc., Englewood, NJ, USA) [40].
Results
1. Descriptive statistics
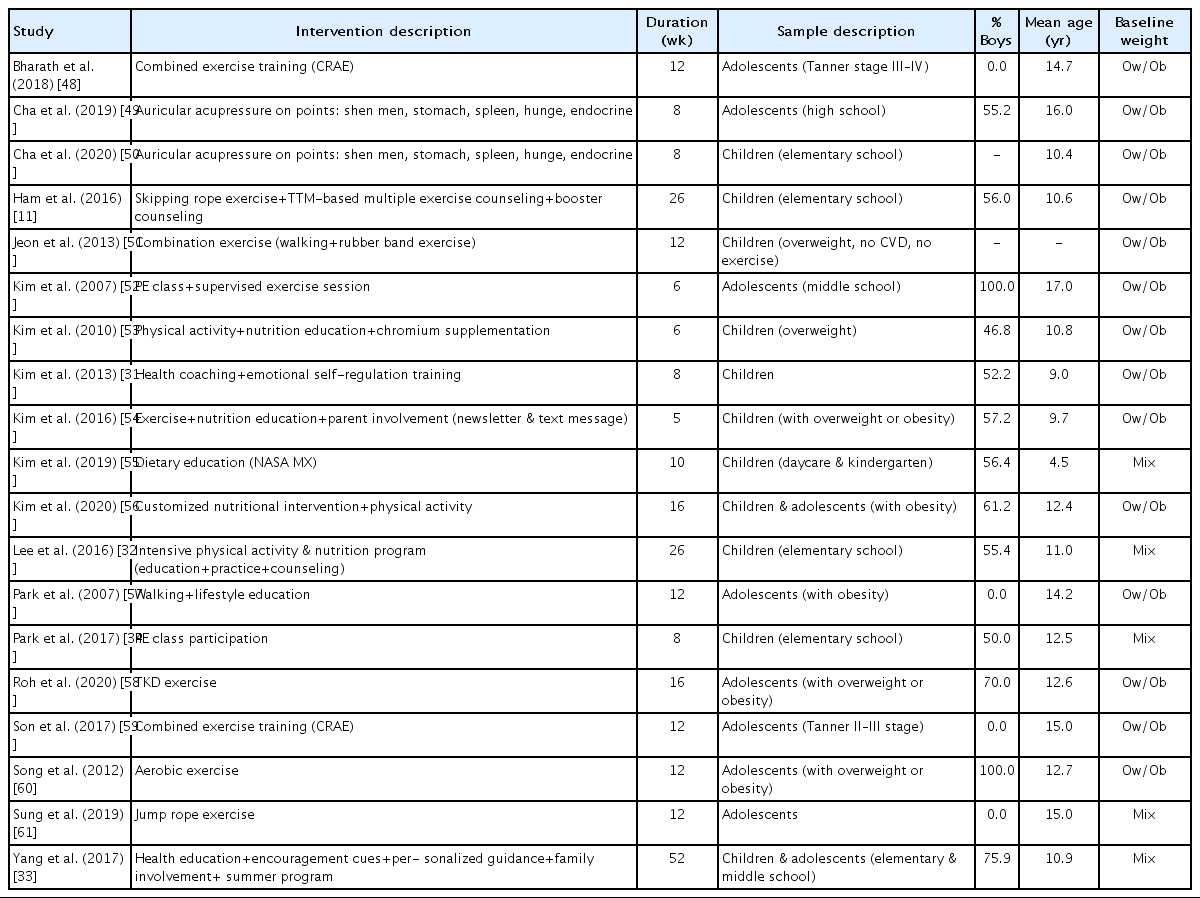
This meta-analysis included 19 intervention studies, involving 38 study arms (19 treatment arms and 19 control arms), with 2,140 Korean children and adolescents. The number of total study participants ranged from 20 to 768 (mean, 113 participants). The mean age of participants ranged from 4.5 to 16.0 years (mean, 12.2 years) at baseline, and the mean intervention duration ranged from 5 weeks to 1 year (mean, 15.4 weeks).
Of the 19 studies, 2, 4, and 13 studies sampled boys only, girls only, and both boys and girls, respectively. Of these 19, 14 sampled only participants with overweight or obesity at baseline, while 5 used participants regardless of their baseline body weight. Nine studies sampled only children, 8 sampled only adolescents, and 2 sampled both children and adolescents.
Ten studies used one-component interventions, 4 two-component interventions, 4 three-component interventions, and only 1 study used five components (Yang et al.’s study) [33]. Regardless of the number of intervention components, there were a total of 14 studies with at least one physical activity component as part of its intervention, and 5 studies that did not have a physical activity component. Nine studies had at least one group education component, while 10 did not have an education component. Five had a counseling component, while 14 were missing a counseling component. There were also 2 studies with, and 17 without, a family support component. Three had other atypical components (i.e., 1 chemical supplementation and 2 acupressure treatment), while 16 did not have any of those components. Characteristics of included studies are summarized in Table 1.
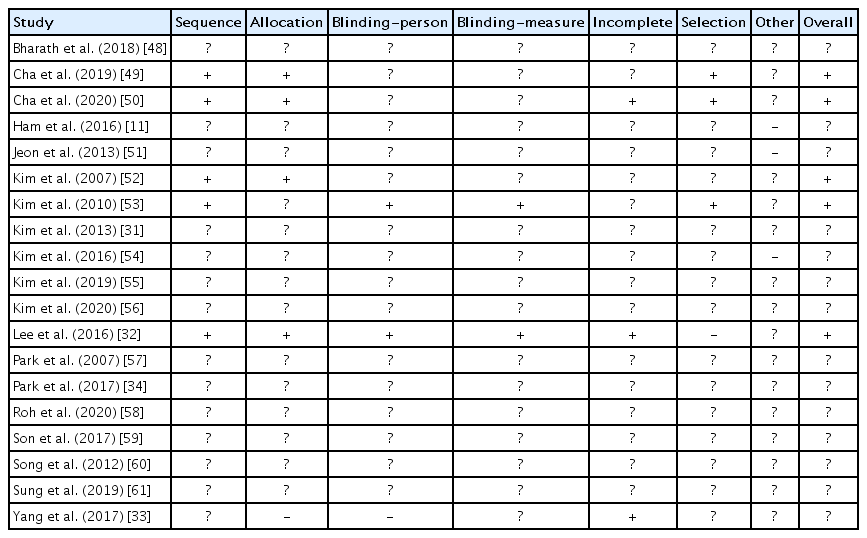
2. Bias assessment
Quality assessment is summarized in Table 2. Studies generally showed unclear risk of bias under each category. We found a sign of publication bias among included studies, based on asymmetrical distribution of the precision funnel plot (see Fig. 2) and Begg test (1-tailed P<0.01). However, the point estimate did not notably change after inclusion of imputed studies using Duval and Tweedie trim and fill.
3. Effect of interventions on BMI
Overall, a significant treatment effect was observed. Combined effect size was 1.61 (95% CI, 1.12–2.09; I2=94.8; P<0.001) in the random-effects model, indicating a significant BMI reduction in the intervention-treated group compared to the control group. BMI change ranged from -3.00 to 0.79 for the intervention group (mean, -0.80), and -2.00 to 1.08 for the control group (mean, 0.09). Summary of intervention components and effect size data are found in Table 3 and Fig. 3.
4. Subgroup analysis
1) Comparison by participants’ sex, age group, and baseline weight category
Significant treatment effect was observed in boys and girls among 6 studies reporting sex-specific data. In both sexes, significant BMI reduction was observed in intervention groups compared to their controls. Among 6 studies with sex-specific data, 2 reported data on boys, with an effect size of 1.94 (95% CI, 0.44–3.45; I2=78.1; P=0.011). Four reported data on girls, with an effect size of 3.53 (95% CI, 2.21–4.86; I2=86.4; P<0.001). Despite significant treatment effect, the magnitude of effect sizes did not significantly differ in boys and girls, and no between-groups heterogeneity was observed (P=0.12).
Among 17 studies reporting age-group specific data, treatment effect was significant in both age groups (i.e., children and adolescents). Among these 17 studies, 9 reported data on children, with an effect size of 1.39 (95% CI, 0.63–2.15; I2=93.9; P<0.001). Eight reported data on adolescents, with an effect size of 2.38 (95% CI, 0.93–3.83; I2=95.3; P=0.001). No significant difference was observed by participant’s age group (P=0.12).
Treatment effect was significant regardless of participants’ baseline weight category, when examining all included studies. Fourteen studies that sampled only participants with overweight or obesity at baseline had an effect size of 1.88 (95% CI, 1.10–2.66; I2=93.6; P<0.001), while 5 studies that sampled participants across all weight categories had an effect size of 1.17 (95% CI, 0.51–1.82; I2=95.8; P<0.001). However, no significant difference was observed between the 2 groups (P=0.17) (Supplementary Figs. 1-4)
2) Comparison by number, duration, and type of intervention components
The number of intervention components was a significant moderator, showing significant treatment effect across all levels. Effect sizes were 1.63 (95% CI, 0.73–2.54; I2=95.3; P<0.001) for 10 one-component studies, 1.33 (95% CI, 0.25–2.40; I2=90.0; P=0.015) for 4 two-component studies, 3.05 (95% CI, 1.09–5.01; I2=95.6; P=0.002) for 4 three-component studies, and 0.20 (95% CI, 0.06–0.34; I2=0.00; P=0.006) for 1 five-component study. Total between-groups heterogeneity was significant at P<0.001.
Intervention duration was significant across all levels, with effect sizes of 1.10 (95% CI, 0.10–2.10; I2=92.7; P=0.032; n=7) for interventions lasting 1–2 months, 2.19 (95% CI, 1.13–3.26; I2=95.9; P<0.001; n=9) for 3–4 months, and 1.71 (95% CI, 0.12–3.30; I2=97.1; P=0.035; n=3) for 5 or more months. However, total between-groups heterogeneity showed no significance (P=0.340), and intervention duration was not a significant moderator.
When considering different types of intervention components, only 2 (i.e., physical activity component and family support component) out of 5 components were significant moderators (both P<0.001 for tests of between-groups heterogeneity). Studies with at least one physical activity component in its interventions showed significant treatment effect (effect size=2.43; 95% CI, 1.63–3.24; I2=92.1; P<0.001; n=14), while no significant effect was found in studies with no physical activity component (effect size=0.02; 95% CI, -0.26 to 0.31; I2=80.3; P=0.868; n=5). Studies showed significant treatment effect whether or not they included a family support component. However, the magnitude of treatment effect was greater in studies without family support, such that effect sizes were 0.20 (95% CI, 0.07–0.34; I2=0.00; P=0.004; n=2) for studies with a family support component, and 1.91 (95% CI, 1.23–2.59; I2=95.2; P<0.001; n=17) for studies without a family support component. None of the remaining 3 moderators (i.e., group education, counseling, and other component) showed significant between-groups heterogeneity (respective P’s=0.391, 0.148, and 0.745).
Discussion
Many interventions have been conducted to address childhood obesity in Korea. However, no reviews have been published that have compiled the scientific evidence about the effectiveness of childhood obesity interventions in Korea. To best of our knowledge, this is one of the first meta-analyses to examine the combined effect of obesity interventions in Korean children and adolescents. We also conducted subgroup analyses to explore possible source of heterogeneity. This review is important to help inform research, policy, and practice pertaining to childhood obesity interventions in Korea.
We found that, overall, intervention group children showed more favorable changes than control group children, as the 2 groups differed by 1.61 standard deviations. Our findings had the direction of effect that was consistent with earlier meta-analyses [25,29], but the magnitude of effect was notably greater than the one found in U.S. minority children (median effect size=0.16) [25]. Such difference may be attributed to the limitations of studies included in our analysis. We found evidence of publication bias, suggesting that obesity interventions in Korean children may have been unpublished if they showed small or negligible effect sizes, which in turn exaggerated the effect found in our analysis. This is consistent with findings of an earlier meta-analysis, which had relaxed inclusion criteria (therefore included data from interventions not published in scientific journals), showed no sign of publication bias, and had relatively smaller effect sizes [29].
Despite the number of moderators we explored in our subgroup analysis, most of those moderators were not statistically significant. We found that, in Korean children, obesity interventions had equal effect regardless of participants’ sex, age, and baseline obesity status, while an earlier meta-analysis among U.S. minority children suggested that interventions limited to children who already had overweight or obesity produced greater effect sizes [25]. We also found that intervention durations and the number of intervention components do not necessarily correspond with intervention effects in Korean children, while the meta-analysis among U.S. minority children found that interventions with 3–4 components were more effective than those with only 1–2 components [25]. While further studies are needed to understand why and how the effect of Korean interventions differs from that of U.S. interventions, clinicians must take additional precaution when making recommendations based on studies conducted outside Korea. Also, it should be noted that most of the interventions included in our analyses were intended for completion in less than a year, sometimes intended for just a couple of weeks. Considering how weight regain is common in years following obesity interventions [41], interventions lasting longer than 1 year may show reduced effectiveness compared to interventions included in this meta-analysis.
We found that selection of intervention components may be of greatest importance when designing obesity interventions for Korean children. We found evidence that a physical activity component should be included whenever possible, such that it helps intervention children escape sedentary lifestyle. However, the inclusion of a counseling component (e.g., professional guidance) and a family support component (e.g., parent’s involvement) must be done carefully, as they did not show the desired or intended effect. It is possible that interventions including counseling components were sometimes improperly implemented or failed to consider the factors that affect participants’ adherence (e.g., time needed to build rapport between children and counselor). Like this study, several U.S. childhood obesity studies [42-45] reported that counseling did not play an important role in pediatric obesity. However, unlike this study, a recent meta-analysis [46] that analyzed randomized controlled trials published in English from 2008 to 2018 showed that childhood obesity interventions with parental involvement produced larger effects than those without parental involvement. According to the World Health Ogarnization [47], parents play a vital role in encouraging their children to adhere to healthy eating and physical activity which in turn is related to favorable results in obesity prevention. It is important for health educators in Korea to provide parents with health education programs that help them understand the health risks of childhood obesity. Future strategies to curb childhood obesity among Korean children should consider the vital role of parents in the prevention and treatment of childhood obesity, and rigorous evaluation of parental involvement is needed using experimental studies that focus on this topic.
Limitations of this study should be acknowledged. First, this meta-analysis compared intervention and control groups using BMI changes as the study outcome, but the 2 groups were not compared using other measures (e.g., blood pressure, fat distribution, and presence of comorbidities like diabetes) that help the clinical diagnosis of obesity. While BMI is a commonly used measure of adiposity, it does not guarantee that individuals above a certain BMI threshold for obesity are truly unhealthy and have a diagnosable form of obesity. Similarly, we do not know if interventions that effectively reduced study participants’ BMI necessarily improve the health of those participants. Second, results of this meta-analysis were not corrected for age, and our subgroup analysis only compared 2 large age groups (children vs. adolescents). As intervention effectiveness may vary by intervention target’s precise age, our age-related inference may be limited. Third, inference related to “other” intervention component may be limited, as it includes methods that are not formally recognized as clinical intervention of pediatric obesity (e.g., acupressure). Regardless, these studies cannot be omitted, as they fit our initial inclusion criteria, and sensitivity analysis found that their omission does not significantly alter our results. Fourth, there was a sign of publication bias among included studies. We sought to minimize the effect of publication bias by using imputation; however, there is still a chance that this meta-analysis does not accurately reflect how the research findings truly are if we were to include studies that were unpublished or were published in other sources (e.g., thesis, dissertation, and commercial journals) which were not included in our search. Further investigations are needed to understand why many intervention studies on childhood obesity were unpublished in Korea. Lastly, this meta-analysis focused on quantitative synthesis, but provides no qualitative synthesis. Qualitative synthesis may provide further insight into why and how Korean obesity interventions differ from obesity interventions conducted in other countries. However, we only provided a table that summarizes study quality for assessing risk of biases. A review study with in-depth qualitative synthesis of Korean obesity interventions may be needed.
In conclusion, this study showed the effectiveness of obesity interventions for Korean children. Overall, intervention groups were strongly favored over control groups, consistent with what is suggested in the literature. Sex, age, baseline obesity status, and intervention durations did not significantly affect the BMI outcome, while interventions that include at least one physical activity component were significantly better than those that did not include any physical activity components. Despite what was suggested in the literature, we found that increasing the number of intervention components does not necessarily translate into increased intervention effects. The number of published intervention studies on childhood obesity is limited in Korea. Additional intervention studies, as well as follow-up meta-analyses, are needed to confirm findings of this meta-analysis.
Supplementary materials
Supplementary Figs. 1-4 can be found via https://doi.org/10.3345/cep.2020.01620.
Notes
Funding
This research was supported by the academic research fund of Namseoul University in South Korea.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to thank librarians and undergraduate research assistants at Miami University for their help with the literature search. This paper was performed with the support of the academic research fund of Namseoul University in South Korea.