Survey of Korean pediatrician’s perceptions of barriers to and improvements in breastfeeding
Article information
Abstract
Background
Although the benefits of breastfeeding are broadly acknowledged with the efforts of the government and several medical societies, the rate of exclusive breastfeeding through 6 months is lower in Korea than in developed countries.
Purpose
This study aimed to investigate pediatricians’ perceptions of breastfeeding barriers and the current breastfeeding counseling environment and propose government policies to encourage breastfeeding in Korea.
Methods
Fourteen survey questions were developed during meetings of Korean Society of Breastfeeding Medicine experts. The Korean Pediatric Society emailed a structured questionnaire to domestic pediatricians registered as official members of the Korean Pediatric Society on May 4, 2021, and June 3, 2021. This study examined the survey responses received from 168 pediatricians.
Results
The 168 respondents included 62 professors, 53 paid doctors, and 53 private physicians. Breastfeeding was recommended by 146 Korean pediatricians (86.9%). However, only 99 responders (59%) currently provide breastfeeding counseling in hospitals. Most respondents stated providing less than 15 minutes of breastfeeding counseling time in the clinic. Moreover, 89.88% of the respondents responded that they would participate in breastfeeding counseling education if an appropriate breastfeeding counseling program was newly established.
Conclusion
This study showed that, although Korean pediatricians had a positive attitude toward breastfeeding, limited counseling was provided for parents. Along with policy support to improve the medical environment through the establishment of an appropriate breastfeeding counseling program, high-quality counseling and an increased breastfeeding rate are expected.
Key message
Question: What barriers to breastfeeding do Korean pediatricians perceive?
Finding: Regardless of medical institution, breastfeeding counseling for parents is currently limited, and breastfeeding is commonly discontinued due to various maternal and neonatal factors.
Meaning: To promote breastfeeding, increasing pediatrician participation in breastfeeding counseling with the establishment of appropriate breastfeeding counseling fees and the expansion of practical and high-quality breastfeeding education for medical staff should be considered.
Graphical abstract. Socioecological breastfeeding model.
Introduction
Breastmilk from an infant’s mother is the most appropriate, personalized form of nutrition, and many studies have demonstrated the benefits of breastmilk [1,2]. Recent findings on human milk microbiota, which is associated with the development of healthy intestinal flora and immune system in infants, and bioactive components in breastmilk not contained in the formula have underlined the importance of breastfeeding [3-5].
Although modern infant formulas have been manufactured since 1912 to replace breastfeeding for infants who are unable to breastfeed, the present rate of exclusive breastfeeding through 6 months is 25.6% in the Unites States, 37.4% in Japan, and 18.3% in Korea, indicating that formula feeding accounts for a larger proportion of infant nutrition than breastmilk [6-8].
To improve the breastfeeding rate, efforts are being made at various levels in the world. International organizations such as World Health Organization and United Nations Children’s Fund have recommended that infant should be breastfed exclusively for the first 6 months [9,10] and established the Baby-Friendly Hospital Initiative with medical communities to help mothers initiate and continue to breastfeed, encouraging other hospitals to participate [11].
In Korea, the rate of exclusive breastfeeding has decreased from 59.5% at one week of age to 5.6% after 6 months of age [6]. Many studies have been conducted on individual and interpersonal factors as barriers to breastfeeding [12-14]. The government has also made a national health promotion plan to increase the exclusive breastfeeding rate at 6 months to 77.6% by 2030 [15]. However, the still low rate of exclusive breastfeeding indicates a gap between the research community’s knowledge about the importance of breastfeeding and its practical application. In addition, there is no formal breastfeeding education for medical professionals to qualify as breastfeeding consultants, and there is no standardized breastfeeding education program for families that allows for interchangeability between medical institutions in Korea either. Pediatricians who provide primary care for infants and children in the community can more effectively inform parents about the importance of breastfeeding and resolve parental breastfeeding prejudices and grievances.
The purpose of the study was to investigate pediatricians’ perception of breastfeeding barriers and the current medical environment for breastfeeding counseling. Another purpose of this study was to propose addition government policies to encourage breastfeeding in Korea.
Methods
1. Study design, samples, and surveys
To understand the status of breastfeeding counseling in Korea, a total of 14 survey questions were developed through 3 meetings of experts affiliated with the Korean Society of Breastfeeding Medicine. The Korean Pediatric Society sent a structured questionnaire to a total of 6,000 domestic pediatricians registered as official members of the Korean Pediatric Society on May 4, 2021 and June 3, 2021 via email. The questionnaire form used Google Forms (https://forms.gle/436uySjEgArj1H659). All participants have read the rationale of this study by email and must check the box to agree before beginning this study. Each person completed the survey semianonymously as names were not requested. However, information on position within the hospital, the type of hospital they were working, and the field of specialization were collected to determine differences in responses based on their positions within the hospital.
The survey was completed by 175 respondents (2.92%). There were 62 professors, 53 paid doctors, and 53 private physicians. In addition, 3 were on leave of absence and 4 were serving in the military (Fig. 1). These 7 subjects were excluded from the analysis. The number of responses per question was not constant due to the inclusion of opinions other than suggested answers for each question.
2. Statistical analysis
To determine differences in response to the questionnaire according to responder groups, categorical variables were analyzed by chi-square tests or Fisher exact test and expressed as numbers and percentile. The level of significance was set at P<0.05. All statistical analyses were performed with Rex version 3.0.3 (RexSoft Inc., Seoul, Korea).
3. Ethics statement
This study conformed to ethical guidelines of the World Medical Association Declaration of Helsinki. The present study protocol was reviewed and approved by the Institutional Review Board (IRB) of Soonchunhyang University Seoul Hospital (IRB approval No. 2021-02-022). The need for informed consent was also waived by the IRB of Soonchunhyang University Seoul Hospital.
Results
1. Characteristics of respondents
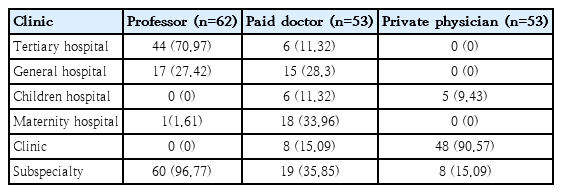
Characteristics of respondents are shown in Table 1. In the professor group, 44 (70.97%) worked in tertiary medical institutions while 17 (27.42%) worked in general hospitals. In the group of paid doctors, 18 (33.96%) worked in maternity hospitals, 15 (28.3%) worked in general hospitals. Of 53 private physicians, 48 (90.57%) worked in the clinics.
2. Current status of breastfeeding counseling in hospitals
Of 168 respondents 60 (35.71%) reported that breastfeeding counseling lasted 5 to 10 minutes, 45 (26.79%) answered that it lasted 10 to 15 minutes, and 41 (24.40%) answered that it lasted 5 minutes or less (Table 2). Rates of counseling time for 5 to 10 minutes and within 5 minutes were high in the professor group. Rates of 5 to 10 minutes and 10 to 15 minutes were high in the private physician group.
3. Breastfeeding counseling provided in hospitals currently
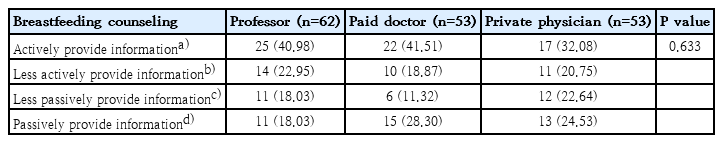
Of all respondents (n=168), 99 (58.93%) provided information about breastfeeding in the hospitals (Table 3). Twenty-five (40.98%) of the professor group, 22 (41.51%) of the paid doctor group, and 17 (32.08%) of the private physician group provided breastfeeding counseling even if there was no parental question. Fourteen (22.95%) of the professor group, 10 (18.87%) of the paid doctor group, and 11 (20.75%) of the private physician group provided breastfeeding counseling only when parents asked about breastfeeding. There were no significant differences among the 3 groups.
4. Neonatal factors and maternal factors in stopping breastfeeding
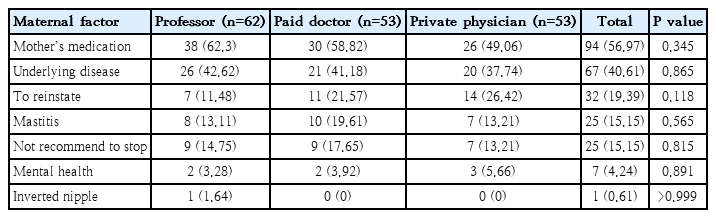
Neonatal jaundice (n=67, 39.88%) and insufficient weight gain (n=32, 19.05%) were neonatal main factors that stopped breastfeeding according to respondents (Table 4). As other opinions, 51 respondents (30.36%) stated they did not recommend mothers to stop breastfeeding. As maternal risk factors for stopping breastfeeding, mother’s medication use was the most common (n=94, 56.97%), followed by mother’s underlying disease (n=67, 40.61%) and return to work (n=32, 19.39%, Table 5). The difference in each group was not statistically significant.
5. Response to recommending breastfeeding when there is no clear medical reason to discontinue breastfeeding
Of 168 respondents, 93 (55.36%) answered that they always recommended breastfeeding, followed by 53 (31.55%) who answered they usually recommended it, and 19 (11.31%) who left it to the mother’s judgment (Fig. 2). These trends were similar in each group. Differences between groups were not statistically significant (P=0.087).
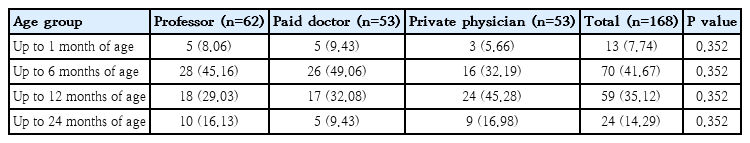
6. The age group that should be applied if the breastfeeding consultant fee is newly established
Among total respondents (n=168), 70 (41.67%) chose the age group within 6 months of age, followed by 59 (35.12%) who chose the age group within 12 months, 24 (14.29%) who chose the age group within 24 months, and 13 (7.74%) who chose the age group within 1 month (Table 6). The difference between each group was not statistically significant.
7. Appropriate breastfeeding counseling fee and participation in education for qualification
Of total respondents (n=168), 76 (45.75%) answered that it was appropriate to add the breastfeeding counseling fee which was 100% of the first-visit medical expense and 50 (30.12%) chose to add counseling fee which was 200% of the first-visit medical expense (Table 7). Nineteen (11.45%) chose to add a counseling fee which was 100% of the education fee for chronic renal failure patients. Of all respondents (n=168), 151 (89.88%) responded that they would participate in breastfeeding counseling education for qualification when an appropriate breastfeeding counseling cost was newly established.
8. Response to training time to qualify for a new fee for breastfeeding counseling
In all groups of respondents, training time of 5 hours was chosen as the most appropriate time, followed by training time of 10 hours (Fig. 3). There were no statistically significant differences among the 3 groups (P=0.465).
9. Please suggest a good opinion to improve breastfeeding
Suggestions for improving breastfeeding included the following: (1) expanding maternal and child rooming-in immediately after childbirth and reinforce breastfeeding education for workers in maternal hospitals and postpartum care centers; (2) promote breastfeeding awareness through public service advertisement and increase mass media exposure; (3) establish the environment and equipment (e.g., refrigerator) for breastfeeding or pumping breast milk at work; and (4) provide practical education on mother’s difficulties and concerns about breastfeeding besides a structured education.
Discussion
This study showed that although Korean pediatricians had a positive attitude on breastfeeding, breastfeeding counseling for parent was limited. We conducted this study using survey responses of 168 pediatricians. Currently, approximately 87% of Korean pediatricians recommend breastfeeding in hospitals. Despite the fact that ‘I did not recommend to stop breastfeeding’ was not presented as a selectable answer for neonatal factor in stopping breastfeeding, 30.36% of total respondents added this to other additional opinions. The majority (n=151, 89.88%) answered that they would participate in education for qualification if an appropriate breastfeeding consultant fee was implemented.
However, only 99 respondents (59%) were currently providing breastfeeding counseling in a hospital. The majority of respondents stated that the counseling time in the clinic was less than 15 minutes.
Neonatal jaundice and insufficient weight gain were the most common neonatal factors for pediatricians to stop mothers from breastfeeding. The most common maternal factors were medication and underlying disease. This result was similar to the factors for early cessation of breastfeeding reported in previous studies conducted on mothers [16]. Another study has reported that the lack of tertiary education, primiparity, and inconvenience/fatigue due to breastfeeding are factors for stopping breastfeeding earlier [17]. In addition, mothers who had postpartum employment were less likely to continue breastfeeding than mothers who did not, but later return to work and the highest maternal education could reduce discontinuation of breastfeeding [18,19]. In studies mentioned above, the knowledge or education of mothers about breastfeeding was reported as a common factor for maintaining breastfeeding. Furthermore, the meta-analysis of trials reported that, although low-quality evidence, providing counseling at least 4 times postnatally is more effective to prevent to stop exclusive breastfeeding before 6-month postpartum than providing counseling only and/or less than 4 times [20]. Therefore, to encourage early initiation and continuation of breastfeeding, formal and standardized breastfeeding education for breastfeeding instructors as well as mothers is needed from antenatal to postnatal periods, taking into consideration dyad characteristics of mothers and newborns [21].
Regarding the appropriate breastfeeding counseling fee, the plan of adding 100% of the first-visit medical expenses to medical expense had the highest response rate. Regarding the duration for breastfeeding counseling qualifications, education time of 5 hours was selected the most.
During the coronavirus disease 2019 pandemic, 17.9% of hospitals reduced in-person lactation support and 59.7% of hospitals provided in-person breastfeeding consultations after discharge [22]. In addition, with social distancing, the incidence of other infectious diseases has been reported to drop sharply compared to that in the past. The number of visits to the emergency room by the pediatric population in Korea has also plummeted [23,24]. This may adversely affect breastfeeding by reducing the chance of having contact with pediatricians and breastfeeding counseling opportunities, preventing support of mothers in their efforts to continue breastfeeding, and widening the knowledge disparities among mothers [12].
Thus, to promote breastfeeding, increasing the participation of pediatricians in breastfeeding counseling with the establishment of appropriate breastfeeding counseling fees and expanding practical and high-quality breastfeeding education not only to doctors, but also to medical staff in postpartum care centers and maternity hospitals need to be considered.
This study has several limitations. First, the Korean Pediatric Society sent an email for a questionnaire to a total of 6,000 official members registered. However, only a total of 175 (2.92%) responded. Secondly, to investigate the difference in respondents’ propensity for risk factors that induce them to stop mothers from breastfeeding, specific situations and cases encountered in the hospital could be presented. However, the depth and details of the questions were lacking. Lastly, we could not compare or investigate the difference in respondents’ disposition toward exclusive breastfeeding between full-term and premature infants.
In conclusion, this study investigated pediatricians’ perception of breastfeeding barriers and the current medical environment for breastfeeding counseling in Korea. Along with policy support to improve the medical environment through the establishment of an appropriate breastfeeding counseling fee, high-quality counseling and an increase in the breastfeeding rate are expected.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: YRL, HJS, YMA, SMS, YJK, Ellen AR K, YJS, DYY, SML, JYL, JAL, SHC, ESJ, EKC, JSH; Data curation: SPB, WHH; Formal analyses: SPB, WHH; Methodology: SPB, YRL; Project administration: YRL; Visulization: SPB; Writing-original draft: SPB; Writing-reveiw and editing: WHH, YRL