Impacts of maternal COVID-19 during pregnancy on neonatal health and epidemiology
Article information
Key message
Newborns born to mothers infected with coronavirus disease 2019 (COVID-19) should be closely monitored for respiratory disorders, such as transient tachypnea of the newborn, regardless of their COVID-19 test results. Further research is required of the development of infants born to mothers with COVID-19. The trends in Korea's birth rate and infant mortality rates have not been significantly affected by COVID-19.
Many studies have explored the effects of coronavirus disease 2019 (COVID-19) on newborns and fetuses of mothers diagnosed with the virus during pregnancy. These studies have consistently reported very low rates of vertical transmission to neonates or infections during delivery. Furthermore, even in cases in which infection occurs, the majority of cases are documented as asymptomatic or mild [1]. In recent studies, newborns born to mothers with COVID-19 who tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exhibited higher rates of prematurity and multiple birth. However, no cases of neonatal mortality have been reported, and there is no significant difference in the need for mechanical ventilation based on SARS-CoV-2 results [2]. In September 2023, the Korean Society of Pediatric Infectious Diseases and the Korean Society of Neonatology released a recommendation advocating standard precautions without preemptive quarantine or testing when managing babies born to mothers with COVID-19, emphasizing the importance of close symptom monitoring [3].
In clinical practice, there have been cases in which newborns born to COVID-19-infected mothers tested negative for the virus through reverse transcription-polymerase chain reaction but required oxygen therapy due to mild respiratory issues or had extended hospital stays due to reduced activity and feeding difficulties. This raised questions about whether maternal COVID-19 impacted newborns born to infected mothers but testing negative. Therefore, we thoroughly reviewed this study to compare newborns born to mothers with versus without COVID-19.
This study [4] compared the clinical outcomes between newborns born to mothers with COVID-19 who tested negative and those born to noninfected mothers (control group). The two groups were compared by matching gestational age at birth, and errors in the study results were reduced by regression analysis and controlling for other factors that may affect neonatal outcomes, including cesarean section. A significantly higher risk of transient tachypnea in the newborn, noninvasive ventilation use, and supplemental oxygen requirement were noted among neonates born to mothers with COVID-19. The authors emphasized the importance of closely monitoring respiratory symptoms in neonates born to COVID-19-infected mothers [4]. A Swedish study also reported that maternal SARS-CoV-2 infection during pregnancy was significantly associated with increased risk of respiratory disorders and other neonatal health issues [5]. Therefore, it is recommended that clinicians care for newborns while considering both the COVID-19 guidelines mentioned earlier and the results of this study.
The following points in the discussion section are also considered important and are briefly mentioned. Several studies have proposed the mechanisms underlying these symptoms. Pregnant women infected with SARS-CoV-2 have elevated levels of proinflammatory cytokines such as interleukin-6, interleukin-1β, and tumor necrosis factor-α. These cytokines can cross the placenta and induce inflammation in the fetal lungs and brain [6]. A recent study also showed placental inflammation (53.4%) and maternal vascular malperfusion (27.5%)in the placenta of COVID-19-infected mothers, while SARS-CoV-2 antigen was detected in 94.8% of placental tissues [7]. Additionally, another cohort study indicated that infants exposed to SARS-CoV-2 in utero may face an increased risk of neurodevelopmental disorders by 12 months of age [8]. Therefore, careful long-term follow-up and further research are required of the growth and development of infants born to mothers infected with COVID-19.
The effects of the COVID-19 pandemic on pregnancy, childbirth, and infant mortality vary across countries. During the pandemic, in the United States and Europe, birth and premature birth rates decreased, while low-income countries saw increases, possibly due to unplanned pregnancies resulting from interruptions in international aid projects and family planning programs [9,10]. To examine the impact of COVID-19 in South Korea, here we investigated population dynamics between the COVID-19 pandemic period (2020–2021) and previous periods using Statistics Korea data [11].
The number of births in South Korea decreased from 484,550 in 2012 to 260,562 in 2021. During the same period, the rates of premature and multiple births increased from 6.27% and 3.22% in 2012 to 9.12% and 5.38% in 2021, respectively. The neonatal and infant mortality rates per 1,000 live births continued to decrease from 1.72 and 2.90 in 2012 to 1.25 and 2.40 in 2021, respectively. The data showed no significant changes in the trends attributable to the COVID-19 pandemic (Table 1). This indicates that the COVID-19 pandemic had a minimal impact on maternal pregnancy and newborn health in South Korea.
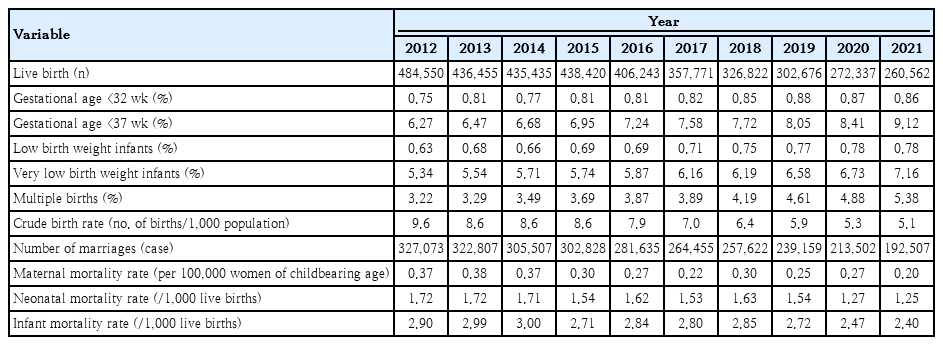
Population dynamics between coronavirus disease 2019 pandemic period (2020–2021) and previous periods
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgements
The author thank Professor Yun Sil Chang of Samsung Medical Center, Sungkyunkwan University School of Medicine and Professor Do-Hyun Kim of Dongguk University Ilsan Hospital for their valuable advice.
