Changes in frequency of benign convulsions with mild gastroenteritis and their viral causes before and during the COVID-19 pandemic: a single-center study
Article information
Abstract
Background
Benign convulsions with mild gastroenteritis (CwG) are prevalent in young children during the winter. Early in the coronavirus disease 2019 (COVID-19) pandemic, viral gastroenteritis occurrence decreased and seasonal variation was lost, which can change CwG.
Purpose
Here we investigated changes in frequency, seasonal variation, and causative viruses of CwG during the COVID-19 pandemic.
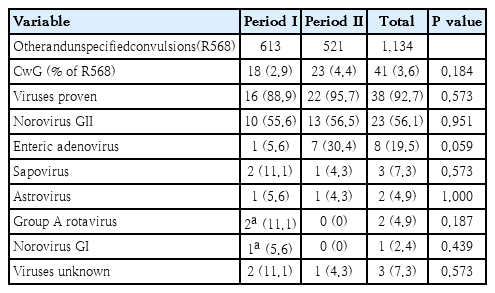
Methods
We screened 1134 patients (3–36 months) with “other and unspecified convulsions” treated at Chonnam National University Hospital between March 2017 and February 2023; of them, we enrolled 41 (3.6%) with CwG. We compared their medical records from period I (March 2017 to February 2020) to those from period II (March 2020 to February 2023). Publicly available viral gastroenteritis surveillance data from the Korea Disease Control and Prevention Agency (KDCA) were reviewed as reference.
Results
Of the 41 patients with CwG, 18 (2.9% of 613) were affected in period I versus 23 (4.4% of 512) in period II (P=0.184). In period I, CwG mainly occurred in winter and spring (55.6% and 22.2%, respectively). In period II, there were fewer CwG cases (39.1%) in winter and more cases in summer and autumn (26.1% and 17.4%, respectively): the cases of norovirus genogroup II (GII)-associated CwG increased significantly in the summer (38.5% vs. 0%, P= 0.046). Norovirus GII was the most common virus (56.1% of isolates). Enteric adenovirus was the second most common (19.5%), with one case in period I and 7 cases in period II (P=0.059). The clinical characteristics of enteric adenovirus-associated CwG were similar to those of norovirus. Seasonal changes in and viral causes of CwG were consistent with those observed in the KDCA stool surveillance data.
Conclusion
During the COVID-19 pandemic, CwG frequency did not change, seasonal variation was unapparent, and enteric adenovirus-associated CwG frequency increased.
Key message
Question: Did coronavirus disease 2019 (COVID-19) affect the frequency, seasonal variation, or virus type of benign convulsions with mild gastroenteritis (CwG)?
Findings: We compared 41 cases of CwG before and during the COVID-19 pandemic. After March 2020, frequency did not change significantly (18 patients vs. 23 patients), seasonal variation was lost, and number of cases of enteric adenovirus-associated CwG increased (1 cases vs. 7 cases).
Meaning: The COVID-19 pandemic affected CwG.
Graphical abstract. Overview of the study design and resutls. COVID-19, coronavirus disease 2019; CNUH, Chonnam National University Hospital.
Introduction
Benign convulsions with mild gastroenteritis (CwG) are afebrile situation-associated seizures that occur in infants or young children, and are associated with acute gastroenteritis [1,2]. Previous research shows that CwG presents at a similar peak age as febrile seizures in previously healthy children without serum electrolyte imbalance, hypoglycemia, or central nervous system infection [2,3]. However, they frequently occur in clusters, which is different from febrile seizures [2,3]. The long-term prognosis of children with CwG is quite good because they have normal psychomotor development after the seizures, have a very low risk of CwG recurrence, and rarely develop epilepsy [2,4,5]. When compared with febrile seizures, CwG has a lower probability of relapsing and progressing to epilepsy [2,3].
Rotavirus is frequently associated with CwG and before vaccine introduction, it was the most detected pathogen in patients with CwG [1,5-9]. Hence, the pathophysiologic mechanisms of CwG have been mainly investigated in the context of rotaviral infections, although they remain unclear [10]. However, after the introduction of the rotavirus vaccine, noroviral infections have been rising in developed countries, including South Korea [9,11-13]. Currently, norovirus is the most common CwG-associated pathogen in South Korea, which is attributable to the development of crude antirotavirus immunity [9,11,12].
Based on clinical surveillance data from the Korea Disease Control and Prevention Agency (KDCA), between March 2020 and February 2021, the coronavirus disease 2019 (COVID-19) pandemic markedly reduced the rate of enteric viral infections in South Korea [14]. In the first year of the pandemic, the incidence of enteric viral infections fell by 31.9% when compared with the previous 2 years (March 2018–February 2020). In this period, noroviral, Group A rotaviral, and enteric adenoviral infections fell by 40.2%, 31.8%, and 13.4%, respectively [14]. This trend did not vary by age [15]. Moreover, unlike in the previous 2 years, seasonal variation was not apparent in 2020 [14]. However, there are no published data for the period between the first year of the COVID-19 pandemic and now.
The marked reduction in the rate of enteric viral transmissions between children might have been caused by several factors, including improved personal hygiene, e.g., frequent hand washing, and strict social distancing, such as school closures [14-16]. Hence, we hypothesized that during the COVID-19 pandemic, the frequency of CwG in our hospital might have also changed, its seasonal variation might not be apparent and its viral causes might have changed. We investigated if there were changes in the frequency, seasonal variation, and viral causes of CwG by comparing data from 3 years before the COVID-19 pandemic (March 2017–February 2020) and 3 years during the pandemic (March 2020–February 2023). In addition, publicly available viral gastroenteritis surveillance data for the same periods were obtained from KDCA and reviewed to determine viral gastroenteritis trends in South Korea.
Methods
1. Study design and setting
This retrospective cross-sectional study compared the frequency and seasonal variation of CwG in the period between March 2017 and February 2020 (period I) with the period between March 2020 and February 2023 (period II). The stool virus types between the 2 periods were also compared, as well as the clinical characteristics of the 2 most common viruses. Periods I and II represent 3 years before the COVID-19 pandemic in South Korea and 3 years during the pandemic, respectively. The periods were subdivided into spring (March–May), summer (June–August), autumn (September–November), and winter (December–February). In addition, KDCA’s publicly available viral gastroenteritis surveillance data [17] for March 2017–February 2023 were reviewed as reference (Fig. 1).
2. Study population
We screened patients (age, 3–36 months) with ‘other and unspecified convulsions’ (Korea Informative Classification of Diseases [KOICD] code R568) [18], who received admission or emergency room treatment at Chonnam National University Hospital (CNUH) from March 2017–February 2023. CwG was given code R568 because currently, it lacks a specific KOICD code [17]. The patients’ digital medical records were retrospectively reviewed and CwG confirmation diagnosis was done for patients with the following [1,2,4-9,11,12]: (1) afebrile seizures; (2) normal development before seizure onset; (3) acute gastroenteritis; (4) normal ranges of serum glucose, electrolytes, and cerebrospinal profiles; (5) no moderate or severe dehydration; (6) short-lasting seizures that can recur within 24 hours; (7) no moderate-severe electroencephalography (EEG) abnormalities; and (8) no markedly abnormal brain images. Patients lacking sufficient information for CwG diagnosis were excluded.
Ethical approval for the study was granted by the ethics committee of CNUH (IRB number: CNUH-2023-096).
3. Data collection
The following basic clinical data were collected for each patient: age, sex, illness history, family history of seizures or developmental problems, body temperature during seizures, enteric symptoms and signs (e.g., abdominal pain, vomiting, and diarrhea), and hospital admission date and season. Specific seizure data, including seizure type, duration, and frequency, the interval between the first and last seizure, duration between the initial enteric symptoms and the seizure onset, seizure recurrence during follow-up, and post-seizure developmental problems were reviewed.
We also reviewed data on the isolated stool viruses, laboratory blood profiles (e.g., blood cell counts, blood lactate, serum uric acid, glucose, and electrolyte levels), EEG reports, and the brain images acquired at admission. Each patient’s stool virus types were determined using a multiplex real-time polymerase chain reaction test using the Seeplex kit (Seegene Inc., Seoul, Korea) and classified as norovirus genogroup I (GI) or II (GII), group A rotavirus, enteric adenovirus, astrovirus, or sapovirus.
The KDCA data [17] were reviewed and the total number of stool samples, and the number of samples positive for each virus were summarized by year and month of diagnosis.
4. Statistical analyses
Numerical values are presented as number (%) or median (interquartile range, IQR). Categorical variables between the 2 groups were compared using Pearson chi-square test. Fisher exact test was used for data involving less than 5 samples. A Mann-Whitney U test was used to compare differences between continuous variables (e.g., age and laboratory profiles) between the 2 groups. P<0.05 indicates statistically significant differences. Statistical analyses were done using IBM SPSS Statistics ver. 29.0 (IBM Co., Armonk, NY, USA).
Results
1. Frequency of CwG in periods I and II, and the basic clinical information
A total of 1,134 patients (613 and 521 in periods I and II, respectively) were diagnosed with other and unspecified convulsions (KOICD: R568). Of these, 41 patients (3.6%) with CwG (18 [2.9%] and 23 [4.4%] belonging to periods I and II, respectively (P=0.184) (Table 1) were enrolled in the study. The median age of patients with CwG was 17 months (IQR, 14.0–22.0 months). Female patients accounted for 58.5% (N=24) of the patients. The median follow-up period was 18.5 days (IQR, 8.75–321.50 days). CwG frequency was highest in 2017, 2021, and 2022 (N=9 per year, Supplementary Fig. 1).
A male patient diagnosed with norovirus GII-associated CwG at 18 months of age in period I, presented with afebrile seizure associated with astrovirus gastroenteritis at 33 months of age in period II, and was therefore counted twice. Additionally, a female patient in period I had a previous history of CwG. Four patients had febrile seizures before (2 patients) and after (2 patients) CwG. Brain magnetic resonance imaging and EEG were acquired at admission for all patients with CwG. However, genetic diagnoses for seizures were not carried out. Five patients had a family history of febrile seizures and 2 patients had family members who experienced seizures during early childhood, although it could not be determined if they were febrile or afebrile.
Based on the publicly available viral gastroenteritis surveillance data from KDCA, 10,036 and 9,273 stool samples were submitted for pathogen analyses in periods I and II, respectively, with the number of samples falling by 763 in period II. The nubmer of stool virus-proven samples was lowest in 2020 (N=495, Supplementary Table 1).
2. Seasonal CwG frequency in periods I and II
In period I, CwG were more common in the winter and spring (55.6% and 22.2% of a total number of CwG, respectively) than in the summer and autumn (11.1% for each). In period II, CwG frequency decreased during the winter (39.1%) and increased in the summer and autumn (26.1% and 17.4%, respectively; Fig. 2).

The seasonal distribution of patients with CwG in periods I (March 2017 to February 2020; gray bars) and II (March 2020 to February 2023; black bars). In South Korea, spring is from March to May, summer is from June to July, autumn is from September to November, and winter is from December to February. The frequency of norovirus GII-associated CwG (empty, upward arrows) increased significantly during the summer of period II versus period I (P=0.046). CwG, benign convulsions with mild gastroenteritis; GII, genogroup II. Norovirus GII, *P<0.05
This change in seasonal frequency was most apparent for norovirus GII-associated CwG, which, in period I, occurred during the winter and spring (N=6 and 4, respectively) only, whereas, in period II, they occurred in all seasons (38.5%, 38.5%, 15.4%, and 7.7% in the winter, summer, spring, and autumn, respectively). Notably, its frequency in period II increased significantly in the summer, comparing with period I (P=0.046) (Fig. 2). Enteric adenovirus-associated with CwG that were mostly observed in period II, were commonly detected in the winter and autumn (57.1% and 28.6%, respectively).
he seasonal distribution of virus-positive samples changed in period II when compared with period I, with the number of virus-positive samples increasing in the summer and decreasing in the spring and autumn of period II. This trend was most apparent for norovirus (Fig. 3, Supplementary Table 2).

Seasonal distribution of patients with viral gastroenteritis in periods I (March 2017 to February 2020; gray bars) and II (March 2020 to February 2023; black bars) based on publicly available Korea Disease Control and Prevention Agency stool surveillance data. The frequency of norovirus-associated gastroenteritis (empty, upward arrows) was significantly increased during the summer of period II versus period I (P<0.001). Norovirus GII, *P<0.05
3. The viruses detected in patients with CwG in periods I and II
A stool virus panel was tested for all patients with CwG. Viruses were isolated from 92.7% of all samples: 88.9% (N=16 of 18) of the samples from period I, and 95.7% (N=22 of 23) of the samples from period II (P=0.573) (Table 1). Norovirus GII was the most common pathogen and was detected in 56.1% of all samples: 55.6% (N=10) of period I samples, and 56.5% (N=13) of period II samples. Each year, except in 2018 and 2021, norovirus GII was isolated from >60% of all patients with CwG. Enteric adenovirus was the second most common pathogen and was detected in 19.5% of all samples: 5.6% (N=1) of period I samples, and 30.4% (N=7) of period II samples (P=0.059). Enteric adenovirus was mainly isolated in 2021 (66.7% of total CwG cases in 2021). Sapovirus (N=3), astrovirus (N=2), group A rotavirus (N=2), and norovirus GI (N=1) were also detected. One patient with CwG was coinfected with group A rotavirus and norovirus GI(Table 1, Supplementary Fig. 1).
Based on KDCA’s gastroenteritis surveillance data, virus pathogens were detected in 29.3% of the 10,036 period I samples and 30.3 % of the 9,273 period II samples (P=0.1114). The frequencies of norovirus, enteric adenovirus, and sapovirus increased during the COVID-19 pandemic, whereas the frequency of group A rotavirus decreased (P<0.05) (Table 2).
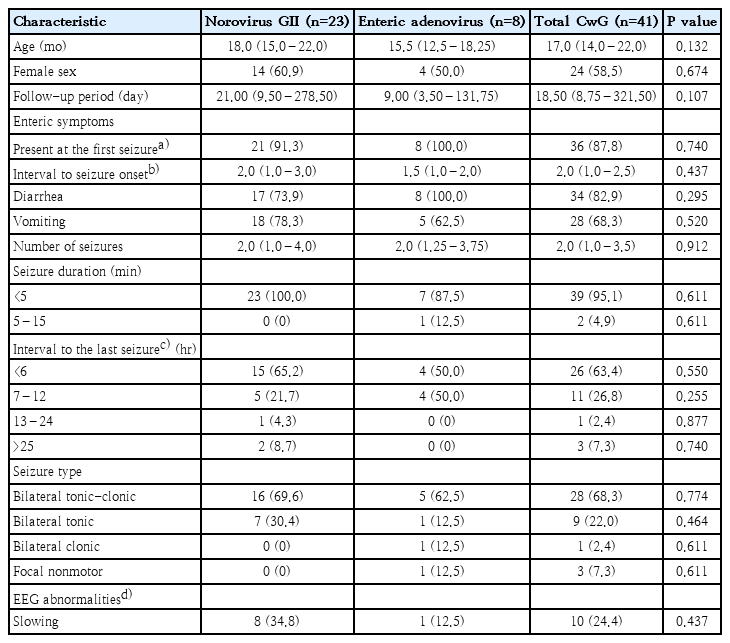
4. Norovirus GII-associated CwG versus enteric adenovirus-associated CwG
The median ages of the patients with norovirus GII (N=23) and enteric adenovirus (N=8) were 18.0 months (IQR, 15.0–22.0 months) and 15.5 months (IQR, 12.5–18.25 months). Of the patients with norovirus GII, 60.9% were female, whereas females made up 50% of the patients with enteric adenovirus. Interestingly, enteric adenovirus-associated CwG was not detected in the spring. In all patients with enteric adenovirus, enteric symptoms were present at seizure onset. The median interval between enteric symptom onset and seizure onset was 2 days (IQR, 1.0–3.0 days) in those with norovirus GII and 1.5 days (IQR, 1.0–2.0 days) in those with enteric adenovirus. All patients with enteric adenovirus-associated CwG had diarrhea (Table 3).
Clustered seizures were observed in 69.6% and 75% of the patients with norovirus GII and enteric adenovirus, respectively, and the median number of seizures was 2.0 in both groups. The duration of each episode was <5 minutes in all patients, except the one with enteric adenovirus. The intervals between the first and last seizure were within 12 hours in all patients with enteric adenovirus. Bilateral tonic-clonic seizures were present in 69.6% of the patients with norovirus GII and 62.5% of those with enteric adenovirus. Focal epileptiform discharges were not observed in the patients. EEG slowing was observed in 34.8% and 12.5% of the patients with norovirus GII and enteric adenovirus, respectively (Table 3).
Uric acid levels were elevated in both groups. Most laboratory profiles did not differ significantly between the enteric adenovirus- and the norovirus GII-associated CwG groups, although blood lactate levels were slightly higher in the enteric adenovirus group (P=0.030) (Supplementary Table 3).
Discussion
In this study, we hypothesized that in South Korea, during the COVID-19 pandemic, the incidence of CwG would change with the markedly lower incidence of viral enteritis at the start of the pandemic [14,15]. However, our analysis shows that the frequency of CwG did not change significantly in our clinic during the pandemic. In the 3 years before COVID-19, there were 18 patients with CwG, whereas 23 patients developed CwG during the 3-year pandemic. There may be several reasons why CwG frequency did not fall during the COVID-19 pandemic. First, personal hygiene may have only marginally improved in children aged less than 3 years, a group prone to CwG. Indeed, frequent hand washing and strict social or personal distancing might not have been possible in this age group. Therefore, the rate of enteric viral transmission via the fecal-oral route, and the need for intimate contact may not have reduced significantly in children aged less than 3 years when compared with older children. Second, there was a gradual increase in viral gastroenteritis after 2021. Although no relevant South Korean studies were published in the pandemic period, based on KDCA’s publicly available national data on viral gastroenteritis surveillance using the clinical reports and direct stool samples, the incidence of viral gastroenteritis and the number of acute gastroenteritis stool samples increased gradually after 2021 [17].
The seasonal CwG variation observed in our study was not apparent during the COVID-19 pandemic. The loss of seasonal variation during the COVID-19 pandemic was statistically significant in those with norovirus GII-associated CwG. Norovirus GII was the most common pathogen in the patients with CwG and was detected in more than half of the CwG cases reported in this study. Although in the period before the COVID-19 pandemic, norovirus GII-associated CwG was detected only in winter and spring, during the pandemic they were detected in all seasons and were significantly higher in summer. Based on KDCA’s publicly available viral gastroenteritis surveillance data, the number of virus-positive samples during the COVID-19 pandemic increased significantly during summer but decreased in spring and autumn [17].
A notable change in the types of CwG-associated viruses during the COVID-19 pandemic is indicated by the increase in the number of enteric adenovirus-associated CwG cases, with enteric adenovirus being isolated in only one patient before the pandemic and in 7 patients during the pandemic. Although the small sample size of enteric adenoviral CwG cases did not reach statistical significance, enteric adenoviruses were predominantly isolated in 2021. Indeed, KDCA’s viral gastroenteritis surveillance data also show that the positivity rate for enteric adenoviruses increased from 2021, although norovirus is the most common cause of viral gastroenteritis, accounting for more than half of the cases [17]. However, the positivity rate of group A rotaviruses decreased from 2020 [17].
Despite the increase in the incidence of enteric adenoviral infections during the COVID-19 pandemic, no studies have described the clinical characteristics of enteric adenovirus-associated CwG. In this study, the median age of the 8 patients with enteric adenovirus-associated CwG was 15.5 months (IQR, 12.5–18.25 months). There was no notable sexual distribution in the patients with enteric adenovirus-associated CwG. Enteric adenovirus-associated CwG was not observed during spring. Instead, its cases began being detected after summer and peaked during winter. Diarrhea was present in all subjects with enteric adenovirus-associated CwG. The median duration between enteric symptom onset and seizure onset was 1.5 days (IQR, 1.0–2.0 days). Clustered seizures affected 75% of the patients, with all seizures ceasing within 12 hours. Most seizures (62.5%) were bilateral tonic-clonic. The clinical characteristics of the subjects with enteric adenovirus-associated CwG with did not differ from those of the patients with norovirus GII-associated CwG, although clinical data based on large sample sizes are needed to validate these observations. Serum uric acid levels in the patients with enteric adenovirus-associated CwG were as high as in rota- or norovirus-associated CwG patients [12,19]. Blood lactate levels in the subjects with enteric adenovirus-associated CwG were slightly higher than in the patients with norovirus GII-associated CwG.
Human adenoviruses are a group of 7 species (A to G), with 104 serotypes [20]. Adenoviruses are common in children aged less than 5 years [20]. These nonenveloped, double-stranded DNA viruses cause various diseases [20], including respiratory tract infections, which are most common, and gastroenteritis, which is also common, especially in children [20-22]. Adenovirus 40 and 41 (species F) are important causes of pediatric acute gastroenteritis [20,22,23]. Although a seasonal prevalence of adenoviral gastroenteritis has not been established, data from some countries indicate that their incidence peaks in the summer and autumn [21,23]. Adenovirus-associated inflammatory central nervous system diseases are rare and they mostly affect immunocompromised individuals [20,24,25]. Meningitis, meningoencephalitis, and acute necrotizing encephalopathy have been associated with adenovirus 3 or 7 (species B) [20,24-27].
This study has several strengths. First, it is the first to analyze changes in the frequency, seasonal variation, and viral causes of CwG during the COVID-19 pandemic. Second, it is the first to describe the clinical characteristics of enteric adenovirus-associated CwG. However, this study’s retrospective single-center design and small CwG sample size may limit its generalizability, and larger prospective studies are needed to validate our findings.
In conclusion, the frequency of CwG in our center did not change significantly during the COVID-19 pandemic, although the total number of patients with ‘other and unspecified convulsions’ decreased. The seasonal predilection of CwG during the winter and spring was not apparent during COVID-19. Norovirus GII-associated CwG occurred over 4 seasons during the COVID-19 pandemic, with a significant increase during summer. Enteric adenovirus-associated CwG increased during the COVID-19 pandemic. Their clinical and laboratory characteristics were not very different from those with norovirus GII-associated CwG, although further studies of additional patients are warranted.
Supplementary materials
Supplementary Tables 1-3 and Fig. 1 can be found via https://doi.org/10.3345/cep.2023.01137.
Viruses detected via gastroenteritis surveillance
Seasonal frequency of viral pathogens based on Publicly available data from the Korea Disease Control and Prevention Agency [17]
Laboratory characteristics of norovirus GII-associated CwG versus enteric adenovirus-associated CwG
Annual distribution of patients with benign convulsions with gastroenteritis. GII, genogroup II.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contribution
Conceptualization: KYO; Data curation: NH, LS, KSH, KYO; Formal analysis: NH, LS, KSH, KYO; Methodology: KYO, NH; Project administration: KYO; Visualization: NH, KYO; Writing original draft: NH, KYO; Writing - review & editing: KYO.
Acknowledgements
We gratefully acknowledge the staff who care for children with seizures in the pediatric department of Chonnam National University Children’s Hospital, Gwangju, Korea. We also thank the medical records department’s staff for providing data on inpatient visits and the secretary, Mi Jin Lee, for managing the data.