Utility of eosinophil granule proteins in management of pediatric chronic cough
Article information
Key message
· Pediatric chronic cough often involves eosinophilic inflammation; however, objective measurements are not routinely used in treatment decisions.
· Accurate biomarkers of eosinophil activity, such as eosinophil-derived neurotoxin (EDN) and cationic proteins (ECP), should be used. EDN, which overcomes the shortcomings of ECP, recently received approval for use in Korean healthcare settings.
· EDN and ECP can play a role in treatment period and drug selection decisions.
Cough is among the most common symptoms of pediatric respiratory diseases. Chronic cough is usually defined as coughing for >8 weeks in adults and adolescents >14 years of age [1]; however, many define a shorter time period of >4 weeks in children and adolescents ≤14 years [2-4]. Determining the etiology of chronic cough is important as it may signal a potentially serious medical condition; however, in some cases, it remains unknown.
Airway inflammation may be a feature of chronic cough, and airway eosinophilia may occur without asthma [5]. Cough-variant asthma, among the most common causes of chronic cough in some populations, can account for 33%–41% of cases in adults [6,7]. Various specimens from patients with different cough phenotypes contained inflammatory cells such as eosinophils, neutrophils, and mast cells that were implicated in the pathogenesis [8]. The neurokinins interleukins (IL)-4 and -5, substance P, and calcitonin gene-related peptide stimulate effector molecules such as major basic protein (MBP), cysteinyl leukotrienes, and eosinophil cationic protein (ECP) that are released from eosinophils, which in turn stimulate cough sensory and muscarinic nerves [8]. Notably, IL-4 and -5 are T helper 2 cytokines that play key roles in allergic inflammation [5]. The role of allergic airway inflammation in chronic cough is highlighted by the fact that nerve growth factor, which is mainly derived from eosinophils, increases the expression of neuronal receptor transient receptor potential channels on inflamed sensory nerves [8].
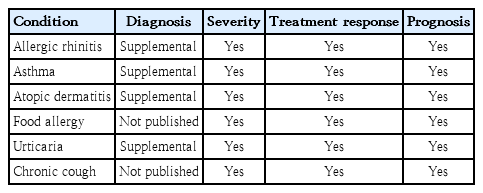
Activated eosinophils, the major effector cells of allergies, release 4 highly basic granule proteins: MBP, ECP, eosinophil peroxidase, and eosinophil-derived neurotoxin (EDN). The direct measurement of one or more of these eosinophil granule proteins reportedly reflects the eosinophilic inflammatory response [5,9-11]. In a letter to the editor recently published in Clinical and Experimental Pediatrics, Kim et al. [2] reported that serum ECP levels were significantly increased and highly correlated with blood eosinophil counts and fractional exhaled nitric oxide levels. They also found that serum ECP levels were elevated in more than half of patients with neither atopic sensitization nor eosinophilia. These findings are interesting. In the past, as Kim et al. [2] mentioned, ECP has been the most widely studied. However, times have changed, and through multiple studies by many independent research groups, the usefulness of EDN in the diagnosis, treatment, and monitoring of several diseases has been demonstrated [9] (Table 1). EDN can be collected from a number of specimen types (e.g., blood, serum, induced sputum, nasal swab, urine, and feces), as can ECP, but EDN is superior to ECP in test reproducibility because: (1) it is more easily recovered from measuring instruments and cell surfaces due to its weaker electrical charge; and (2) it is released from eosinophils at greater efficiency than ECP, further increasing its recoverability. Unlike ECP, EDN has activity against respiratory infections that are strongly associated with allergic disease development (e.g., respiratory syncytial virus and human rhinovirus) [9].
Few studies have examined eosinophilic inflammation in chronic cough are few, particularly in pediatric populations. Kim et al. [2] recently reported significantly increased ECP levels in 62% and 63% of pediatric age groups (i.e., 6–13 and <6 years of age), respectively. Among patients without atopic sensitization or eosinophilia, 51% and 56% exhibited high ECP levels, respectively. The authors concluded that evaluating serum ECP levels may aid treatment decisions in cases of pediatric chronic cough. To date EDN in chronic cough has been studied only in adults [5]. This study, of EDN (and MBP) as biomarkers of eosinophilic degranulation showed that sputum EDN levels in the group with chronic cough and asthma were significantly higher than those in patients with chronic cough but no asthma as well as normal controls. EDN levels in the nonasthma group were higher than those in normal controls, butthe difference was not statistically significant. Because of its overall superior performance of EDN as a biomarker (versus ECP), future studies in pediatric chronic cough are warranted.
The diagnosis, treatment, and monitoring of allergic diseases are especially difficult in children. Airflow limitation does not immediately elicit symptoms or warrant rescue medication use, and parents often do not recognize decreased lung function. Younger children (<6 years of age) cannot adequately participate in lung function and other physiological tests [9]. Therefore, objective measurements of respiratory impairment are needed for this age group as well as older children, a sentiment echoed in the recent study of Kim et al. [2] of eosinophil granule protein levels in chronic cough as well as other studies [3,9-12].
Direct measurements of eosinophilic granule proteins like EDN and ECP have proven useful in the diagnosis, treatment, and monitoring of allergic diseases; therefore, their use in childhood chronic cough should be further explored.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.