Efficacy of social skills group intervention among children with mild autism spectrum disorder
Article information
To the editor,
Autism spectrum disorder (ASD)is a neurodevelopmental disorder diagnosed based on Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria. This includes having persistent deficits in social communication and interaction, plus restricted repetitive behaviors (RRB) [1]. Severity of ASD is classified into level 1 (requiring support), level 2 (requiring substantial support) and level 3 (requiring very substantial support). Individuals with ASD face social interaction difficulties which vary over the spectrum and with time, but persist as a significant challenge [2,3]. Interventions targeting social interaction have shown varying degrees of effectiveness with limitation in generalizability among children with ASD [4].
The child development clinic team of Hospital Sultan Ismail Johor Bahru has been conducting an annual social skills group (SSG) workshop for children with mild ASD (level 1 severity) since 2018. The SSG workshop is a 10-day program developed based on Social Thinking (ST®) “We Thinkers!” series. ST® is a cognitive-based methodology which focuses on developing social competencies such as social perspective taking, self-awareness, executive functioning and social problem solving. Children are enrolled from their routine outpatient visits if they are between 4 and 11 years old with clinical diagnosis of mild ASD based on DSM-5 criteria, have cognitive or developmental quotient ≥70, and have fluent speech in either English, Malay, or Chinese. Children with impaired hearing, genetic disorders, severe medical conditions, or receiving concurrent >20 hours per week of other intensive interventions, are not eligible.
Part 1 (first 5 sessions) and part 2 (last 5 sessions) of the SSG workshop are held during 2 different school holiday periods. On each day of the workshop, parents and children attend a 2-hour session. Each session consists of opening routine, storytelling, teaching session, structured group activity (among children only), and closing routine (includes debriefing for parents). A 2-hour debriefing session is conducted 4 weeks after the end of each part to recap the program and highlight activities to be carried out at home. This study aimed to evaluate the effectiveness of the 2022 SSG workshop.
A single arm, pre- and postinterventional study was conducted on children with mild ASD who attended the full 2022 SSG workshop. All children attending the 2022 SSG program were included in the study. Subjects were excluded if they missed ≥1 day of the SSG workshop or did not complete all the assessments. Written informed consent was taken from all parents prior to the study.
Outcomes were measured using the Social Responsiveness Scale, second edition (SRS-2) and the parenting sense of competence (PSOC). The SRS-2 is a 65-item assessment that consists of 5 subscales: social awareness, social cognition, social communication, social motivation, and RRB [5]. Higher scores indicate higher social impairment associated with ASD. The PSOC is a 17-item scale measuring parental satisfaction and efficacy [6]. Higher scores indicate a higher sense of parental competence. The preassessment was conducted in May 2022 before the workshop. The first postintervention measure was conducted in January 2023 and repeated in May 2023 to evaluate the longer-term effect. Nonverbal intelligence quotient (NVIQ) score was assessed using the Kaufman Brief Intelligence Test Second Edition for children above 6 years old [7].
All data were analyzed using IBM SPSS Statistics ver. 28.0 (IBM Co., Armonk, NY, USA). Results were presented as frequencies and percentages for categorical variables and as median (range) for continuous variables. The Wilcoxon ranked sum test was performed for analysis of nonparametric data. Spearman correlation was performed to explore correlation between NVIQ score and improvements in outcome. A value of P<0.05 was considered statistically significant.
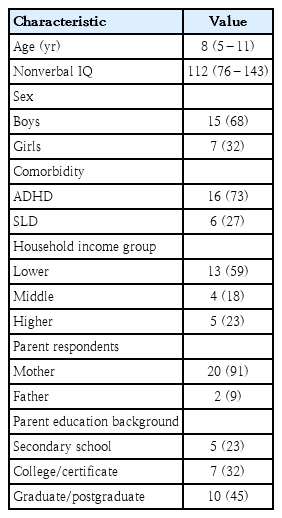
Thirty children enrolled for the 2022 SSG workshop. After excluding 8 subjects (4 missed ≥1 day, 4 incomplete assessments), 22 patients were included into the study. Table 1 shows the demographics of the children and their parents.
Total SRS-2 T-scores reduced immediately post workshop (P=0.028) and persisted 5 months post intervention though statistically not significant (Table 2). SRS-2 subscales showed significant improvement in RRB and social communication both immediately (P<0.001 and P=0.010 respectively) and 5 months after the SSG (P=0.008 and P=0.015 respectively). PSOC scores improved post workshop (P=0.020) and sustained even 5 months after the workshop (P=0.024). There were no significant correlations between the improvements and NVIQ scores.
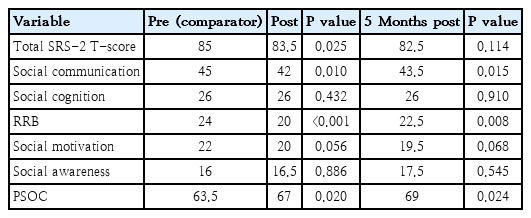
SRS-2 and PSOC scores preworkshop, immediately postworkshop, and 5 months postworkshop for 2022 Social Skills Group Program participants
This study showed that children who participated in the SSG had improvement in SRS-2 scores, especially in communication and RRB. The KONTAKT trial in Sweden reported that adolescents receiving SSG training had significantly larger change in SRS-2 scores compared to standard care during posttreatment(-8.3, P=0.012) and during follow-up (-8.6, P=0.015) [8]. In India, SSG therapy was able to reduce SRS-2 scores after 10 sessions (83.5 to 80.1, P<0.001) and 3 months post therapy (76.9, P<0.001) [9]. All SRS-2 subscale scores showed improvement. Another parent-mediated social skills intervention program for young children with ASD showed significant improvements in SRS-2 scores posttreatment (75.45–66.86, P<0.001) and on follow-up (68.34, P<0.01) [10].
This SSG workshop placed emphasis on receptive and expressive social communication skills such as eye contact, body language, and bidirectional social communication, which improved communication scores. The improvement in RRB may result from lessons targeting dynamic appraisal and flexible creative thinking. Besides, improvement in social communication and interaction could also increase their engagement with others therefore allowing them to develop a wider scope of interest. The workshop provided parents with skills to guide their children with ASD, leading to higher competency and less distress, thus improving PSOC scores.
Limitations of this study include that there was no control group (children with ASD who did not attend the SSG workshop). The participants were self-recruited due to the high commitment required. It is recommended for future research to be conducted with higher quality designs and larger sample sizes. Effects of confounding factors such as co-morbidities should be investigated.
In conclusion,the workshop introducing the SSG program potentially increased parental competence and improved ASD symptoms in terms of RRB and social communication. Some of the effects persisted 5 months after the workshop.
Notes
Ethical statement
This study was approved by the Medical Research and Ethics Committee of the Ministry of Health Malaysia with the NMRR ID-21-02198-B7K.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgements
We would like to thank the Director General of Health Malaysia for permission to publish this study. We would also like to thank Dr Lim Chooi Ling from IMU University for assistance with the statistics.