Role of proper postnatal care in continued exclusive breastfeeding among young Indonesian mothers
Article information
Abstract
Background
Exclusive breastfeeding (EBF) provides numerous health benefits to children. However, the EBF rate is unsatisfactory among young mothers because they often experience difficulties. Thus, interventions during the postnatal period are imperative to encouraging EBF practices in these populations. Postnatal care (PNC) should be delivered appropriately to ensure a positive postnatal experience; however, there has been little discussion of evidence therein to date.
Purpose
This study investigated the association between proper PNC and EBF practices among young Indonesian mothers.
Methods
This cross-sectional study analyzed data from the 2017 Indonesia Demographic Health Survey. All mothers aged 15–24 years who delivered an infant within the 2 years preceding the survey were included. Mothers were considered to be receiving proper PNC if they started breastfeeding soon after delivery, attended a PNC appointment within 2 days after giving birth, and received breastfeeding counseling and observation during the PNC visit.
Results
Approximately 51.6% of infants under 6 months of age born to young mothers (those aged 15–24 years) were exclusively breastfed. Appropriate PNC was received by approximately 24.3% of the total population. The correlation between proper PNC and EBF practices was significant among adolescent mothers aged 15–19 years after an age stratification analysis (odds ratio, 8.22; 95% confidence interval, 1.957–34.524). Maternal age became a noticeable confounder after a risk-stratification analysis.
Conclusion
Our findings imply the importance of breastfeeding service delivery during the early postnatal period in continuing EBF. Ensuring high PNC quality helps ensure positive postnatal experiences, particularly for adolescent mothers.
Key message
Question: Is proper postnatal care (PNC) associated with exclusive breastfeeding (EBF) practice among young Indonesian mothers?
Finding: Proper PNC elevates the likelihood of EBF among Indonesian adolescent mothers aged 15–19 years.
Meaning: Breastfeeding services should be provided during the early postnatal period to support EBF practice among adolescent mothers. High-quality PNC is a tailored intervention for vulnerable populations.
Introduction
Exclusive breastfeeding (EBF) is very important for a child's early life because it can protect around 800,000 children under 5 from the risk of death and various diseases [1]. Breastmilk has active capabilities that can be adapted optimally to the baby's needs, and it is the only nutrition within the first six months of life [2]. EBF practice can serve as a major component during the older period, such as improving cognitive function and intelligence, preventing obesity, and reducing the risk of cardiovascular and metabolic diseases [3,4]. However, the rate of EBF practice in the world is only around 44%, with less than one in two children exclusively breastfed [5].
The low practice of EBF is more severe among young mothers compared to older mothers. In India, EBF coverage among young teenage mothers is only 58.7% [6], while in Bangladesh, it is only 53% [7]. In Indonesia, the proportion of EBF among adolescent mothers aged 15–19 years is only 50.9%, while in the older age group, it is relatively higher, namely 53.9% [8]. This evidence implies that even though abundant measures have been taken to promote EBF practice, it is not adequate to be sensitive towards specific groups, such as young mothers. Therefore, any EBF program must be sensitive to vulnerable groups. Adolescent-oriented intervention could be expected to raise their knowledge, attitude, and practice of EBF [9].
As a part of motherhood experience, EBF is quite challenging for all mothers, and the challenges are more burdensome for younger ones. Aside from facing various lactation problems, young mothers often receive social stigma against breastfeeding in public [10,11]. One intervention to promote EBF is encouraging postnatal care (PNC), which includes counseling about breastfeeding and understanding breastfeeding problems [12]. A shred of evidence suggests that visiting PNC within two days after delivery has benefits in reducing non-EBF compared to no visits at all [13]. However, limited evidence identified the service quality regarding EBF practice during the PNC visit.
This study explored the relationship between proper PNC and EBF practice among young Indonesian mothers. The assumption is that proper PNC will link to a greater chance of EBF practice among young mothers in Indonesia. Aside from generating further evidence about the motherhood experiences among young mothers, our study has the potential to explore the gap in breastfeeding interventions that have been implanted till today, which might not target the vulnerable population. The present study's findings could be recommendations for policymakers and other stakeholders to improve the programs based on scientific evidence and precise data.
Methods
1. Study design
An observational cross-sectional study was carried out in this study to present the quantitative variables. The present study used secondary data from the Indonesian Demographic Health Survey (IDHS) 2017. The nationally representative survey thoroughly depicts Indonesia's population, family planning, reproductive health, and maternal and child health conditions. The National Population and Family Planning Board, the Board of Statistics, and the Ministry of Health (Kemenkes) of Indonesia together conducted the 2017 IDHS. The Indonesian government funded the survey's local expenditures. The Inter City Fund International offered technical support through the Demographic and Health Surveys Programme, sponsored by the United States Agency for International Development. More information about the survey methodology and sampling procedure is provided elsewhere [14].
Any information from the mothers was collected since they were the survey respondents. Every infant born to a woman aged 15–24 included in the survey was eligible for analysis. The analysis was limited to these inclusion criteria: (1) The infant was born within 24 months preceding the survey. (2) The infant was alive and living with her mother. (3) The infant was the last-born child, aged less than six months.
Any respondent who did not meet the inclusion criteria was excluded. Since the proportion of missing data was only 3.8%, all missing data were dropped. 437 observations were retrieved in this phase. To account for multistage randomized cluster sampling method in the survey, weighted analysis was performed in all stages of analysis. The weight variable was generated by dividing the individual's sample weight by one million. Thus, 415 respondents were included in the final analysis, with an average response rate of 98%.
2. Variables
Our primary outcome was EBF practice, defined as the proportion of infants under six months who received no other foods or liquids, including water, except for oral rehydration solution, prescribed vitamins, or medicines. It was composed of recall information 24 hours before the survey, derived from IDHS individual women’s questionnaires. The respondent, the infant’s mother, was asked whether she still breastfed their children and did not give them any food or liquid 24 hours before the survey. The outcome was categorized into a binary form: (1) EBF, if the last-born infant lived with her mother fully breastfed without any additional food, coded as one; (2) non-EBF, if the last-born infant was not breastfed or breastfed with additional food or other liquid, such as formula milk, coded as zero.
The primary independent variable was proper PNC. We constructed proper PNC as a qualified newborn health service complemented with breastfeeding care within 2 days after delivery. Proper PNC (coded as one) was determined if a mother carried out a series of actions below:
· Early initiation of breastfeeding, defined as a newborn who started breastfeeding within one hour after birth [8].
· Early PNC, defined as a mother and her last child visiting care within two days after delivery [15]. This service is crucial since it is the first contact between mother and infant with the health provider after being discharged from hospital.
· Breastfeeding counseling is defined as support for the mother and her infant provided by healthcare within 2 days after delivery [16].
· Breastfeeding observation is the identification of proper breastfeeding methods within the first 2 days after delivery.
Any respondent who did not complete all the above indicators was coded as zero and considered as conducting improper PNC.
Sociodemographic characteristics such as the mother’s age within the 5-year group, mother’s education level, marital and working status, as well as household wealth index, number of living children, type of residence, regions, media exposure, and decision maker for child healthcare for children, were measured as covariates. Principal component analysis (PCA) was used to build the household wealth index based on household ownership of a few specified assets, such as a toilet type, an energy source, and a drinking water source [17]. Birth history variables, such as place of delivery and history of caesarean section, were explored to identify features under the mother-infant dyad. Every variable listed earlier was considered a potential confounder of the analysis.
3. Statistical analysis
Three steps of statistical analysis were performed to answer the study's objective. First, descriptive analysis was used to determine the distribution of respondents' characteristics, which were presented in frequency (N) and proportion (%). Since we used nationally representative survey data, a weighted analysis was executed. The weight variable was generated by dividing each individual's sample weight by 1 million.
The following analysis was bivariate logistic regression to estimate crude odds ratio (OR) as the effect size of predictor and outcome correlation. Any relationship which possessed a probability value (P value) less than 0.05 (P<0.05) was considered statistically significant. We also measured any influenced variable (P<0.25) to be included in the multiple logistic regression for multivariate analysis.
Multiple logistic regression to determine adjusted OR (aOR) was conducted to control multiple influences concurrently. For a deeper understanding of the population, we carried out a risk-stratification analysis. The stratification was utilized to identify the effect modification within the relationship between predictors and outcomes and enhanced precision and accuracy. Moreover, understanding the variation across different levels could improve the targeted interventions to tailor specific groups. In this present study, age in the 5-year group was utilized for the stratification analysis. All analyses were performed using the StataMP 17.0 (StataCorp LLC, College Station, TX, USA).
4. Ethical consideration
Our study was approved by the Medical and Health Research Ethics Committee, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada on February 15th, 2024, with reference number KE/FK/0242/EC/2024.
Results
1. Respondent’s characteristics
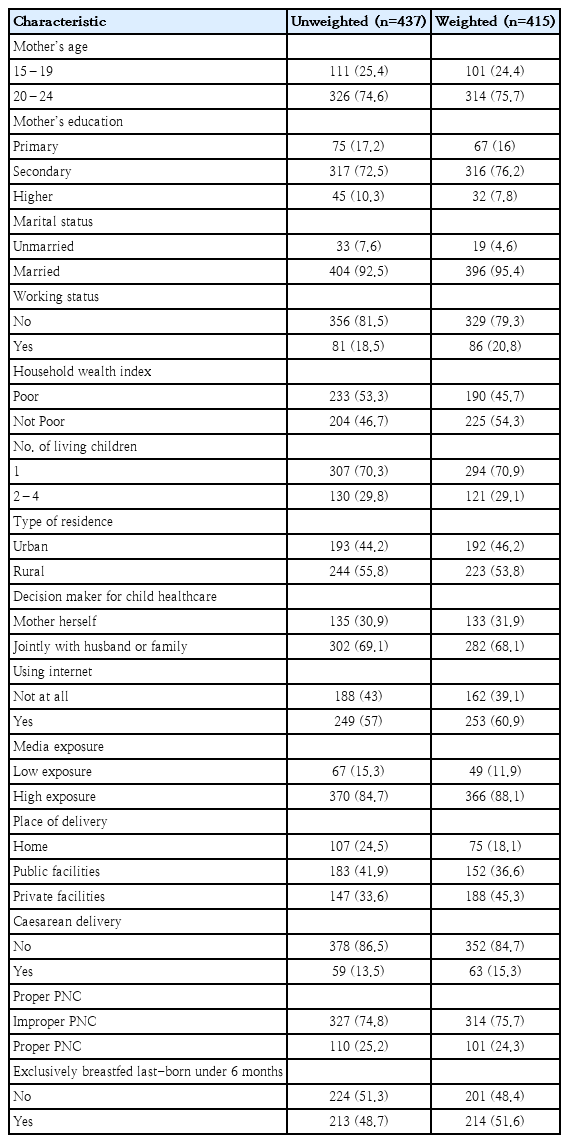
Approximately 75.7% of total respondents were young adult mothers, aged 20 to 24, while the rest were adolescent mothers, aged 15 to 19. Most respondents went to secondary high school (76.2%) and married (95.4%), while only around 20.8% of them were employed. The respondent’s infant was typically singleton birth, namely 70.9%. The vast majority of respondents lived in rural areas (53.8%) and had good exposure towards the internet (60.9%) and other media (88.1%).
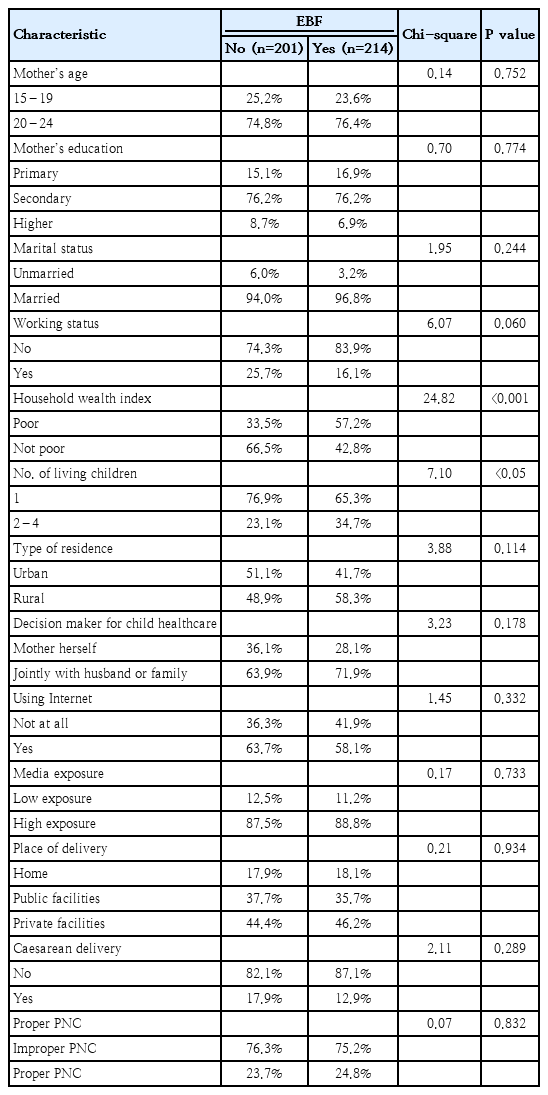
The decision for child healthcare was primarily made by the mother and her spouse or family member (68.1%). Private facilities were the prominent delivery location (45.3%), followed by the public’s (36.6%) whereas the majority of respondents delivered their infant vaginally (84.7%). Slightly fewer than a-quarter of these young mothers received proper services during PNC visit within 2 days after delivery. Furthermore, the proportion of exclusively breastfed infants aged less than 6 months was approximately 51.6%, and its distribution did not display a noteworthy difference according to the sociodemographic characteristics except for wealth index (P<0.05) and number of living children (P<0.05) (Tables 1 and 2).
2. Correlation between predictors and EBF
Logistic regression analysis was performed to determine the effect size presented in Table 3. For bivariate analysis that used simple logistic regression, working status, wealth index, and number of living children were significant predictors of EBF practice. The multivariate analysis was conducted to control any covariates that demonstrated a level of significant association (P value) of less than 0.25. Marital status, working status, wealth index, number of living children, type of residence, decision maker for child healthcare, using the internet, and caesarean delivery were included in multivariate model to adjust our main independent variable, proper PNC. The findings demonstrated some differences from the bivariate analysis. The number of living children was no longer a noteworthy predictor of EBF practice (P>0.05) while working status and wealth index remained significant. Interestingly, marital status became a remarkable predictor after considering the external variables.
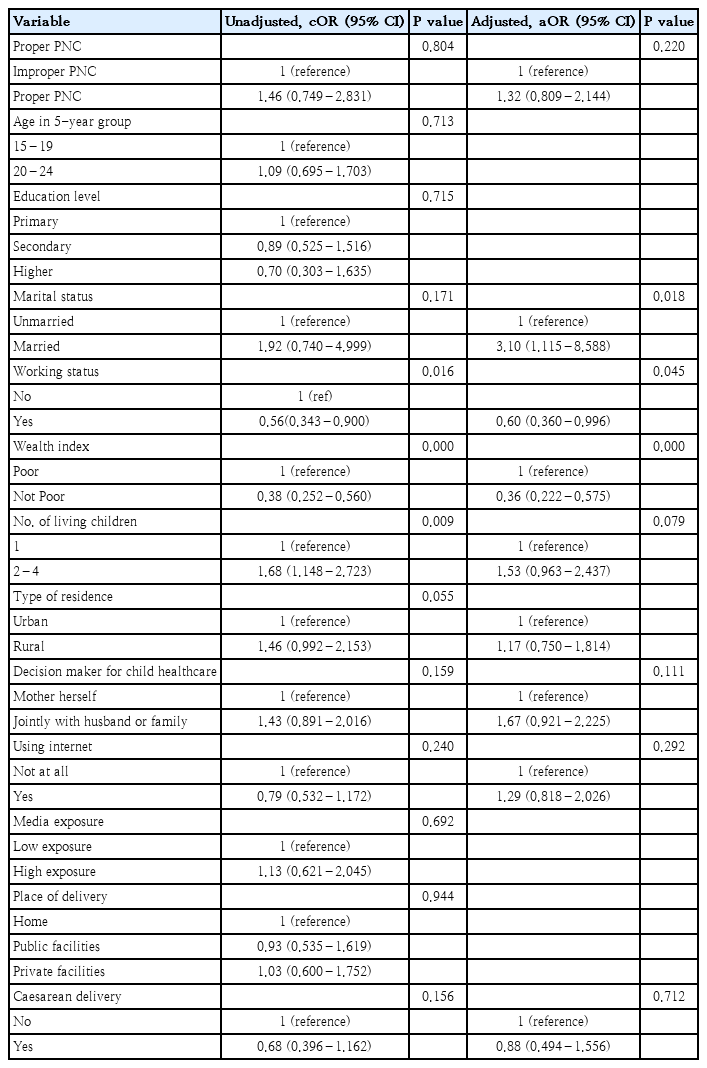
Logistic regression modeling of exclusive breastfeeding practice among young Indonesian mothers (weighted) (EBF vs. non-EBF)
Employed mothers showed a lesser chance to breastfeed their infant exclusively compared to unemployed ones (aOR, 0.60; 95% CI, 0.360–0.996), whereas married mothers were vice versa (aOR, 3.095; 95% CI, 1.115–8.58). Furthermore, infants from poor families had a nearly 70% lower probability of receiving EBF (aOR, 0.36; 95% CI, 0.222–0.575) compared to those who are from wealthier families. Unfortunately, we did not find an important correlation between proper PNC and EBF practice in this stage of analysis. Thus, the analysis was stepped up to risk-stratification analysis for further exploration.
3. Age stratification analysis
A stratification analysis was carried out to identify and further understand the relationship between proper PNC and EBF practice pursuant to certain covariates. We decided to stratify the analysis according to age in the 5-year group and found a distinctive correlation between proper PNC with EBF practice after performing this test. The results are demonstrated in Table 4.
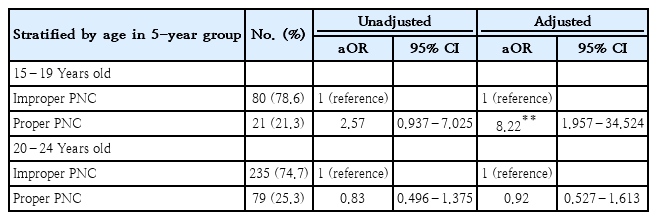
Age stratification analysis of correlation between proper PNC and EBF continuation among adolescent and young mothers, 2017 IDHS (EBF vs. non-EBF)
A mere 21% of adolescent mothers who were between the ages of 15 and 19 experienced a PNC within 2 days of giving birth, completed early initiation of breastfeeding, and received breastfeeding observation and counseling. In contrast, the share of older mothers was higher, coming in at 25%. In the multivariate model, infants born to adolescent mothers who visited proper PNC had approximately eight times higher likelihood of EBF compared to mothers who improperly attended PNC (aOR, 8.22; 95% CI, 1.957–34.524). The correlation did not occur among young mothers who aged 20 to 24 (Table 4).
Discussion
This study has proven around 51.6% of infants born to young mothers were exclusively breastfed. According to sample characteristics, the distribution of EBF practice only differed significantly (P<0.05) by wealth index and number of living children. The present study demonstrates that some factors linked to EBF practice among young mothers were marital status, working status, and wealth index. The primary independent variable, proper PNC was not significantly associated with EBF practice in all age groups; instead, it became noteworthy factors for infants delivered by adolescent mothers aged 15 to 19.
Being married could raise the probability of an infant being breastfed exclusively up to threefold higher among young mothers. Parallel with a previous study conducted in Ethiopia [18], the supportive environment from a spouse or another family member may encourage the mother to breastfeed her baby devotedly [19]. In contrast, unmarried young mothers are underprivileged in this context. The reason is probably caused by facing problems accessing adequate health services, as they often deal with negative stigma [20] and perceived judgement of premarital sex [21]. These issues demonstrate the necessity to put more effort and tailored intervention among young unmarried mothers, who are often neglected. Moreover, family involvement becomes an essential consideration when proposing adolescent-oriented interventions.
As explained in our study and the previous one [22], an infant whose young mother is employed possesses a negative association with EBF practice [17]. Furthermore, in Indonesia, less than 25% of working mothers utilize the lactation service, and only one-tenth of them can obtain its benefits [23]. Although breastfeeding promotions and campaigns have been implemented in the working environment [24], our findings indicate the uptake of lactation services is under the line, particularly among young mothers. Working mothers who experience difficulties in breastfeeding or expressing breastmilk in the workplace [17] choose to purchase formula milk to feed their infants because breastmilk substitutes such as infant formula are highly accessible and marketed largely across regions in Indonesia [25]. As an impact, we found wealthy young mothers can afford to buy breastmilk substitutes compared to poor ones, resulting in suboptimum breastfeeding practice.
In the present study, infants born to adolescent mothers aged 15–19 who properly received postnatal services had an approximately eightfold higher chance of obtaining breastmilk exclusively. It sheds light on the quality of PNC as a careful consideration since only attending PNC within two days after delivery cannot be measured as a qualified service [26]. A study suggests that increasing the likelihood of breastfeeding maintenance at six months of an infant’s life necessitates lactation services in PNC [27]. The present study demonstrates the importance of breastfeeding initiation after delivery, lactation counseling, and breastfeeding observation to emphasize EBF practice among infants born to adolescent mothers.
Postnatal education is an essential means of supporting breastfeeding behavior in adolescent mothers who still develop their capacity for comprehensive awareness. It allows them to immediately comprehend what to do while practicing with the infant directly [28]. A higher chance of EBF practice is observed among mothers who initiate breastfeeding soon after delivery [29] and counsel on breastfeeding during postnatal period [30]. However, the majority of adolescent mothers are reported to have trouble starting to breastfeed [31] and feel abandoned when healthcare providers just provide advice instead of giving them direct observation and guidance while breastfeeding [32]. Thus, providing a comprehensive postnatal service, which includes lactation management within 2 days after delivery, is imperative to ensure the qualified service received by mother-infant dyad, particularly among adolescents.
Our study highlights the encouragement of EBF practice by providing a positive postnatal experience towards adolescent mothers and their infants. To the extent of our knowledge, this is the first study identifying proper services acquired by adolescent mothers during early postnatal period in correlation with EBF practice. This study used IDHS 2017 data, which is nationally representative, so the results can be generalized to Indonesian population. However, there are some restrictions in interpreting the findings of the study. First, our study cannot provide a temporal causal-effect relationship since both predictors and outcomes were observed simultaneously. Thus, it only describes the effect size of association between predictors and outcome. Secondly, although data is derived from a population-based and nationwide survey, the retrieved final sample is only around one per cent of the total IDHS 2017 sample size. A small final sample size might influence confidence interval and level of significance values. Further research in prospective design can be beneficial to evaluate the adolescent mother's parenthood behavior, particularly since pregnancy. A deeper understanding of sociocultural context is also significant to determine the broader influence of family and society on infant feeding practices among vulnerable groups.
In conclusion, this study suggests that adolescent mothers in Indonesia need proper services during early postnatal period in maintaining EBF practice for their infants. Proper PNC should comprise lactation management services like early initiation of breastfeeding, lactation counseling, and breastfeeding observation in order to serve a high-quality service. Concerning the sociocultural aspects of vulnerable populations is advantageous in proposing adolescent-oriented intervention. Looking at the findings in this study, policymakers and stakeholders are in charge of putting more effort into breastfeeding promotion among younger mothers. Adolescent mothers who are already burdened experiencing their motherhood should be accompanied by equitable and qualified services to prevent adverse impacts on their infant’s health.
Notes
Conflicts of interest
The authors declare no conflict of interest related to this article
Funding
The study is supported by Indonesia Endowment Fund for Education (LPDP) of the Ministry of Finance of Indonesia.
Author contribution
Conceptualization: WT, AW, SP; Data curation: WT; Formal analysis: WT, AW, SP; Funding acquisition: WT; Methodology: WT, AW, SP; Project administration: WT; Visualization: WT; Writing-original draft: WT; Writing-review & editing: WT, AW