Diet-related behaviors affecting health and substance use among children and adolescents
Article information
Abstract
Unhealthy diet-related behaviors and poor diet quality during childhood and adolescence are the main factors contributing to noncommunicable diseases such as obesity, dyslipidemia, diabetes, hypertension, and cardiometabolic syndrome. Unhealthy diet-related behaviors can become lifelong habits associated with mental health problems, including depression, anxiety, attention deficit hyperactivity disorder, and substance abuse issues such as smoking, drinking, and other chemical compounds. Children and adolescents are in the developmental stages of brain structure, function, and neurotransmission systems, which can make them more susceptible to substance abuse (tobacco, alcohol, and drugs). Thus, mental health problems and substance use in children and adolescents may originate from unhealthy diet-related behaviors and poor diet quality. Here we reviewed the impact of diet-related behaviors and diet quality on children's and adolescents' physical and mental health and substance use by scrutinizing the 2021 Korean Youth Risk Behavior Survey (54,848 participants) and other relevant studies.
Key message
· Diet behaviors in children and adolescents are influenced by environmental and sociocultural factors.
· Unhealthy diet behaviors and poor diet quality are the main contributing factors to noncommunicable diseases and mental health problems during childhood and adolescence.
· Smoking and alcohol drinking in children and adolescents may be associated with unhealthy diet behavior or poor diet quality.
Graphical abstract. Association among unhealthy diet-related behaviors, poor diet quality, and physical and mental health problems and substance abuse. Unhealthy diet-related behaviors and poor diet quality during childhood and adolescence are the main factors contributing to noncommunicable diseases and mental health problems. The inflammatory response caused by unhealthy eating habits or poor diet quality is a suggested cause of physical and mental health problems. Childhood and adolescence are strongly influenced by the environment and sociocultural, emotional, and behavioral factors of dietary habits. This situation is significantly aggravated by substance abuse including smoking, drinking, and drugs.
Introduction
Childhood and adolescence are periods of rapid growth and development; therefore, an individual's health may be compromised if the large amounts of energy and nutrients required to fulfill their physiological requirements are not received. Healthy diet-related behaviors and good diet quality positively impact the physical functioning, mental health, emotional regulation, and academic performance of children and adolescents [1,2].
Children and adolescents are vulnerable to social influences in that their dietary habits are strongly influenced by sociocultural as well as emotional and behavioral factors [3,4]. Adolescence is often marked by a change in diet patterns, including skipping meals, frequent snacking, and consuming large amounts of unhealthy foods [5]. Diet culture is a global trend in which Westernized fast foods like hamburgers are common. The recent popularity of tanghuru, a traditional Chinese snack of several rock sugar-coated fruits, among children and adolescents in Korea is a typical case. In fact, unhealthy diet-related behaviors cultivated during childhood and adolescence can last a lifetime [6].
Diet-related problems can lead to obesity, increased cardiometabolic risk, impaired cognition, and poor academic performance [1,2], all of which are also linked to mental health problems [7,8]. In addition to poor diet quality and a lack of physical activity, substance abuse (i.e., smoking, drinking, and other drugs) further aggravates this circumstance [9].
Since 2012, the Korea Disease Control and Prevention Agency has conducted the Korean Youth Risk Behavior Survey (KYRBS) among middle and high schoolers. The KYRBS includes questions about diet-related behavior and diet quality, physical activity, smoking, drinking, and mental health [10]. We reviewed the literature on the impact of diet-related behavior and diet quality on the physical and mental health of and substance use among children and adolescents by examining data from the 2021 KYRBS (54,848 participants) and other relevant studies.
Unhealthy diet-related behavior and poor diet quality in children and adolescents
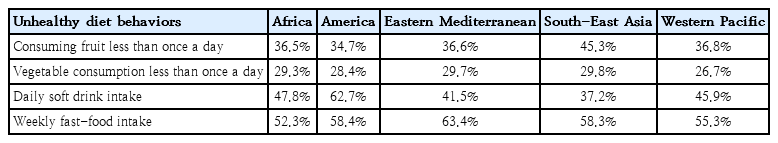
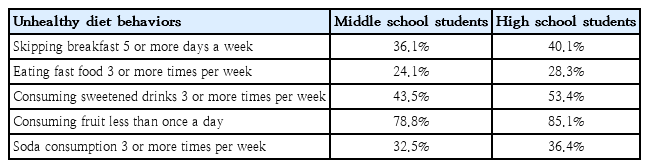
Diet-related behavior is characterized as an eating-related habit or pattern. A healthy or high-quality diet includes a higher intake of fruits, vegetables, fish, whole grains, and other foods that are beneficial to one's health [1]. Unhealthy diet-related behaviors include eating calorically dense foods with low nutrients, skipping meals (mainly breakfast), and using restrictive diets to lose weight, which can lead to nutrient deficiencies and health problems (Table 1) [4]. A poor diet quality refers to the consumption of insufficient amounts of fish, fruits, and vegetables and high amounts of fast food, processed foods, and soft drinks (sweetened beverages) [2].
Unhealthy diet-related behavior and poor diet quality are associated with a number of mental health concerns in children and adolescents [1]. Five key dietary recommendations for mental health have been established [5]: (1) following "traditional" dietary patterns, such as the Mediterranean, Norwegian, or Japanese diet; (2) increasing the consumption of fruits, vegetables, legumes, whole-grain cereals, nuts, and seeds; (3) consuming large amounts of foods rich in omega-3 polyunsaturated fatty acids; (4) replacing unhealthy foods with wholesome and nutritious foods; and (5) limiting the intake of processed foods, fast foods, commercial bakery goods, and sweets [5].
According to the Global School-Based Health Survey of the adolescents of 61 countries, 37% consumed fruits less than once a day, 28.5% consumed vegetables less than once a day, 50% consumed soft drinks daily, and 57.4% consumed fast food weekly (Table 1) [11]. However, the above study included the South-East Asian region of Bangladesh, Indonesia, Maldives, Nepal, Sri Lanka, and Thailand [11], and did not include data from Korea, Japan, or China. In a meta-analysis of the overall and regional pooled prevalence of psychological distress and unhealthy diet-related behaviors among 222,401 adolescents across countries and regions, the prevalence of psychological distress was 17.9%, and it was associated with inadequate fruit intake (pooled adjusted odds ratio [aOR], 1.19; 95% confidence interval [CI], 13.17–1.23), inadequate vegetable intake (pooled aOR, 1.19; 95% CI, 1.16–1.22), daily consumption of soft drinks (pooled aOR,1.14; 95% CI, 1.12–1.17), and weekly consumption of fast food (pooled aOR,1.12; 95% CI, 1.09–1.15). The authors suggested that adolescents experiencing psychological distress were more likely to have unhealthy dietary habits [11].
The 2021 KYRBS [10] assessed unhealthy diet-related behaviors, such as skipping breakfast 5 or more days a week, eating fast food 3 or more times a week, consuming sweetened drinks 3 or more times a week (Table 2). Of the students, 38.0% skipped breakfast 5 or more days a week (36.1% of middle schoolers, 40.1% of high schoolers); 26.2% ate fast food 3 or more times a week (24.1% were middle schoolers, 28.3% were high schoolers); and 48.3% consumed sweetened drinks 3 or more times a week (43.5% of middle schoolers, 53.4% of high schoolers). The high consumption rate of sweetened drinks among middle and high schoolers in Korea is similar to that of Australian children and adolescents, the highest consumers of ultra-processed foods such as confectionaries, savory snacks, fast food dishes, mass-produced packaged bread, frozen and readymade meals, juices, and soft drinks (53.1% and 54.1%, respectively) [12].
Obesity
Obesity is a global challenge against children’s health with increasing prevalence and morbidity [13]. The issues caused by a poor diet among the United States child population include obesity, dyslipidemia, insulin resistance, high blood pressure, pulmonary disorders, dental caries, and anemia [14]. The 2021 KYRBS [10] reported that the obesity rate was 13.5% of all students, 12.1% of middle schoolers, and 15.0% of high schoolers, with an increasing trend among the latter. The rates of overweight were 9.9%, 10.2%, and 9.6% for all, middle school, and high school students, respectively. The increasing trend of obesity and overweight among students might be related to unhealthy diet-related behaviors, including eating fast food 3 or more times a week and consuming sweetened drinks 3 or more times a week [4].
Diet quality and inflammatory responses
Diet quality plays a significant role in exacerbating or alleviating low-grade inflammation [15]. It is well-known that chronic sustained low-grade inflammation promotes the release of a multitude of inflammatory mediators and cytokines, predisposing the individual to insulin resistance, dyslipidemia, and other metabolic dysregulations [16]. Moreover, chronic low-grade inflammation contributes to the pathogenesis of mental health disorders (co- and multimorbid situations) of children and adolescents [15]. An unhealthy diet-related behavior or poor diet quality was associated with decreased health-related quality of life among children and adolescents [1]. Previous studies demonstrated that adolescents experiencing psychological distress tend to gravitate toward unhealthy or suboptimal dietary habits [17,18]. Nevertheless, such relationships can be complex to understand and potentially bidirectional [18].
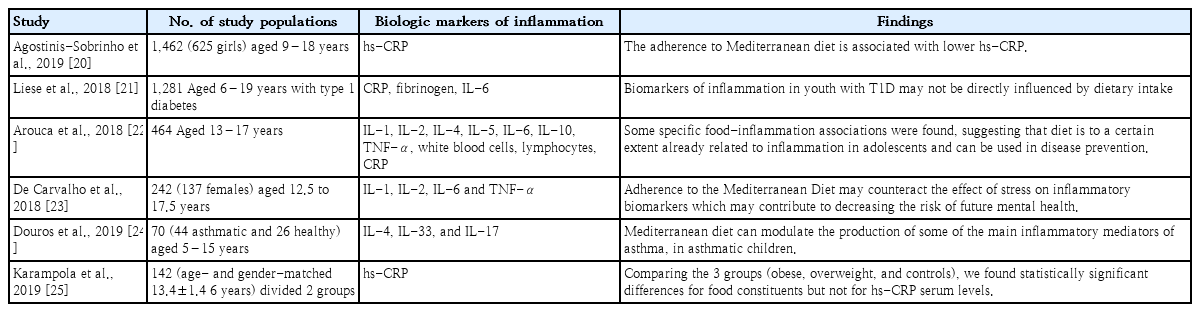
A systematic review of studies highlighted that inflammatory biomarkers are associated with dietary patterns, food types, and nutrients in children and adolescents aged 2–19 years; Mediterranean dietary patterns (vegetables and fruits, which are rich in fiber, vitamin C, and vitamin E) were associated with lower levels of proinflammatory biomarkers (C-reactive protein, interleukin-6, and tumor necrosis factor-α), whereas Western dietary patterns (containing added sugars and saturated fatty acids and ultra-processed foods) were associated with higher inflammatory biomarker levels [15]. Recent studies indicated dietary patterns as predictors of mental health problems and higher body weights among adolescents, suggesting inflammation as a critical pathway in this relationship (graphical abstract) [19]. However, few studies investigated diet quality and its relationship with inflammatory responses in children and adolescents. Table 3 shows recent observational studies of the association between the Mediterranean diet and inflammatory responses in children and adolescents [20-25]. Five studies showed a lower inflammatory response in the blood with a Mediterranean diet [20,22-25], while another of people with type 1 diabetes showed no difference [21].
Mental health
Diet quality is associated with mental health conditions such as depression and anxiety across countries and cultures [8]. Poor nutrition may impair an individual's rapidly developing brain and cognitive function, and a low-quality diet may deteriorate a child's academic achievement [26]. Meanwhile, a high-quality diet is associated with improved mental health among children and adolescents [27]. Diet quality differs considerably among adults with depression and controls [28]. The symptoms of depression and fatigue are associated with increased inflammation of the immune and nervous systems, and both depression and chronic stress involve persistent activation of the hypothalamic-pituitary-adrenal axis (Fig. 1) [29,30]. Proinflammatory cytokines such as interleukins and tumor necrosis factor-α appear to be driving this activation via the prolonged secretion of cortisol. This can have profound negative effects on brain structures such as the hippocampus, amygdala, and prefrontal cortex (Fig. 1) [29].
Suggested role of dietary inflammation in mental health problems. A diet high in sugar, refined flour, saturated fats, and red processed meat contributes to inflammation. Low-grade chronic inflammation and immune system activation with prolonged exposure to an unhealthy diet may play a role in the development of neuropsychiatric disorders. Elevated levels of pro-inflammatory cytokines (C-reactive protein, interleukin-6, and tumor necrosis factor-ɑ) are activated by prolonged cortisol secretion, both directly by stimulation of the hypothalamic-pituitary-adrenal axis and indirectly by increased sensitivity of glucocorticoid receptors. Increased levels of inflammatory cytokines affect brain structures such as the hippocampus, amygdala, and prefrontal cortex. These relationships can be complex and are potentially bidirectional.
Most mental disorders begin early in life but are not detected until later in life. Self-harm and suicide are primary cause of deaths among young people [7]. Therefore, the onset patterns of psychiatric disorders should be identified during childhood and adolescence [31]. Depression affects 7.4% of adolescents aged 10–14 years globally [7]. A recent Australian cross-sectional study reported that 10–14-year-olds with a less healthy diet according to the Australian Dietary Guidelines were at increased risk of developing depressive symptoms [32]. A cross-sectional study of about 3,000 adolescents aged 11–14 years in the United Kingdom found a close relationship between the intake of unhealthy foods and mental health symptoms on the Strengths and Difficulties Questionnaire [33]. The Childhood to Adolescence Transition Study in Australia of 787 children aged 8–9 years indicated that an overall good-quality diet is related to more positive mental health in preadolescents [8]. Diet quality was significantly associated with children's mental health (beta=-0.11; 95% CI, -0.18 to 0.04; P=0.004) [8]. The 2021 KYRBS reported [10] that 25.9% of middle school students and 27.7% of high school students experienced depression. However, no studies have examined the association between depression and diet quality among children and adolescents in Korea.
A systematic review of studies of diet-related behaviors and mental health published between 1978 and 2017 identified that healthy dietary patterns and food quality positively impact mental health [7]. The ingestion of several healthy foods, such as olive oil, fish, nuts, legumes, dairy products, fruits, and vegetables, is inversely associated with the risk of depression and associated symptoms [7]. Adverse food patterns such as a poor appetite, skipping meals, and a dominant desire for sweet foods are prerequisites and main causes of depression [7]. However, little is known about problems such as anxiety, eating disorders, school absences, poor academic performance, physical symptoms, or behavioral problems [34,35].
Attention deficit hyperactivity disorder (ADHD) is significantly associated with poor diet quality, a low physical activity level, and increased time spent playing video games or watching television. Children who reported feeling "worried, sad, or unhappy" and experiencing "pain or discomfort" were more likely to have mental health problems and an ADHD diagnosis [36]. A cohort study of 1,352 students of 10–11-year-olds in Alberta, Canada, who were followed from birth to 2012 showed that 8.3% were diagnosed with ADHD [36]. Of the 4,875 students in the Canadian province of Nova Scotia, 9.7% of those aged 10/11–18 years had ADHD [37]. The diagnosis of ADHD was significantly less common among students with better diet quality, higher physical activity levels, and spending less time on computers and video games (P<0.05) [37]. A longitudinal study in Canada showed that poor diet quality and a low physical activity level among students in grade 5 were associated with increased diagnoses of both internalizing disorders and ADHD during childhood [36]. In Korea, an unhealthy diet pattern, characterized as a diet high in sugar, salt, and saturated and total fat but low in whole grains, fish, fruits, and vegetables, was associated with increased ADHD symptoms [38].
Smoking, drinking, and drug use
Adolescents, whose brain and neurotransmission systems are under development, are more susceptible to abuse when exposed to substances such as alcohol and drugs (Fig. 2) [39]. Exposure to drugs such as cannabis, opioids, cocaine, and amphetamines is likely to affect their cognitive function, neurotransmitter systems, and gene expression [39]. Smoking in adolescents is correlated with depression and other mental health problems, alcohol use, disconnectedness from school or family, communication problems with parents, poor school performance, and peer smoking [40]. Thus, smoking is associated with unhealthy diet quality, mental health problems, and poor school performance. Adolescents who start smoking out of curiosity but become addicted have higher levels of nicotine-induced pleasure or nicotine dependence than adults [41]. According to the 2021 KYRBS [10], the lifetime smoking experience rate was 14.9%, current smoking rate was 6.7%, and daily smoking rate was 3.2%; the mean age at which they started smoking was 12.8 years. Early smoking experiences influence suicide attempts among Korean adolescent smokers [42]. In Korea, the Ministry for Health and Welfare, the Ministry of Education has provided anti-smoking programs to educate students since 2015 [43]. In 2020, the government launched a new no-smoking campaign named No-Dam Sapiens [44] to show that young people who do not smoke are healthy and fabulous. With this no-smoking campaign [43,44], the smoking rates among middle schoolers (1.9%) and high schoolers (7.2%) in Korea were not as high [10] as the global youth smoking rate of 34.8% [45].
Consequences of adolescent substance use. Adolescents are vulnerable to the detrimental effects of alcohol and other drugs. The prefrontal cortex is involved in both decision making and reward processing, and unique changes in this brain region that occur during adolescence are discussed in terms of their role in mediating addiction.
In Korea, the Ministry of Education, Ministry for Health and Welfare, Ministry of Gender Equality and Family has also provided educational programs to prevent youth drinking, but a majority (90%) of them focused on prohibiting alcohol sales to youth while other prevention activities were rare [46]. In 2021 KYRBS [10], 2.1% of the students responded that they drank alcohol 5 or more days to the point of blacking out or not remembering during the previous 30 days. Current drinking was reported by 5.6% of middle schoolers and 16.0% of high schoolers, while binge drinking was reported by 45.5% of all students, 30.3% of middle schoolers, and 51.0% of high schoolers [10]. It is difficult to distinguish the effects of substances such as e-cigarettes and cannabis from the effects of alcohol on adolescents’ drinking. It is important to understand the impact of alcohol exposure and drinking patterns on adolescents to help us further investigate drug use among Korea's youth [47].
According to a survey by the Ministry for Consumer Affairs in Korea, 60.6% of middle and high schoolers have consumed energy drinks; of them, 25% increased their consumption during specific periods like exams [48]. Among the high schoolers, 6.4% (more girls than boys) reported having used diet products [48]. The main motive for using such drugs is to lose weight or improve one's appearance, but 62.6% reported taking drugs to improve sexual performance [48]. The 2020 Drug Crime White Paper of the Supreme Prosecutors' Office in Korea published an increase in the number of young drug offenders under 19 years of age [47].
There have been cases of the illegal administration and distribution of fentanyl patches among teenagers. In 2020, there were 313 drug offenders under 19 years of age, an increase of 31.0% from 2019 and 158.7% from 2016 [47]. Adolescents are exposed to drugs through social media and the Internet (dark web), where they encounter advertisements for drugs. Drugs are inexpensive, and there are cases of their smuggling through overseas jobs and sale through messenger chat applications. Drugs are then easily accessed through social networks or the Internet [47]. The increase in drug use among youth is associated with juvenile delinquency and crime, presumably because delinquent youths have greater access to drugs and are more likely to commit crimes while under their influence. Drug and alcohol use are highly associated with suicide, with the former being a more significant risk factor than the latter.
Conclusion
Unhealthy diet-related behaviors or poor diet quality during childhood and adolescence are the main factors contributing to noncommunicable diseases and mental health problems via increased inflammatory responses (graphical abstract). Unhealthy diet-related behaviors can become lifelong habits, which can be associated with mental health problems as well as issues with smoking, drinking, and substance abuse. Biologically, the adolescent brain is not yet fully mature; therefore, exposure to nicotine, alcohol, and drugs can lead to withdrawal symptoms and dependence [39], making prevention programs very important. Diet-related mental health problems, such as depression and ADHD, can be reduced with healthy eating patterns, and a healthy diet quality can lead to body image confidence. Therefore, it is essential to actively educate adolescents about healthy eating, engaging in regular and sufficient exercise, and reducing sedentary behaviors [8,9].
For children’s and adolescents' physical and mental health, the distribution of diet-related behavior and diet quality should be evaluated annually; these data will aid the design of healthy diet-related behavior programs. Further studies are needed to investigate the impact of diet-related behavior and physical activity on children and adolescents in Korea with mental and physical problems, substance abuse, or addiction.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.