Balance assessment with decreased base of support for children with disabilities
Article information
Abstract
Background
Children’s ability to achieve an appropriate motor development is largely associated with their capacity to control balance. Furthermore, accomplishing balance tasks with a narrowed base of support is a necessary precursor to engaging in everyday functional activities and developing more complex balance abilities.
Purpose
To investigate the relationship between the tandem stance (TS) and the single-limb stance (SLS) items of the Pediatric Balance Scale (PBS) assessment tool with the PBS total score in children with impaired balance.
Methods
Forty-two children (22 with neurological disabilities, 10.7±3.1 years; 20 typically developing [TD], 8.3±2.7 years) performed all 14 PBS items. Linear regressions separately determined the impact of TS and SLS on total PBS score in both groups. Bland-Altman plots expressed agreement between the balance measurements.
Results
For children with disabilities, only the SLS entered the model, explaining 64.5% of the variance in total PBS score. A high level of agreement was observed between the SLS and total PBS scores. For TD children, only the TS entered the model, explaining 45.2% of the variance in the total PBS score. A high level of agreement was observed between the TS and total PBS scores.
Conclusion
Our findings support the practical and efficient use of a single balance task to assess balance ability in children with disabilities.
Key message
Question: Can a balance task with narrowed base of support indicate overall functional balance control in children with disabilities?
Finding: While single-limb standing could explain overall balance control for children with disabilities, it was unrelated with balance control for typically developing children.
Meaning: One balance task with narrowed base of support can be used as practical assessment of balance abilities for children with disabilities when allocated session time is of concern.
Introduction
Children’s ability to perform fundamental movement skills and achieve appropriate motor development is largely associated with their capacity to control balance [1,2]. Accomplishing balance tasks with a narrowed base of support, such as the tandem stance (TS) and single-limb stance (SLS), are necessary precursors to developing more complex balance abilities and are key in evaluating children’s performance of balance control [3]. Moreover, accomplishing tasks such as TS and SLS are necessary for every day functional activities such as gait and stair negotiation. While typically developing children can master balance tasks with a narrow base of support between ages 4 and 5 years, these tasks can be challenging even for postpubescent children with neurologic disorders [3-5].
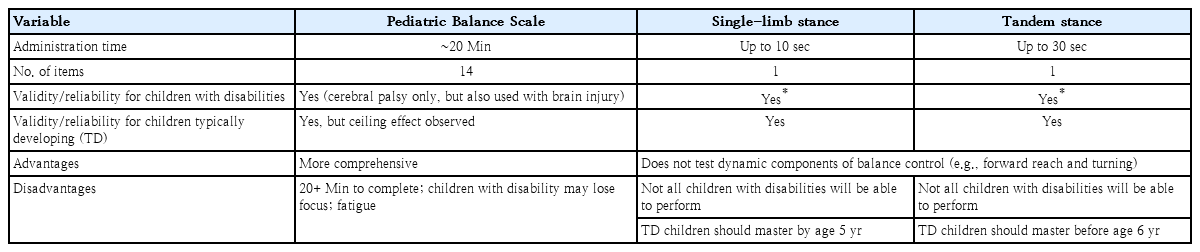
The Pediatric Balance Scale (PBS), a battery of 14 test items, evaluates functional balance during tasks that mimic experiences of everyday living [6]. This assessment tool is used extensively in clinical and research settings and is valid and reliable for a wide array of diagnoses in the pediatric patient population [7-11]. Performance of certain items, however, may not accurately represent a child’s balance abilities since the time required to maintain stationary postures are unfeasible for some young children or those with attention deficits secondary to a neurologic insult, such as brain injury, cerebral palsy, or stroke [12-15]. The inability to tolerate the time demands of the entire battery of tests (please see comparison presented in Table 1), in contrast to the inability to perform a given balance task, may lead to inaccurate scores of a child’s true balance ability. Additionally, the known ceiling effect in PBS’s scoring system can limit quantification of balance improvements for both typically developing children and children with mild to moderate physical deficiencies [16,17].
When considering all 14 items of PBS, 2 items (TS and SLS) are unique since both require the need to control balance in the upright posture during a narrowed base of support. Furthermore, these tests alone are often used in the pediatric balance-related literature, explaining relationships between balance control and motor development [5,18-20], as well as predictive normative data across many pediatric diagnoses (National Institutes of Health Toolbox Standing Balance Test) [21,22]. Thus, the purpose of this study was to investigate the relationship between the TS and SLS items and the PBS total score in children with impaired balance secondary to neurologic injuries. We also investigated the relationship in typically developing children to verify whether observed relationships were unique to children with disabilities. We hypothesized that the TS and SLS sub-scores would explain a significant variance in the PBS total score for both groups.
Methods
1. Participants
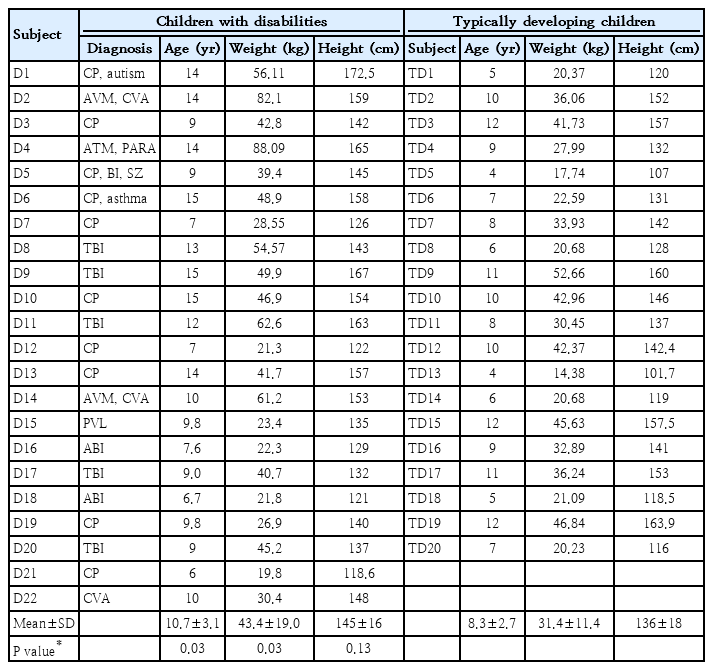
A convenience sample of 22 children with disabilities (12 females) and 20 typically developing children (8 females) participated in this cross-sectional study (Table 2). The primary inclusion criterion involved the ability to walk independently with or without assistive devices. The diagnoses of the children with disabilities are indicated in Table 2. One child with cerebral palsy (subject D7) and one child with traumatic brain injury (subject D9) used a reverse walker to ambulate.
2. Procedures
Participant recruitment occurred via word of mouth in local communities. According to the World Medical Association Declaration of Helsinki, parental informed consent and child assent forms were secured prior to participation in the study in which protocol was approved by the Institutional Review Board at Madonna Rehabilitation Hospitals. Clearance for participation was also secured from each child’s physician prior to engagement in research activities.
At the beginning of the data collection session, anthropometric measures were performed for each participant. Children then performed all 14 items of the PBS. The standardized protocol was followed in which items 1–14 were performed sequentially [6]. Rest was provided as needed between each test item. TS (i.e., standing with one foot in front) was the eighth item and SLS (i.e., standing on one leg) was the ninth item performed. PBS was administered to all participants by the same 2 experienced researchers (TWB, GMC).
3. Data analysis
Items from PBS are scored on a 5-point ordinal scale where each item is scored from 0 (unable to perform) to 4 (perform without difficulty). The maximum score achieved with all 14 items is 56 points. While scoring for some items use the ordinal scale alone, others use a prestipulated time to perform the item as basis for the ordinal scale score. For both TS and SLS a stopwatch was used to time the test. For a TS score of 4, children must place feet in tandem independently and hold the posture for 30 seconds; lower scores are related to feet positioning (3 and 2), need for assistance to step but still able to maintain posture for 15 seconds (score of 1), or inability to maintain balance while stepping or standing (zero). For SLS, children must lift one leg from the floor and independently maintain posture for 10 seconds (score of 4), between 5 and 9 seconds (score of 3), between 3 and 4 seconds (score of 2), or below 3 seconds but maintain the standing posture (score of 1); the score of zero is given to those who are unable to achieve the single-limb posture or require assistance to prevent a fall.
4. Statistical analysis
Forward stepwise linear regression analyses were used separately for children with disabilities and for typically developing children to determine the impact of TS and SLS (independent variables) on PBS total score (dependent variable). Multicollinearity was tested via the variance inflation factor (VIF). VIF values were calculated by running artificial OLS regressions between each independent variable inputted as a dependent variable. All VIF values obtained for both groups were under 4, indicating no correlation among the predictor variables [23].
Bland-Altman plots were used to quantify whether the tests TS or SLS were evaluating the same construct of balance measured via PBS. Thus, Bland-Altman plots were created to represent the between-test differences (i.e., PBS total score minus TS [children with disabilities] or PBS total score minus SLS [typically developing children]) versus the mean value of the 2 tests (i.e., average between PBS total score and TS [children with disabilities] or PBS total score and SLS [typically developing children]). The plots visually describe the agreement between measurements, suggesting good repeatability when 95% of the data points lie within 2 standard deviations (2SDs) of the mean difference [24,25].
All statistical analyses were performed with IBM SPSS Statistics ver. 28.0 (IBM Co., Armonk, NY, USA) and Excel (Microsoft Corp., Redmond, WA, USA) with significant levels set a priori at α=0.05.
Results
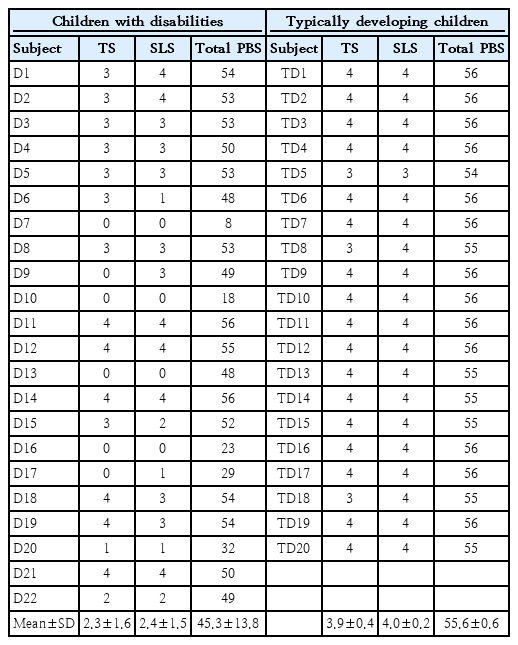
Individual scores for TS, SLS, and PBS total are presented in Table 3 to characterize performance from each group.
For children with disabilities, only SLS entered the model, explaining 64.5% of the variance in PBS total score (P<0.001, F change=36.4, Power=0.998). Higher SLS scores were associated with greater PBS total scores (Fig. 1A). The Bland-Altman plot demonstrated the high level of agreement between the 2 measures (SLS and PBS total score) with 95% of all data points falling within 2SD of the mean (Fig. 1C).
The top graphs display the relationship between total Pediatric Balance Scale (PBS) score and single-limb stance (SLS) score (A) for children with disabilities (n=22) and tandem stance (TS) score (B) for typically developing children (n=20). The lower graphs display the Bland- Altman plots representing the difference between SLS and PBS scores (C) versus the average of the scores from both tests for children with disabilities (note that only one of the data points fell outside the expected limits of agreement, 2 standard deviation [SD], expressed as the red dashed lines); and difference between TS and PBS scores (D) versus the average of the scores from both tests for typically developing children (note that all data points, with overlapping data, fell inside the expected limits of agreement, 2SD, expressed as the red dashed lines).
For typically developing children, only TS entered the model, explaining 45.2% of the variance in PBS total score (P=0.001, F change=14.9, Power=0.919). The correlation between TS and PBS total score can be seen in Fig. 1B. The Bland-Altman plot demonstrated the high level of agreement between the 2 measures (TS and PBS total score) with all data points falling within 2SD of the mean (Fig. 1D).
Discussion
Children with neurologic conditions and impaired balance engage less in physical and life activities compared with typically developing peers, followed by increased risk of secondary medical conditions and social isolation as they transition to adulthood [26-30]. Physical therapists play a critical role helping children improve/sustain balance, yet balance alone may not be the sole focus of evaluations and interventions [7,31]. Most clinical pediatric balance assessments are performed using the PBS, a comprehensive ~20-minute evaluation that involves the completion of 14 separate tasks [6]. Given realistic time constraints within healthcare and school-based therapy programs, identifying evaluations that can be used efficiently to screen for balance control challenges appears crucial not only for documenting underlying challenges, but also justifying treatment necessity to insurers. Our findings suggest that when time limitations and/or attention span limit administration of the more comprehensive PBS, then administration of the SLS may provide a meaningful proxy measure of the balance control capabilities of children with disabilities.
In agreement with our hypothesis, TS and SLS explained a large variance in PBS total score; however, each test contributed separately to the explanation of variance in PBS scores for each group. While SLS was the only test entering the model and explaining well over half of the variance (64.5%) of the PBS total score for children with disabilities, this test did not significantly explain the variance in PBS for typically developing children. Given that TS did not enter the model for this group, the difference in the posture between tests (i.e., both feet in contact with the ground versus one) appears critical. In addition to the modulated muscle activity required to maintain balance over a smaller base of support, the additional requirement of engaging lower limb and hip muscles to maintain one foot raised off the floor enhanced the difficulty in controlling posture by those with disabilities [5]. Moreover, the impaired ability to selectively control lower limb muscles can impact the child’s ability to position the center of mass above the now decreased base of support during SLS posture [32,33]. However, quantification of selective muscle control and its impact on balance control fall outside the scope of the current work.
Important to note that 4 children with disabilities scored zero on the SLS test. To further explore whether the performance outcome of these 4 children alone influenced abnormally the overall findings of our work, we performed a post hoc analysis excluding these 4 participants. The result of this analysis provided an R2 of 0.73 (P=0.011) and similar high statistical power (0.99). Thus, this exploratory post hoc analysis demonstrated that the wide range of balance performance of our sample was expected for children with disabilities instead of a limitation of the investigated sample after considering the 4 participants age and diagnoses.
Interestingly, TS was the only test entering the model for our typically developing participants. Given the ages of our cohort of typically developing children, our finding that SLS did not enter the model can be explained by the literature that suggests SLS is expected to be mastered by typically developing children by ages 5 years [3,4]. While all our participants maintained the TS posture for 30 seconds, 3 children were unable to achieve the required distance (i.e., foot’s length) between heel and toe, receiving the score of 3. Therefore, they were not able to receive the full score of 56 in PBS (54 and 55 points). Given these 3 participants were amongst the younger children from our sample (ages 4, 5, and 6 years), these results corroborate with the expected age-related motor development and balance control seen with the ceiling plateau of PBS scoring around the age of 4.5 years [34].
The analysis of the agreement between PBS and the 2 tests investigated in this study via the Bland-Altman plots allowed for further clinical interpretations to our findings. Both comparisons suggest that one test, i.e., SLS for children with disabilities and TS for typically developing children, can provide comparable balance scoring in comparison to the full battery of tests of PBS (Fig. 1C and D). However, one should note the difference between the 2SD boundaries for both groups. These boundaries indicate the variability in balance performance when analyzing children with disabilities (PBS–SLS) versus typically developing children (PBS–TS). Thus, the larger spread of data points for children with disabilities, observed as approximately 28 times greater than the spread for typically developing children, indicates the greater variability in scores when attempting to perform the SLS task. Although greater variability was expected for those with disabilities in comparison with their typically developing peers given the heterogeneity of motor function emerging from the neurologic injury (since severity of residual deficits can impact reactive balance control), SLS still provided good repeatability of balance measure with only one data point outside the suggested 2SD [35].
Since between-groups comparison was not the design of this study, the groups were not matched by anthropometrics nor age. Additionally, we chose to include children with a wide variety of diagnoses to provide a comprehensive set of motor impairments; however, investigating a group without a focused diagnosis might have increased the motor function heterogeneity of the sample. Lastly, although TS and SLS are key tasks to identify issues with balance control [5,18-22], including more items from PBS into the regression model can provide greater clarification regarding which items are in agreement with the full balance assessment [3,5]. Future work should utilize larger cohorts of children in accordance with the number of variables entering the regression model to confirm our findings, while achieving similar statistical power to our study, and expand on other tests that could facilitate an expedited clinical pediatric balance assessment.
In conclusion, the large variance of the PBS total score that was explained by SLS alone support the use of one balance task as practical assessment of balance ability for children with disabilities when allocated session time is of concern. Given age-expected mastery of SLS motor control by typically developing children, this balance task may not be used for this cohort as a screening tool of balance capabilities. However, further work with larger samples and dedicated diagnoses are needed before findings can be directed as assessment recommendations for a time-efficient evaluation of pediatric balance control.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contribution
Conceptualization: GMC, MG; Data curation: TWB, GMC; Formal analysis: GMC, TWB, MG; Methodology: GMC, TWB; Project administration: JMB, GMC; Visualization: MG, TWB; Writing-original draft: GMC; Writing - review & editing: JMB, GMC