Value of transabdominal ultrasonography for diagnosing functional constipation in children: a systematic review and meta-analysis
Article information
Abstract
Transabdominal ultrasonography is increasingly used as a novel modality for detecting pediatric functional constipation (FC). This systematic review and meta-analysis aimed to assess the diagnostic parameters of FC including rectal diameter (RD) and anterior rectal wall thickness. A systematic search was conducted of the Ovid MEDLINE, Embase, Scopus, and PubMed databases through September 29, 2023, to identify studies comparing RD and anterior wall thickness using transabdominal ultrasonography in children with versus without FC. Metaanalyses were performed using random-effects models to calculate the weighted mean differences (MDs) in RD and anterior wall thickness. Comprehensive Meta-Analysis ver. 3, R, and Review Manager ver. 5.4.1 software were used to assess the optimal cutoff, sensitivity, specificity, and area under the curve (AUC). Fourteen studies involving 1,255 children (mean age, 6.21±2.3 years) were included. The mean RD was significantly larger in constipated children versus controls (MD, 10.35 mm; 95% confidence interval [CI], 6.97–13.74; P<0.001; I2=94%). A meta-regression showed no significant effects of age, weight, or height on RD. An optimal RD cutoff point of 31 mm was suggested by a pooled analysis with an AUC of 0.86 (95% CI, 0.8–0.91; P<0.001), sensitivity of 0.75 (95% CI, 0.59–0.86), and specificity of 0.84 (95% CI, 0.68–0.93). The mean anterior rectal wall thickness was greater among constipated children than among controls (MD, 0.44; 95% CI, -0.26 to 1.13; P=0.22), but this difference was not statistically significant. RD measured using transabdominal ultrasonography with a cutoff point of 31 mm exhibited good diagnostic accuracy for diagnosing FC in children.
Key message
· Functional constipation in children places great burden on their physical and psychological well-being; hence, its prompt diagnosis is needed.
· A larger rectal diameter in children with functional constipation was proposed as a noninvasive diagnostic parameter.
· This meta-analysis highlights the clinical usefulness and optimal cutoff value of rectal diameter measured using transabdominal ultrasonography as a diagnostic criterion for functional constipation in children
Graphical abstract. AUC, area under the curve; CI, confidence interval.
Introduction
Functional constipation (FC) is a common functional gastrointestinal disorder in pediatric patients, accounting for up to 25% of visits to pediatric gastroenterologists [1] with a global prevalence of 14.4% among children [2]. This condition significantly increases healthcare costs [3,4] and adversely impacts children's quality of life and psychological well-being [5]. Thus, the early diagnosis and timely management of FC in children are essential.
The Rome criteria have long been the primary diagnostic tools for FC in children. These criteria incorporate an assessment of medical history, such as infrequent bowel movements, withholding behavior, painful defecation, large stools, soiling among toilet-trained children, and history of stool blockages, along with a clinical examination, particularly noting the presence of large stools in the rectum [6,7]. Clinical assessments typically involve an abdominal examination and/or digital rectal examination (DRE) to detect a rectal fecal mass, which is found in approximately 30%–75% of diagnosed cases of FC [1,8,9].
However, DRE is often avoided by physicians, especially in young children, because of its discomfort and invasiveness, which can lead to fear of defecation and complicated constipation treatment [10]. The absence of information about large stools in the rectum can complicate FC diagnostics. Additionally, other diagnostic tools such as abdominal radiography have low accuracy for differentiating fecal load from fecal impaction [11].
Transabdominal ultrasonography recently emerged as a promising alternative for assessing fecal impaction or large stools in the rectum since it is easy to perform, noninvasive, and free from radiation exposure, making it well accepted by children and their parents [12-15]. Additionally, systematic reviews indicated that larger rectal diameters (RDs) measured via transabdominal ultrasonography strongly correlate with the presence of large stools in the rectum as detected by DRE, suggesting its possible replacement [12-14,16,17].
In cases of withholding behavior, the accumulation of fecal matter in the rectum gradually causes rectal enlargement. Thus, measuring RD as an additional parameter for diagnosing FC in children represents a novel approach [18,19]. However, the lack of standardized cutoff points for RD across studies poses a challenge for clinical application. Other proposed parameters from transabdominal ultrasonography for diagnosing FC include anterior rectal wall diameter, large fecal content in the rectum, and rectopelvic ratio. Therefore, this systematic review and meta-analysis aimed to establish a reference for normal RD values in children and set criteria for dilation in cases of constipation. The values of other parameters were evaluated using transabdominal ultrasonography to diagnose FC in children.
Methods
This systematic review, meta-analysis, and meta-regression followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (Supplementary material 1). The protocol for this review was registered with PROSPERO (CRD42023430645) on June 9, 2023.
1. Literature review and search strategy
A systematic literature search was conducted of the Ovid MEDLINE, Embase, Scopus, and PubMed databases to identify publications comparing the RD and anterior wall thickness measured using transabdominal ultrasonography in children with versus without FC from inception until September 29, 2023. The search used terms encompassed the following 3 concepts: (1) children and pediatrics, (2) constipation, and (3) ultrasonography. MeSH (medical subject headings) database terms were used for the search (Supplementary material 2).
2. Eligibility criteria
This review included cross-sectional, case-control, and cohort studies comparing the parameters measured by abdominal ultrasonography (index test) in children under 18 years of age with or without a clinical diagnosis of FC (study domain) using modified Rome criteria and Rome criteria as the reference test. Studies are required to report data on parameters such as RD and anterior wall thickness measured using transabdominal ultrasonography. Only full-text articles were considered, while case reports, review articles, animal studies, and studies involving patients with organic causes of constipation were excluded.
3. Study screening and data abstraction
All search results were uploaded to COVIDENCE to manage duplicates. Prior to the data abstraction, citations were screened in 3 stages: (1) title and abstract screening, (2) retrieval and examination of the full text, and (3) full-text review. Step (1) was independently conducted by 2 investigators (DLT and PNTT) using COVIDENCE's voting function; conflicts were resolved by a third author (P Sintusek). The reasons for study exclusion are documented (Supplementary material 3). A standardized form was used to extract the data, which included study details such as author, year of publication, country, study design, population characteristics, method of parameters measured by abdominal ultrasonography, and outcomes (e.g., mean age, height, weight, RD, anterior rectal wall thickness, cutoff points, true positives, false positives, true negatives, and false negatives). Parallel extractions by the 2 investigators were cross-verified, and additional information was requested from the authors via email when necessary.
4. Risk of bias evaluation
Two authors (DLT and P Sintusek) independently assessed each study's risk of bias (RoB) using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) with 4 domains: patient selection, index test, reference standard, and flow/timing [20]. The first 3 domains were used to address the applicability concerns. Each domain was rated as low, unclear, or high risk. A study received a "low risk of bias" classification if all domains were rated "low" for both bias and applicability. Studies were deemed "high risk" if any domain was assessed as "high" and "unclear risk" if any domain was rated as "unclear."
5. Statistical analysis
Comprehensive Meta-Analysis software version 3 and Review Manager 5.4.1 (Cochrane Collaboration, London, UK) were used to conduct the meta-analysis. We used random-effects models in conjunction with the inverse-variance formula for continuous variables irrespective of heterogeneity. Three indicators—mean difference (MD), standard deviation (SD), and 95% confidence interval (CI)—were used to express the difference estimates. Heterogeneity was assessed using I2 statistics and categorized as insignificant (0%–25%), low (26%–50%), moderate (51%–75%), or high (>75%). Statistical significance was set at 2-tailed values of P=0.05. Data originally presented as median and interquartile range were converted to mean and SD formats using the method described by Wan et al. [21].
Comprehensive Meta-Analysis version 3 software was used to conduct a meta-regression to explore potential moderators influencing the effect size of RD, including mean age, mean height, and mean weight. A significant relationship between moderators and effect size was determined using Q model statistics with a value of P<0.05, indicating intergroup variation in RD according to the slope values of the significant moderators (z statistics, P<0.05).
We followed the method of Steinhauser et al. [22] using R package diagmeta in Rstudio for Mac OS to ascertain the ideal RD cutoff point and its corresponding sensitivity and specificity for detecting FC. Diagnostic accuracy was evaluated using the summary receiver operating characteristic (SROC) curve. An area under the curve (AUC) of <0.9 suggested very good performance, 0.8–0.9 suggested good performance, 0.7–0.8 suggested fair performance, and 0.6–0.7 suggested poor performance [23]. CI for AUC of SROC was conducted according to the Noma et al. [24] method using R package dmetatool in Rstudio for Mac OS.
Results
1. Characteristics of included studies
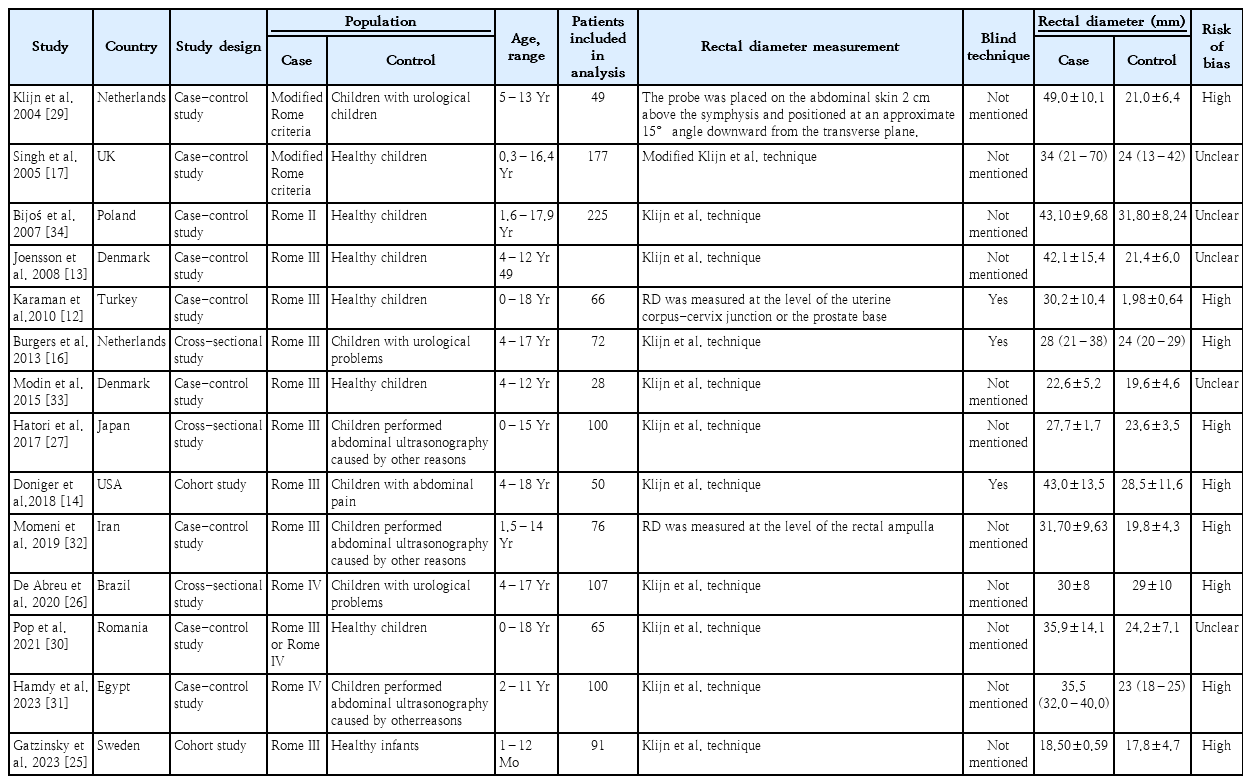
Using this search strategy, 3,479 potentially eligible articles were identified. After excluding 1,253 duplicates using management software, a title and abstract screening was performed, resulting in the removal of 2,198 irrelevant studies (Fig. 1). Subsequently, 28 articles were subjected to full-text assessment. During this step, 7 articles that lacked a control group, 3 conference reports, 2 articles with incorrect outcomes, 1 abstract-only article, and 1 article including duplicate data were excluded (Supplementary material 3). Ultimately, 14 articles were included in the analyses, including 2 cohort studies [14,25], 3 cross-sectional studies [26-28], and 9 case-control studies [12,13,17,29-34]. The mean age of children with FC was 6.21±2.3 years. The characteristics of the included studies are listed in Table 1.
The application of QUADAS-2 to each study revealed that 9 articles had a high RoB and 5 articles had an unclear RoB. The domain ratings for each study are presented in Supplementary material 4.
2. Outcomes assessment
1) Rectal diameter
Fourteen studies (n=1,257) reported the RD measured using ultrasonography in children with and without constipation. The meta-analysis showed that the mean RD was significantly larger in children with constipation versus controls with high heterogeneity (MD, 10.35 mm; 95% CI, 6.97–13.74; P<0.001; I2=94%) (Fig. 2A).
Forest-plot analysis of rectal diameter in children (A) and subgroup analysis of study in different continents and condition of children in control group (B). CI, confidence interval; SD, standard deviation; IV, inverse variance; df, degrees of freedom.
Subgroup analyses across continents (America, Asia, Africa, and Europe) revealed no significant differences in RD between children with and without constipation (P=0.27). Similarly, a subgroup analysis based on the conditions in the control group (healthy children, children with urological problems, and those with other issues) showed no significant variance in RD (P=0.95) (Fig. 2B).
Meta-regression models examining the influence of mean age, weight, and height on RD in children demonstrated no significant association: mean age (coefficient, -0.022; 95% CI, -0.244 to 0.200; P=0.843), mean weight (coefficient, 0.011; 95% CI, -0.025 to 0.047; P=0.543), and mean height (coefficient, 0.025; 95% CI, -0.031 to 0.081; P=0.385) (Supplementary material 5).
A funnel plot analysis indicated a relatively symmetrical inverted shape (Supplementary material 6).
2) Anterior rectal wall thickness
Among the included studies, 3 (n=207) used ultrasonography to measure the anterior rectal wall thickness. The anterior rectal wall thickness was higher among constipated children than that of controls; however, this difference was not statistically significant. Additionally, there was high heterogeneity among studies (MD, 0.44; 95% CI, -0.26 to 1.13; P=0.22; I2=95%; random-effects model) (Fig. 3).

Forest-plot analysis of anterior rectal wall thickness in children. CI, confidence interval; SD, standard deviation; IV, inverse variance; df, degrees of freedom.
Funnel plot analysis indicated no inverted shape (Supplementary material 7).
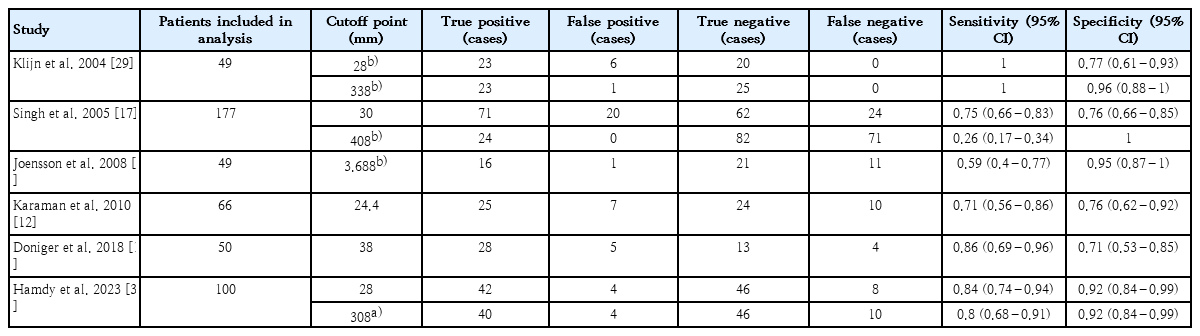
3) Diagnostic value of RD for FC in children
Table 2 presents the RD cutoff points for diagnosing FC in children from specific studies. The analytical results are illustrated in Fig. 4, which shows the SROC curve for RD for the diagnosis of FC. This indicates that an optimal cutoff point for RD at 31 mm, when measured using ultrasonography, can diagnose constipation in children with good accuracy (AUC, 0.86; 95% CI, 0.80–0.91; P<0.001), sensitivity of 0.75 (95% CI, 0.59–0.86), and specificity of 0.84 (95% CI, 0.68–0.93).
Discussion
This meta-analysis showed a significantly larger RD measured using transabdominal ultrasonography among constipated children than controls, albeit with high heterogeneity among participants. An RD cutoff value of 31 mm demonstrated a good diagnostic value when Rome criteria were used as the diagnostic standard for FC. In contrast, anterior rectal wall thickness measured using the same method did not significantly differ between constipated children and controls across the pooled data.
The heterogeneity of the control group may have influenced the results of this meta-analysis. However, the subgroup analyses across continents consistently showed a larger RD in children with constipation, underscoring the robustness of this finding. Additionally, the larger RD in constipated children appeared to be independent of concurrent conditions observed in the control group, suggesting its utility as a diagnostic parameter for FC. This observation aligns with the pathophysiological mechanism of FC, particularly in younger children who exhibit withholding behavior, contributing to rectal dilation and potential megarectal development [18,19,35].
In 2014, the European Society for Pediatric Gastroenterology Hepatology and Nutrition and the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition recommended transabdominal ultrasonography as a straightforward and noninvasive method for assessing FC in children. However, owing to limited data availability at the time, particularly with only 4 studies evaluating transabdominal ultrasonography, the standardization of measurement conditions and establishment of average values are lacking. Consequently, these organizations do not advocate for transabdominal ultrasonography as a diagnostic tool for FC [36].
To date, numerous proposed RD cutoff values using transabdominal ultrasonography for diagnosing FC have been suggested [12-14,27,29,32,37], with some studies indicating variations in children's age, weight, and height [12,17,30,38]. Despite conducting a meta-regression analysis to explore these variables, no statistically significant correlations with RD were found, likely due to the predominance of toddlers and young children in the analyzed data who were generally healthy or had minor illnesses unlikely to impact their growth parameters. Therefore, the cutoff threshold of 31 mm for RD can only be used for diagnosing FC in toddlers and young children and should be carefully applied to other age groups.
While this meta-regression analysis did not identify significant associations among age, height, weight, and RD, limitations in the collected data hindered further exploration of factors such as bladder volume, fecal incontinence, and duration of constipation symptoms [31,39]. Future studies could benefit from investigating these aspects as well as evaluating alternative parameters such as the rectopelvic ratio proposed by Bijoś et al. [34] for diagnosing FC in children.
Anterior rectal wall thickness is a proposed parameter for diagnosing FC. However, only 3 pooled studies have reported such measurements. Two studies conducted by Karaman et al. [12] and Pop et al. [30] showed higher anterior rectal wall thicknesses in constipated children than healthy controls. Conversely, the study by Momeni et al. [32] showed lower anterior rectal wall thicknesses in the constipated group than in children who underwent transabdominal ultrasonography for other reasons. An analysis of these studies indicated no significant relationship with FC, suggesting that it may not serve as a reliable diagnostic indicator for this condition. Similarly, while transabdominal ultrasonography shows promise for detecting fecal impaction [11,16,40], its role in replacing DRE remains under review.
This meta-analysis has several limitations. First, we were unable to comprehensively investigate all potential factors influencing RD, including bladder filling, time of last defecation, fecal impaction, and duration of constipation symptoms, due to data restrictions from previous studies. Second, each study included in the pooled analysis had a relatively small sample size and exhibited heterogeneity. Third, most studies had a high RoB, mainly because of the lack of blinding in the RD evaluation. To enhance our understanding and refine the diagnostic utility of RD in constipated children, future research should prioritize larger cohorts and standardized methodologies. This approach would enable a more comprehensive exploration of the factors influencing RD, as well as anterior wall diameter and fecal content, thereby providing clearer insight into its diagnostic implications.
In conclusion, this meta-analysis demonstrated a statistically significant difference in RD measured using transabdominal ultrasonography between constipated and non-constipated children. Using a cutoff value of 31 mm, transabdominal ultrasonography exhibited good diagnostic accuracy for FC in children. Given its noninvasive, safe, and well-accepted nature among children, it can effectively assess RD, a parameter that can be integrated into the Rome diagnostic criteria for FC in children.
Supplementary materials
Supplementary materials: The supplementary materials 1-7 for this article is available at https://doi.org/10.3345/cep.2024.00927.
Supplementary material 1. PRISMA checklist
cep-2024-00927-Supplementary-material-1.pdfSupplementary material 2. Search queries
cep-2024-00927-Supplementary-material-2.pdfSupplementary material 3. Characteristics of excluded studies
cep-2024-00927-Supplementary-material-3.pdfSupplementary material 4. Risk of bias assessment according to QUADAS-2 tool.
cep-2024-00927-Supplementary-material-4.pdfSupplementary material 5. Meta-regression of mean difference in rectal diameter on mean age (A), height (B), and weight (C).
cep-2024-00927-Supplementary-material-5.pdfSupplementary material 6.
cep-2024-00927-Supplementary-material-6.pdfSupplementary material 7.
cep-2024-00927-Supplementary-material-7.pdfNotes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This research was supported by the Ratchadapisek Sompoch Endowment Fund (2023), Chulalongkorn University (Meta_66_007_3000_002) and Thailand Science Research and Innovation Fund Chulalongkorn University (HAE663000047).
Author contribution
Conceptualization: PSintusek, DLT; Data curation: DLT, PNTT, PSintusek; Formal analysis: DLT, NTP; Methodology: PSintusek, DLT, PSusantitaphong; Project administration: PP, PSusantitaphong; Writing - original draft: PSintusek, DLT; Writing - review & editing: PSintusek, DLT