Knowledge, attitude, and practice regarding dengue vaccine: a baseline study of community members and health providers in Indonesia
Article information
Abstract
Background
Despite recent behavioral interventions aimed at reducing the burden of dengue, persistent unfavorable related behaviors in the Indonesian community suggest that vaccination could be effective. However, before this is implemented nationally, public perception and acceptance of the vaccine should be assessed in addition to health providers’ points of view.
Purpose
This study aimed to assess the knowledge, attitudes, and practices (KAP) of community members and health providers in Indonesia.
Methods
A cross-sectional survey was conducted in 6 districts of 3 Indonesian provinces. Respondents included both community members and health providers living within the territory of the selected primary health care centers. Pretested questionnaires were used to gather information on the sociodemographic characteristics and KAPs regarding dengue vaccines. An independent t test was performed to compare the mean KAP scores between community members and health providers, while a logistic regression analysis was used to identify the predictors in each domain.
Results
Only 18.5% of health providers possessed high knowledge of the dengue vaccine versus only 12.5% of community members. Approximately one-third of the health providers versus one-fourth of community members displayed a high to moderate score for attitudes about dengue vaccines. Dengue vaccination practices demonstrated a more favorable score for both health providers and community members at 59.1% and 41.1%, respectively. No individual sociodemographic characteristics were associated with KAPs; rather, only education was correlated with better dengue vaccination practices. We also found that good knowledge of dengue was the only factor associated with all domains.
Conclusion
Our findings highlight the urgent need to deliver educational interventions to health providers and community members in Indonesia to improve their awareness of dengue vaccines.
Key message
Question: Do community members and health providers show different level of knowledge, attitude, and practice towards dengue vaccine?
Finding: These 2 groups only differed in practice component, while the knowledge and attitude constituents were relatively low for both.
Meaning: There is an urgent need to deliver educational interventions to raise awareness of community members and health providers regarding dengue vaccination.
Graphical abstract
Introduction
Over the past 2 decades, the global burden of dengue fever (DF) has become a significant public health issue. A tenfold case increment, from 500,000 to 5,2 million, has been reported within this period, similar to the worldwide virus spread across 129 countries in 2019 [1]. Moreover, the incidence of this mosquito-borne disease is projected to escalate more rapidly due to human migration, rising population density, waste disposal practices, and climate change [2]. Expanding dengue transmission threatens the public health system, particularly in endemic low- and middle-income countries such as Indonesia.
Without specific antiviral treatment, preventive strategies are important and several measures have been taken to reduce virus transmission by the disease vector, Aedes sp. A national vector control program called “3 M Plus” has been implemented with behavioral modification requiring locals to take on the responsibility for locating and eliminating putative and existing mosquito nests in their neighborhood [3]. However, unfavorable dengue-related behaviors persist and contribute to the annual rise in incidence [4]. Currently, no single intervention can combat the virus spread.
Evidence suggests that a combination of vector control and vaccination may be the most successful strategy [5]. A dengue vaccine for endemic populations is clearly needed given the escalating magnitude and frequency of DF outbreaks, and the lack of long-lasting vector-control treatments [6]. It is considered a crucial, tailored strategy for dengue prevention and control, despite its vague efficacy and safety [7]. The World Health Organization Strategic Advisory Group of Experts has advised that vaccines should be administered in areas with high prevalence and rapid transmission, to optimize its benefits and reduce the dangers to seronegative individuals [8]. Therefore, assessing the public’s perception and likely engagement with the dengue vaccine is warranted to inform the specific approach to dengue prevention.
Several studies have been conducted to assess knowledge, attitude, and practice (KAP) regarding the dengue vaccine. Harapan et al. [9] found that only 42% of the Aceh community, the most northern region in Indonesia, had better knowledge about dengue vaccine, and 32% of them had a higher level of attitude and practice. A study in several high-risk countries assessed the public’s eagerness to pay for dengue vaccines as determined by financial aid and an assurance of government and medical care [10]. To the best of our knowledge, there is no study evaluating health provider’s perceptions and engagement with the dengue vaccine. Existing evidence assesses the KAP of health providers regarding dengue prevention [11], but does not specifically focus on vaccines. Health providers play a crucial role as a source of dengue vaccine information [9]. Hence, it is important to study KAPs to understand how health providers and the community perceive and accept the dengue vaccine.
Our study aimed to compare the dengue vaccine KAP of health providers and the community in Indonesia and determine the associated factors. It will provide evidence-based information to help close the gaps and serve as a benchmark for policymakers to enhance DF prevention and control. This will lessen the health burden and improve control over the spread of the dengue virus by encouraging vaccination and building public confidence in health providers and legislators.
Methods
1. Study design and settings
A quantitative cross-sectional survey was designed to assess dengue vaccine KAP. We studied 6 districts from 3 provinces in Indonesia: Bantul and Gunung Kidul (Yogyakarta), Karanganyar and Purbalingga (Central Java), and Buleleng and Badung (Bali). We studied one urban and one rural Primary Health Center (PHC) in each district. Between May and September 2022, each respondent received pretested questionnaires.
2. Sampling and sample size
We used the purposive sampling method to define the study site based on Indonesian DF prevalence. The DF burden mostly impacts 10 provinces in Indonesia, including Bali and Yogyakarta. Central Java has the highest case fatality rate. Bali was selected as our study site because it has distinctive cultural backgrounds from Yogyakarta and Central Java. Central Java is the nearest province to Yogyakarta. We used the convenience sampling method to reach the health providers and community respondents.
All available staff from selected PHCs who were willing to fully participate and signed the informed consent were included. The respondent must be responsible for the position at least for 1 year. For community member, there should be any representative from parents of children aged 1–11 years old, parents of adolescents aged 12–17 years old, and adults aged 18–60 years old. The respondents and their family should leave within the working area of selected PHCs. Every respondent who worked as a healthcare professional was excluded. To maintain a balanced proportion across the study sites, we required 60 respondents from each district. With a confidence level of 95% and a 5% margin of error, we targeted 360 participants for our minimum sample size.
3. Study variables
1) Explanatory variables
We collected sociodemographic characteristics such as age and sex, and gathered data from PHC health providers on length of service (in years), and employment status. We collected education, occupation, insurance ownership, and monthly household expense data from the community respondents. Their province and type of residence were the only factors in determining the health provider and community members.
We also asked several questions regarding knowledge about dengue in general, such as the cause of DF, virus transmission, signs and symptoms and the severity of DF. A correct answer was given a score of one, a wrong answer, zero. To score the answers, we divided the total number of questions by 100. A score for dengue knowledge of less than 70 was classed as a “low” score, while a score greater than 70 was classed as “higher.” [12] The DF history of health providers and community members was assessed by asking if they had been diagnosed with the disease within the last 5 years.
2) Outcome variables
The study outcomes were knowledge, attitude, and practice regarding the dengue vaccine. There were 11 questions explicitly about the dengue vaccine. An incorrect answer was given a score of zero, while correct answers scored one. The scoring formula was the total number of questions, divided by the total knowledge score, multiplied by 100. We categorized the results into “low” and “high” scores. For knowledge, less than 70 constituted a “low” score [12].
Fourteen questions were asked of respondents to quantify their dengue vaccine attitude. The answers were on a 3-point Likert-like scale (agree, disagree, and neutral). A respondent who showed a positive attitude was given a score of one, while others were zero. We divided the total attitude score by 14 and multiplied the result by 100 to arrive at the score. An attitude score over 60 was categorized as “high-moderate,” and 60 or less was “low.” [11]
To assess dengue vaccination practice, respondents were asked 8 questions about their preferred role in encouraging vaccination in their surroundings, if it was implemented. There were only “yes” and “no” answers. Respondents who showed a willingness to encourage dengue vaccine implementation, scoring more than 60, were categorized as high-moderate, and a score of 60 or less was considered a lower score for practice [11].
4. Data collection
A set of validated questionnaires was distributed to the respondents in Bahasa. Along with sociodemographic characteristics, the questionnaires covered the basic knowledge, habits, and behavior of Indonesians in preventing the spread of the dengue virus, and society’s view and acceptance of the dengue vaccine for prevention of DF. After obtaining informed consent from the respondents, trained enumerators conducted face-to-face interviews. Before the study, the questionnaires were piloted with 30 participants by 2 trained surveyors in one Yogyakarta PHC (outside the study site). We did not include these participants in our final analysis.
5. Statistical analysis
Sociodemographic characteristics were described in frequency (n) and percentages (%) and we calculated the mean scores and standard deviation (SD) of KAP regarding dengue vaccine. We used the independent t test to answer the first objective. Statistical difference was determined if the mean difference of knowledge, attitude, and practice regarding dengue vaccine between health provider and community was not zero (difference ≠ 0) with P<0.05. To define the association between covariates and outcomes, we conducted simple logistic regression to obtain the crude odds ratio (cOR) between high-moderate and low scores of knowledge, attitude, and practice separately. Any covariate which presented a level of significance less than 0.25 (P<0.25) was subjected to multiple logistic regression analysis for obtaining the adjusted odds ratio (aOR), with P<0.05 indicating noteworthy association. The statistical analysis was performed with Stata/MP 17.0 (StataCorp LLC, College Station, TX, USA).
6. Ethical consideration
Our study was approved by the Medical and Health Research Ethics Committee, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada on September 10th, 2021, with reference number KE/FK/1016/EC/2021.
Results
1. Sociodemographic characteristics of the study participants
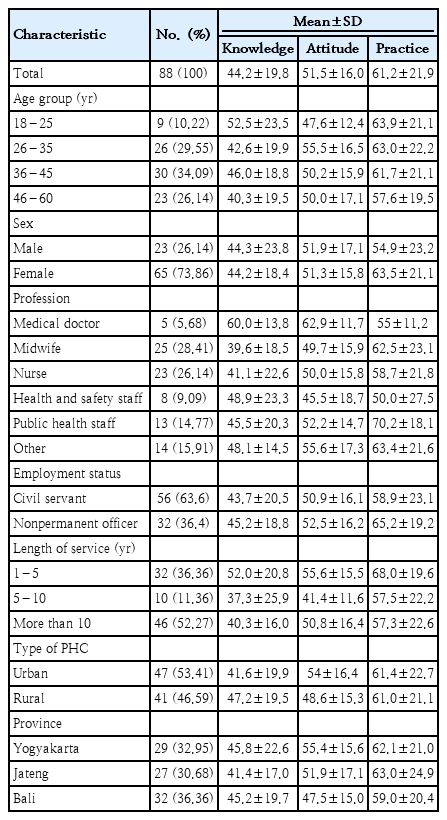
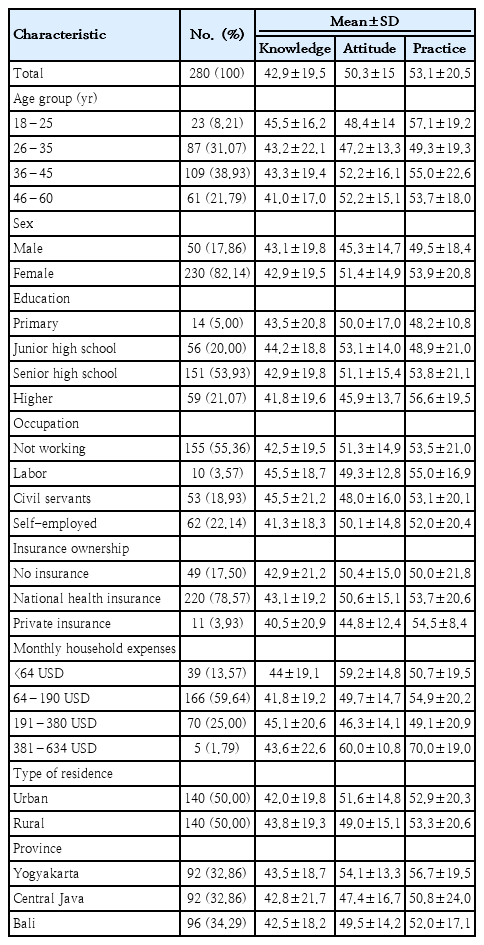
A total of 368 respondents who participated in this survey were included in the analysis, comprising 88 health providers and 280 community members (Tables 1 and 2). Most health providers and community members were 36–45 years old (34.09% and 38.9%, respectively) and female (73.86% and 82.14%, respectively). All the health providers had attained higher education, while 53.93% of community members had completed senior high school. There were 47 health providers from urban PHCs (53.41%), whereas the respondents from the community were equally split between urban and rural areas.
Among health providers, over 50% were midwives or nurses, with only around one-twentieth of the participants being medical doctors. Most health providers’ employment status was civil servant and over half of them had more than a decade of experience. The percentage of health professionals in each region varied, with Bali having the highest and Central Java the lowest.
Most of the community members had household expenses of 64–149 United States dollars (USD) monthly (59.64%), with less than 2% of them spending around 381–634 USD per month. About 22.14% of people in the community were self-employed, 18.93% were civil servants, and most were not working (55.36%). Only 17.5% of the community members had no health insurance. Across the regions, Central Java presented the largest percentage of community members, at 34.29%, whereas the distribution for both Bali and Yogyakarta was 32.86%.
2. Knowledge regarding dengue vaccine
Our study showed that only 18.2% of health providers and 12.5% of community members had a high level of knowledge. Yogyakarta health providers and community members scored the highest for dengue vaccine knowledge. Interestingly, both rural health providers and suburban inhabitants had a higher knowledge score compared to their urban counterparts (Tables 1 and 2). There was no statistically different knowledge score between health providers and the community (Table 3).
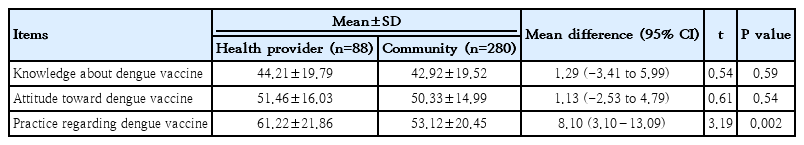
Mean difference in knowledge, attitude, and practice toward dengue vaccine between health providers and community members (n=368)
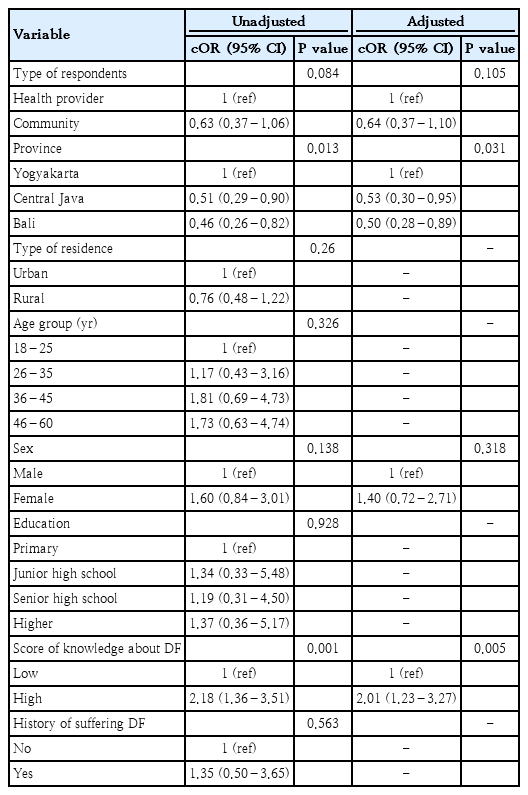
Factors associated with knowledge regarding the dengue vaccine were age, score of knowledge about DF, and history of suffering from DF (Table 4). This study showed a declining likelihood of having higher dengue vaccine knowledge with increasing age. Respondents who were well-informed about general dengue knowledge had a 2.18 (95% confidence interval [CI], 1.20–3.95) times higher chance of understanding the dengue vaccine compared to respondents with lower general dengue knowledge. Moreover, those who had experienced DF within 5 years preceding the survey had increased odds of higher knowledge regarding the dengue vaccine than those never diagnosed with DF.
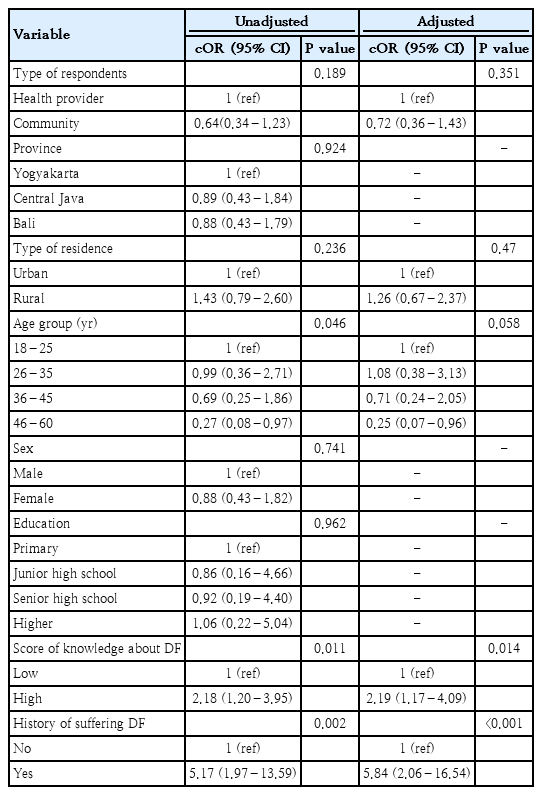
Crude and adjusted odds ratios of predictors in determining knowledge level regarding dengue vaccine (high vs. low) (n=368)
After adjusting for significant covariates (P<0.25), we found both the score of knowledge about DF in general and the history of suffering DF were important predictors for higher knowledge regarding the dengue vaccine. Respondents who were more aware of DF in general would be more likely to have a high knowledge of the dengue vaccine (aOR, 2.19; 95% CI, 1.17–4.09). Additionally, a history of DF increased the likelihood of comprehending the dengue vaccine by sixfold compared to those who did not have a history of DF (aOR, 5.84; 95% CI, 2.06–16.54).
3. Attitude toward dengue vaccine
Approximately 33% and 23.5% of health providers and community members, respectively, showed high-moderate attitude toward dengue vaccine. A higher score was found in both health providers and the community in urban areas. Among the 3 regions, Yogyakarta showed the highest attitudes scores of either health providers or the community (Tables 1 and 2). However, we found no statistically different attitude scores between health providers and the community.
The significant independent variables of high-moderate attitude toward dengue vaccine were province and score of DF knowledge in general. Respondents from Central Java and Bali were approximately 50% less likely than respondents from Yogyakarta, to show a highly positive attitude toward the dengue vaccine (Table 5). As with vaccine knowledge, knowledge about dengue in general was significantly associated with having a high-moderate attitude toward dengue vaccine (cOR, 2.18; 95% CI, 1.36–3.51; P<0.01). Even after conducting multivariable analysis and adjusting for other potential confounders, both predictors remained significant in determining the probability of a better attitude toward dengue vaccine (P<0.05).
4. Dengue vaccine practices
In contrast to knowledge and attitude, the majority (59.1%) of health providers had a high-moderate dengue vaccine practice score. Meanwhile, approximately 41.1% of the community showed a high-moderate score for dengue vaccine practice. Urban and rural inhabitants had similar scores for health providers and community members. Health providers from Bali scored the lowest (mean±SD, 59.0±20.4) among the regions, whereas the community from Yogyakarta scored highest (mean±SD, 56.7±19.5). All female respondents showed a higher vaccine practice score than males did. There was a statistically different mean score between health providers and the community (mean difference, 8.10; 95% CI, 3.10–13.09; P<0.01) (Table 3).
Table 6 presents the unadjusted and adjusted correlations between the independent variables and dengue vaccine practice. The community members had a significantly lower chance of having a high-moderate practice of dengue vaccine than health providers, (cOR, 0.48; 95% CI, 0.30–0.79; P<0.01). Our study also identified a trend toward better practice of the dengue vaccine based on education level. The higher the education level, the higher the odds were of having high-moderate practice (P<0.01). This was also the case with those who scored high in dengue knowledge in general and those who had a history of DF.
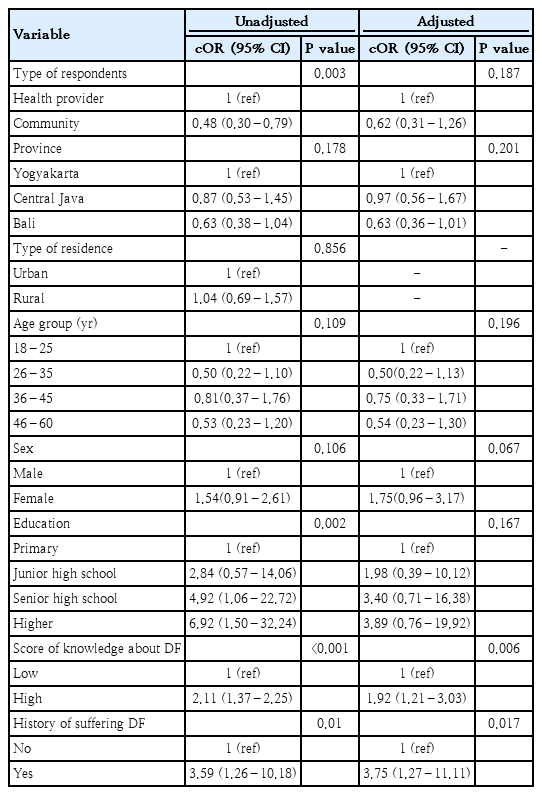
Crude and adjusted odds ratios of predictors in determining level of dengue vaccine practices (high-moderate vs. low) (n=368)
We conducted multivariable analysis with variables with a level of significance less than 0.25. In the adjusted model, the type of respondent (health providers versus community) was no longer statistically significant as a predictor of dengue vaccine practice (aOR, 0.62; 95% CI, 0.31–1.26; P>0.05). Nevertheless, a high-moderate practice score was more likely to be found among those who demonstrated a high level of general DF knowledge (P<0.05) and who had a history of DF diagnosis (P<0.001).
Discussion
Our study assessed dengue vaccine KAP among health providers and the community in 3 different regions of Indonesia. Since there i0s an escalating trend of dengue cases in the country, a dengue vaccine study is important for developing preventive strategies. As nationwide DF immunization program has not yet been implemented in Indonesia, it leads to the inadequate training, continuing medical education, and further socialization about it to health providers. Hence, they do not have sufficient understanding about dengue vaccine. On the other hand, health providers’ knowledge is limited to dengue disease control, specifically about vector control and behavioral prevention, not the vaccine [13]. Thus, our study signifies the importance of measuring their knowledge prior to its implementation in national level. As in this study the knowledge of health providers is considerably low, it is imperative to provide educational interventions in order to upgrade their comprehension about dengue vaccine.
To assess their knowledge of the dengue vaccine, we assessed opinions of its importance. Most respondents agreed that the vaccine is important (Supplementary Table 1). This finding is in line with a study conducted in Brazil, which showed beliefs regarding dengue vaccine are frequently explained in terms of individual involvement with the coronavirus disease 2019 (COVID-19) pandemic. Dengue vaccination was considered one significant approach to support disease control measures [14]. However, only around a third of health providers and community respondents had ever heard about the dengue vaccine. The disparity in perceived importance and awareness of dengue vaccine highlights the need for comprehensive public health education interventions targeted at Indonesian society.
We found that health providers in Indonesia are not well-informed about the dengue vaccine, as only about one-fifth of them showed a high level of knowledge. This finding is in line with a study conducted in Ethiopia, which showed poor knowledge of DF prevention among medical professionals [11]. Evidence suggests that the general public mostly obtains dengue vaccine knowledge from healthcare providers [9]. However, this study showed that only 12.5% of the community fully understood the dengue vaccine. It highlights poor dissemination of dengue vaccine information by health providers to the general population.
According to the Table 1, medical doctors contributed the lowest proportion of all included health providers in this study. Meanwhile, vaccination program in Indonesia involves all of them to deliver vaccine information to community. However, unlike other groups, physicians expressed high-moderate knowledge and attitude regarding dengue vaccine. Our finding is in line with the previous study conducted in Togo, that clearly presents the superiority of knowledge regarding dengue prevention among physicians compared to other professionals like nurses and midwives [15]. It is clearly stated in this study that there are some gaps of KAP towards dengue vaccine occurring among health providers in Indonesia.
The respondents across 3 regions in Indonesia differed in their dengue vaccine attitude scores. We found Yogyakarta inhabitants had almost double the likelihood of a positive attitude toward dengue vaccine than those in Central Java and Bali. This finding might be due to the Wolbachia Mosquito Program in Indonesia, which was initially piloted in Yogyakarta. The program, which interferes with the capability of mosquitoes to spread the virus, has successfully decreased the incidence of symptomatic DF in Yogyakarta [16]. These undertakings contribute to higher engagement and awareness of dengue prevention in the community, and might also influence acuity and willingness to accept dengue vaccines, and encourage more comprehensive dengue prevention efforts in the region.
Most respondents felt that the dengue vaccine should be included in the national vaccination program. Although they considered dengue vaccination a health investment, most preferred not to pay for it (Supplementary Table 1). Our results are comparable to a study that asked inhabitants of Aceh, Indonesia, if they would accept free dengue vaccination [17]. Similarly, a COVID-19 vaccine study demonstrated that both health providers and the community do not want to buy the vaccine because of concerns about its safety, and problems with public perception [12]. Thus, the government has a crucial role in increasing vaccination rates by removing financial barriers and increasing public confidence, because the cost of the dengue vaccine may deter people from being vaccinated [18], particularly in marginalized communities.
Although the respondents had low knowledge and attitude regarding dengue vaccine, their practice scores were relatively higher, even though the community’s practice score did not pass the cutoff point. More health providers demonstrated high-moderate practice than the community respondents, which is due to the disparity in health literacy between them. Health providers are more likely than community members to have access to reliable information [19]. This confirms the ultimate benefit of enhancing the educational framework to encourage supportive vaccine practices among health providers [20].
Health providers and community members would recommend the dengue vaccine to others and were eager to volunteer in the dengue vaccination program (Supplementary Table 1). Most of them would vigorously support the DF vaccination campaign, with fewer than 10% showing no interest in being involved. However, around 62% of the community did not want to recommend the dengue vaccine on social media, possibly for fear of causing controversy, since the public’s perception of vaccination varies [21]. Concern about adverse reactions, a need for further knowledge, and a general lack of faith in vaccinations are the main causes of vaccine reluctance or refusal [22]. Furthermore, as disseminating information on social media becomes easier, negative opinions toward vaccination are increasing on the internet [23]. Therefore, addressing these challenges requires collaboration between health providers, authorities, stakeholders, and public figures to provide accurate information and promote the vaccine for preventing DF.
Our study identified that comprehending DF, for instance, the virus spread, vector, and prevention, was the only factor that was associated with dengue vaccine KAP. Respondents with a high level of dengue knowledge in general had a twofold higher likelihood of KAP regarding the dengue vaccine. The better-informed respondents are about dengue in general, the better are their KAP regarding the vaccine. Our findings support a substantial dengue educational intervention to influence positive behavior toward the dengue vaccine. Meanwhile, the history of suffering from DF is associated with higher knowledge and practice regarding dengue vaccine. This result is consistent with a study conducted in Thailand showing that primary school students with good dengue prevention practices were mostly those who had a history of DF [24].
Our study has some weaknesses regarding representativeness. As previously mentioned, that this study was only conducted among 3 provinces with highest DF cases, it did not cover respondents who live in some big cities from other provinces such as Jakarta, Bandung, and Surabaya, which are possibly more educated about dengue vaccine. Moreover, this study also did not analyze respondents from other parts in Indonesia, for instance Sumatera, or Eastern Indonesia, which could show similar or even lower scores of KAP toward dengue vaccine. Second, our study used convenience and purposive sampling methods, which might have excluded some groups and could affect the study’s generalizability. Although our study has derived proportional sample size from each site, the health provider’s distribution was not even because initially, it did not aim to compare results among health providers. This situation might lead to some underestimation of KAP score among certain groups.
Future investigations which carry more representativeness might be beneficial to gain accuracy in defining the KAP regarding dengue vaccine among community member, particularly in some areas which have not been covered in this study. Secondly, further study which aims to compare groups within health providers with larger proportional sample is also imperative to provide reliable comprehension about their KAP towards dengue vaccine. Thirdly, measuring the effectiveness of educational interventions to raise awareness about dengue vaccine could be conducted to ensure adequate understanding prior to its implementation as a national program.
Although some limitations occurred in this present study, to the best of our knowledge, this is the first study to evaluate the KAP of the dengue vaccine among health providers and community members in Indonesia. The findings reveal that health providers and the community had a low level of dengue vaccine knowledge and attitude. However, there is an obvious distinction in practice, as the health providers exhibited higher engagement with the dengue vaccine than the community did. By studying dengue vaccine comprehension and awareness of health providers and community members, our study addresses the knowledge gap in the current literature. Our comparative analysis provides valuable information for tailored interventions and public health approaches to the dengue vaccine.
In conclusion, this study provided a comprehensive understanding of the KAP of the dengue vaccine in Indonesia, particularly in the most dengue-affected regions. It demonstrated a low level of dengue vaccine knowledge and attitude of health providers and community members, highlighting the need for educational interventions to improve awareness. The only factor that correlated with dengue vaccine KAP was knowledge about dengue in general. The study showed that even though Indonesia is considered a dengue endemic country, the scarcity of dengue education in society remains high. Similar studies in other regions of Indonesia are required to provide a more comprehensive understanding.
Health providers play a crucial role in advocating vaccination to the community, and we recommended interventions to increase their dengue vaccine skills and knowledge. Health providers should be prepared before community interventions with dengue vaccine workshops or continuing medical education. Encouraging health providers can boost their confidence when facing the public. For the community, dengue health campaigns, not only during seasonal outbreaks, in PHCs, schools, and other public places, might be an indispensable measure for raising society’s awareness of dengue prevention and control.
Supplementary material
Supplementary Table 1 is available at https://doi.org/10.3345/cep.2024.00962.
Respondents’ attitude toward dengue vaccine as a national vaccination program
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contribution
Conceptualization: AW, ISL, RSP, JAT; Formal Analysis: WT, AW; Investigation: AW, ISL, RSP, JAT, AWEM; Methodology: ISL, JAT, AW; Project Administration: AWEM; Writing - Original Draft: AW, WT; Writing - Review & Editing: AW, WT