Intermittent sigh breaths during high-frequency oscillatory ventilation among newborn infants
Article information
Key message
Intermittent sigh breaths during high-frequency oscillatory ventilation can improve ventilation and oxygenation by enhancing lung recruitment. Although research on this approach in newborn infants is limited, some published studies suggest that sigh breaths are generally applied at a rate of 2–3 breaths/min with an inspiratory time of 0.5–1 second and pressure of current mean airway pressure + 5 cmH2O (maximum, 30 cmH2O).
Graphical abstract
High-frequency oscillatory ventilation (HFOV) is a lung-protective respiratory support mode that provides effective gas exchange with tidal volumes equal to or less than the anatomical dead space volume, typically with minimal pressure fluctuations [1]. To maintain an appropriate end-expiratory lung volume (EELV) for optimal lung recruitment, continuous distending pressure is adjusted as the mean airway pressure (MAP). HFOV is commonly used in term and preterm infants with respiratory distress. The combined use of HFOV and conventional mandatory inflation was proposed to facilitate lung recruitment [2]. Intermittent sigh breaths delivered during pressure-support ventilation in children improve oxygenation and gas exchange and decrease respiratory drive without major complications [3]. Furthermore, intermittent sigh breaths reportedly are well-tolerated and decrease the mortality rate among adults [4].
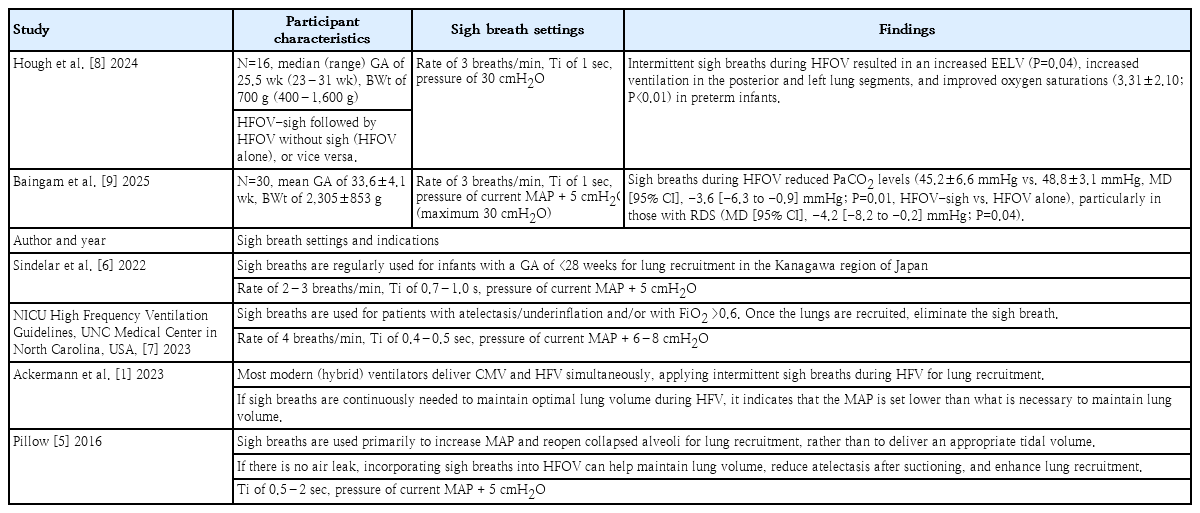
Despite many studies examining intermittent sigh breaths during invasive ventilation in children and adults, research is limited on intermittent sigh breaths during HFOV among newborn infants. Although some neonatal intensive care units (NICUs) deliver intermittent sigh breaths during HFOV to encourage lung recruitment, limited research has examined this approach. Table 1 summarizes the studies of and guidelines for delivering sigh breaths during HFOV among newborn infants.
Sigh breaths are primarily used to increase MAP and reopen collapsed alveoli to encourage lung recruitment rather than deliver an appropriate tidal volume. They are applied with a relatively prolonged inspiratory time of 0.5–2 seconds and pressure approximately 5 cmH2O higher than the MAP. If no air leak is present, incorporating sigh breaths into the HFOV can help maintain the newborn's lung volume, reduce atelectasis after suctioning, and enhance lung recruitment [5]. In the Kanagawa region of Japan, sustained inflation or sigh breaths are regularly used to encourage lung recruitment among extremely preterm infants with a gestational age of <28 weeks [6]. This approach delivers sigh breaths at a rate of 2–3 breaths/min with an inspiratory time of 0.7–1 second and pressure that is 5 cmH2O higher than the MAP. According to the NICU High Frequency Ventilation Guidelines at the University of North Carolina Medical Center in North Carolina, USA, sigh breaths are used for lung recruitment in patients with atelectasis/underinflation and/or a fraction of inspired oxygen >0.6. They are typically applied at a rate of 4 breaths/min with an inspiratory time of 0.4–0.5 second and pressure that is 6–8 cmH2O higher than the MAP. Once lung recruitment is achieved, sigh breaths are discontinued [7] (Table 1).
According to a study by Hough et al. [8] of intermittent sigh breaths administered during HFOV in preterm infants (n=16; median gestational age, 25.5 weeks; range, 23–31 weeks; median birth weight, 700 g; range, 400–1,600 g), intermittent sigh breaths were applied at a rate of 3 breaths/min with an inspiratory time of 1 second and pressure of 30 cmH2O. Infants who received versus did not receive intermittent sigh breaths during HFOV had increased EELV, increased ventilation in the posterior and left lung segments, and improved oxygen saturation.
Similarly, Baingam et al. [9] applied intermittent sigh breaths during HFOV at a rate of 3 breaths/min with an inspiratory time of 1 second and pressure that was 5 cmH2O higher than the MAP (maximum, 30 cmH2O) in term and preterm infants (n=30; mean gestational age, 33.6±4.1 weeks; mean birth weight, 2,305±853 g). The authors concluded that infants who received intermittent sigh breaths during HFOV had a decreased partial pressure of carbon dioxide (PaCO2) compared to those who did not, particularly those with respiratory distress syndrome. The only published studies on intermittent sigh breaths during HFOV in newborn infants are those by Hough et al. [8] and Baingam et al. [9], with only 2 ongoing clinical trials and little information in the literature (Table 1).
In conclusion, the administration of intermittent sigh breaths during HFOV can reduce PaCO2 levels, increase EELV, and improve ventilation and oxygenation in newborns by enhancing lung recruitment. Sigh breaths during HFOV are applied at a rate of 2–3 breaths/min, inspiratory time of 0.5–1 second, and pressure of current MAP + 5 cmH2O (maximum, 30 cmH2O). Although many NICUs provide intermittent sigh breaths during HFOV, there is little research on this approach and no evidence of its long-term benefit or safety. Thus, further research is required to determine the long-term benefits and safety of intermittent sigh breaths during HVOF and establish optimal settings based on birth weight among term and preterm newborns.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.