Success rates of conservative treatment and optimal surgical timing for pediatric chylothorax
Article information
Abstract
Background
Pediatric chylothorax poses management challenges, with conservative treatment as the first-line approach and surgery reserved for persistent cases. However, data remain limited on factors related to conservative treatment success and optimal surgical timing.
Purpose
This study aimed to evaluate the success rate of conservative treatment, identify the associated factors, and determine the optimal timing for surgical intervention.
Methods
We retrospectively reviewed pediatric chylothorax cases at Siriraj Hospital treated between January 2012 and December 2022. Clinical and laboratory parameters, treatment modalities, and outcomes were analyzed.
Results
Thirty pediatric patients were included (median age, 1.7 months); 67% were male. Conservative treatment had an overall success rate of 83.3% (25 of 30) and a 95% (19 of 20) success rate among patients with chylothorax after congenital heart disease surgery. Among the factors associated with successful conservative treatment, chylothorax caused by surgery was associated with a significantly higher success rate than nonsurgical causes (91.7% vs. 50%, respectively; P=0.04). The successful group exhibited a significantly lower peak pleural fluid flow rate than the unsuccessful group (26.8 mL/kg/day vs. 91 mL/kg/day, P=0.002). A time-to-event analysis showed that the success rate of conservative treatment for postsurgical chylothorax was 78% at 14 days, suggesting that 2 weeks may be the optimal timing for surgical intervention.
Conclusion
Conservative treatment is an effective first-line treatment for pediatric chylothorax. The etiology and peak flow rate of pleural fluid drainage are associated with its success. Optimized surgical intervention timing is crucial for improving outcomes.
Key message
Question: What is the success rate of conservative treatment for pediatric chylothorax, and when should surgical intervention be employed?
Finding: Overall success rate of conservative treatment was 83.3%. Surgically related etiologies and lower peak pleural fluid drainage rates were significantly associated with successful conservative management of pediatric chylothorax.
Meaning: If chylous drainage persists at ≥10 mL/kg/day beyond 2 weeks of optimal conservative treatment, surgical intervention should be considered.
Graphical abstract
Introduction
Chylothorax is a medical condition characterized by the accumulation of chyle, a lipid-rich lymphatic fluid, within the pleural cavity due to a disruption or rupture of thoracic lymphatic vessels. The etiologies of chylothorax include congenital anomalies, tumors, thoracic trauma, and postoperative complications, particularly following surgical interventions for congenital heart diseases [1,2]. The diagnosis of chylothorax is established when pleural fluid triglyceride levels exceed 110 mg/dL and the pleural fluid-to-serum cholesterol ratio of less than 1. In cases where pleural fluid triglyceride levels are below 110 mg/dL or the diagnosis remains uncertain, the presence of chylomicrons in the pleural fluid, detected through lipoprotein analysis, confirms the condition [1].
The management of chylothorax generally involves 2 main approaches: conservative treatments and surgical or interventional procedures. Conservative treatment focuses on reducing chyle production and its passage through lymphatic vessels, allowing lymphatic system to self-repair and seal the leaks. This approach typically includes dietary modifications such as a fat-free diet with or without medium-chain triglyceride (MCT) oil supplementation, total parenteral nutrition (TPN) with nil-per-os (NPO), and pharmacological interventions such as octreotide. Success rates for conservative treatment in pediatric chylothorax have been reported to range from 80% to 95% [3-7].
Various factors associated with unsuccessful conservative treatment have been identified. These include older age, higher peak chyle flow rates from tube thoracostomies, lower serum albumin levels [8], and greater drainage volumes on day 7 after initiating treatment [3]. Furthermore, pediatric patients with chylothorax resulting from thrombosis or high venous pressure in the superior vena cava, as well as those with congenital chylothorax or lymphangiomatosis, were at a higher risk of conservative treatment failure compared to those with chylothorax caused by direct thoracic duct injury [3].
Surgical or interventional procedures are generally considered when conservative therapy fails, with many authors recommending an extended trial period of 3 to 4 weeks before escalation [1-3,9,10]. Surgical options include thoracic duct ligation, pleurodesis, and pleuroperitoneal shunting. Indications for surgical intervention typically include chyle volumes exceeding 100 mL per year of age, clearly identifiable chyle leakage sites, and a high risk of malnutrition or immunosuppression [1]. However, the optimal timing for transitioning to surgical or interventional management remains controversial. Prolonged chylous leakage can lead to complications such as proteinenergy malnutrition, secondary immunodeficiency, and coagulopathy, which result in the increased risk of infection, prolonged hospitalization, and elevated mortality rates [11,12].
Given the variability in reported factors influencing conservative treatment outcomes and the lack of consensus on optimal timing for surgery, this study aims to evaluate the success rate of conservative management of chylothorax over the past 11 years. Additionally, it seeks to identify factors associated with successful conservative treatment and establish the appropriate timing for considering surgical intervention when conservative measures fail to achieve resolution.
Methods
This retrospective chart review was conducted at Siriraj Hospital, focusing on pediatric patients aged 0 to 18 years diagnosed with chylothorax between January 2012 and December 2022. Chylothorax was diagnosed based on newly developed pleural effusion and pleural fluid analysis demonstrating: (1) triglyceride levels >110 mg/dL in patients on a regular diet, or <110 mg/dL in those who were NPO or on a fat-free diet; (2) exudative pleural fluid with lymphocyte predominance >80% of total nucleated cells; and (3) sterile culture results. The study was conducted in accordance with the Declaration of Helsinki and approved by the Siriraj Institutional Review Board (COA No. Si 791/2023). Informed consent was waived due to the retrospective nature of the study.
In our clinical practice, pediatric patients diagnosed with chylothorax were initially managed with pleural fluid drainage and dietary modification, consisting of a fat-free diet with or without MCT oil supplementation. TPN with NPO status was initiated when the pleural fluid output remained above 10 mL/kg/day after 5–7 days of dietary management, when the initial pleural fluid drainage exceeded 100 mL per year of age, or when enteral feeding was contraindicated. Octreotide therapy was considered if the pleural fluid output remained high despite TPN administration, typically initiated in the second week after the initial diagnosis. Surgical interventions, such as thoracic duct ligation and pleurodesis, were considered when conservative management failed to reduce chyle output, typically after 4 to 6 weeks of treatment.
1. Data collection
Data were extracted from electronic medical records using a standardized data collection form. Demographic information gathered included age, sex, weight, length or height, and etiologies of chylothorax. Anthropometric assessments−including percentages of weight-for-age, weight-for-length/height, and length/height-for-age−were conducted using the Thai National Growth Charts provided by the Bureau of Nutrition, Department of Health, Ministry of Public Health, Thailand [13]. Clinical characteristics and relevant laboratory results from blood tests (serum albumin and absolute lymphocyte counts [ALCs]), and pleural fluid profiles (triglyceride levels, cell counts, cell differentiation, and culture) were examined. Pleural fluid drainage including initial volume drainage and peak flow rate were assessed. Treatment modalities, encompassing fat-free diets with or without MCT oil supplementation, TPN with NPO, octreotide, and surgical procedures, were also documented.
2. Outcome measures
The primary outcome was the success rate of conservative treatment, defined as patient survival and recovery from chylothorax without the need for surgical or interventional procedures.
The secondary outcomes included: (1) Identification of factors associated with successful conservative treatment by comparing etiologies, relevant clinical and laboratory parameters between the successful and unsuccessful conservative treatment groups. (2) Determination of time to response to conservative treatment, defined as the duration required to reduce pleural fluid drainage to less than 10 mL/kg/day.
3. Statistical analysis
Data analysis was performed using IBM SPSS Statistics ver. 26 (IBM Corp., USA). Descriptive statistics were used to summarize baseline characteristics. Categorical variables were reported as frequencies and percentages, while continuous variables were presented as medians with interquartile ranges (IQRs).
Comparisons between the 2 groups were conducted using the chi-square test or Fisher exact test for categorical variables and the Mann-Whitney U test for nonnormally distributed continuous variables. A P value of <0.05 was considered statistically significant.
To determine the optimal timing for surgical intervention in cases likely to fail conservative treatment, time-to-event analysis using the Kaplan-Meier curves was performed using IBM SPSS Statistics ver. 26 and MedCalc ver. 20.0.4 (MedCalc Software Ltd., Belgium).
Results
1. Participant characteristics
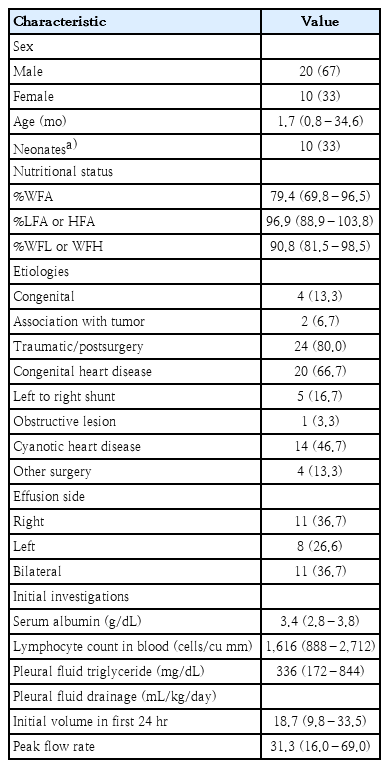
A total of 30 patients diagnosed with chylothorax were included in the present study, of whom 20 (67%) were male. The median age was 1.7 months (IQR, 0.8–34.6 months). Postsurgical chylothorax was the primary etiology, accounting for 24 of 30 cases (80%). Among these, 20 patients underwent cardiac surgery for congenital heart diseases, while the remaining 4 cases involved diaphragmatic plication, tracheoesophageal fistula repair, catheterization for cerebral glue embolization, and open thoracic extracorporeal membrane oxygenation cannulation.
At diagnosis, pleural fluid mostly exhibited a milky, turbid appearance, with a median triglyceride level of 336 mg/dL (IQR, 172–844 mg/dL). The median volume of initial pleural fluid drained in the first 24 hours was 18.7 mL/kg/day, and the median peak flow rate was 31.3 mL/kg/day. Baseline characteristics and laboratory findings are presented in Table 1.
2. Treatment outcomes
The overall success rate of conservative treatment in pediatric chylothorax in this study was 83.3%. Twenty-five of the 30 patients recovered with conservative treatment and were able to resume a normal diet without recurrence of chylous pleural effusion.
Among the 5 patients who did not respond to conservative treatment, 4 underwent surgical or interventional procedures. The first received lymphatic duct ligation, the second underwent lymphatic embolization, and the third had both lymphatic duct ligation and lymphatic embolization. All 3 achieved successful outcomes. However, the fourth patient underwent lymphatic ligation 3 times but ultimately died of severe sepsis. The intervals from the initiation of conservative management to surgery for these 4 patients were 41, 25, 113, and 35 days, respectively. The fifth patient died of severe sepsis after 34 days of conservative treatment without receiving any surgical or interventional procedure. Treatment outcomes are summarized in Fig. 1.
Summary of outcomes of 30 pediatric patients with chylothorax stratified by etiology and management strategy. Data are reported as number (percentage). MCT, medium-chain triglyceride; NPO, nil per os; TPN, total parenteral nutrition.
Subgroup analysis focused on 20 postcardiac surgery cases for congenital heart disease. Among these, one patient required surgical intervention after conservative treatment failed. As a result, the success rate of conservative treatment for postsurgical chylothorax following congenital heart surgery was 95% (19 of 20).
In the successful conservative treatment group, the median duration of intercostal drainage indwelling was 15.5 days (IQR, 8.7–25.5 days). The median duration from initiation of conservative treatment to resumption of a normal diet without recurrence was 35.8 days (range, 29–51 days).
3. Factors associated with successful conservative treatment
Factors associated with successful conservative treatment were analyzed by comparing 25 patients in the successful group and 5 in the unsuccessful group (Table 2). Two significant factors were identified: the etiology of chylothorax and the peak flow rate of pleural fluid drainage. Postsurgical chylothorax had a significantly higher success rate than nonsurgical causes (22 of 24 [91.7 %] vs. 3 of 6 [50%], P=0.04), and the peak flow rate was significantly lower in the successful treatment group (26.8 mL/kg/day vs. 91 mL/kg/day, P=0.002).
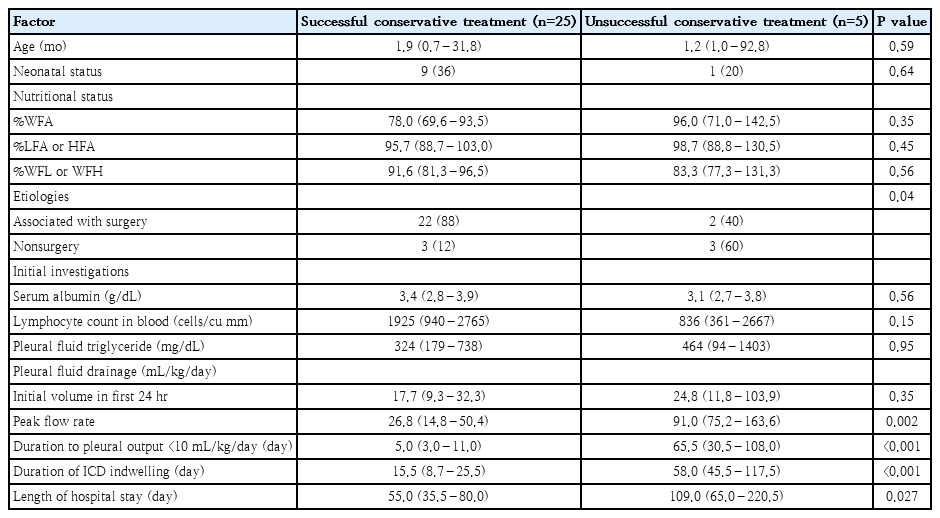
Characteristics of successful versus unsuccessful conservative treatment groups of pediatric patients with chylothorax
Although higher ALC in the blood and lower initial pleural fluid drainage volumes were observed in the successful group, these differences were not statistically significant. The median length of hospital stay was significantly shorter in the successful conservative treatment group (55.0 days; IQR, 35.5–80.0 days) compared to the unsuccessful group (109.0 days; IQR, 65.0–220.5 days; P=0.027).
A secondary analysis was conducted to compare chylous drainage between the 2 etiologic groups—postsurgical and nonsurgical chylothorax. Despite the higher success rate in the postsurgical group, there were no significant differences in median initial drainage volume (23.1 mL/kg/day [IQR, 11.8–34.0 mL/kg/day] vs. 14.1 mL/kg/day [IQR, 6.1–29.2 mL/kg/day], P=0.32) or median peak flow rate (27.4 mL/kg/day [IQR, 16.0–61.8 mL/kg/day] vs. 43.8 mL/kg/day [IQR, 12.1–114.1 mL/kg/day], P=0.70). To further evaluate the severity of chyle output, the incidence of high-output chylothorax was assessed using 2 peak pleural fluid flow rate thresholds: >20 mL/kg/day and >100 mL/kg/day. The proportion of patients with drainage exceeding 20 mL/kg/day was comparable between groups (15 of 24 [62.5%] postsurgical vs. 4 of 6 [66.7%] nonsurgical, P=1.00). Similarly, extremely high-output chylothorax (>100 mL/kg/day) was observed in 3 of 24 (12.5%) and 1 of 6 (16.7%) patients, respectively (P=1.00).
4. Time to response in conservative treatment
Among the 25 patients in the successful conservative treatment group, the median time to achieve a response—defined as pleural fluid drainage of less than 10 mL/kg/day—was 5 days (range, 1–23 days). In contrast, the 5 patients in the unsuccessful group had a significantly longer median time to response of 65.5 days (range, 25–116 days; P<0.001) (Table 2).
Fig. 2 illustrates the daily chest tube drainage of each patient. A trend toward reduced chyle output emerged by the second week, with most patients achieving successful conservative treatment within 2–3 weeks. In contrast, those in the unsuccessful group rarely demonstrated drainage below 10 mL/kg/day and often exhibited fluctuating chyle output.
Daily chest tube drainage volumes for each patient from day 1 to day 45 following the diagnosis of chylothorax and initiation of conservative management. (A) All pediatric patients with chylothorax (n=30). (B) Patients in whom conservative treatment was successful (n=25). (C) Patients in whom conservative treatment was unsuccessful (n=5).
Excluding one patient who died before undergoing a surgical or interventional procedure, a Kaplan-Meier time-to-event analysis was conducted on 29 patients to determine the optimal duration of conservative treatment before considering surgical intervention. The overall median time to response was 7 days (95% confidence interval, 3–12). Fig. 3 presents the cumulative percentage of patients achieving a response over time, stratified by etiology of chylothorax. The success rates of conservative treatment for postsurgical chylothorax were 78% at 14 days and 91% at 21 days, whereas for nonsurgical chylothorax, the success rate was 50% at 14 days. The log-rank test demonstrated a trend toward a difference between the 2 groups (P=0.06).
Kaplan-Meier curve comparing the cumulative success rate of conservative treatment over time of patients with postsurgical chylothorax (solid line) versus nonsurgical chylothorax (dashed line). The x-axis represents time (in days), while the y-axis indicates the cumulative success rate of patients with <10 mL/kg/day of pleural fluid drainage.
Discussion
The present study reviewed 30 pediatric patients diagnosed with chylothorax, the majority of which occurred postoperatively, primarily following congenital heart disease surgery. The findings demonstrate that conservative treatment is highly effective as a first-line approach, with a success rate of 83.3%. Factors significantly associated with successful conservative management included postsurgical etiology and a lower peak pleural fluid drainage rate. Additionally, a 14-day threshold emerged as an appropriate duration for considering surgical or interventional procedures if pleural fluid drainage remains above 10 mL/kg/day following the initiation of conservative treatment.
The high success rates of conservative treatment observed in this study—83.3% overall and 95% in postcardiac surgery cases—are consistent with findings from previous research, which reported success rates ranging from 80% to 95% [3-7]. This underscores the efficacy of conservative treatment as the initial approach for managing pediatric chylothorax. A prior study at Siriraj Hospital, conducted between 1997 and 2003, reported a higher overall success rate of 87% for conservative treatment in pediatric patients with chylothorax and chylopericardium [5]. The higher success rate in the previous study may be attributed to differences in etiology, as most cases (15 of 16, 94%) were secondary to cardiothoracic surgery, compared to 80% in the present study.
Comparison between groups revealed that, in addition to postsurgical etiology, a lower peak pleural fluid drainage rate was significantly associated with conservative treatment success. Patients in the unsuccessful conservative treatment group exhibited a significantly higher peak pleural fluid flow rate than those in the successful group. This finding aligns with previous research on both pediatric and adult chylothorax cases [3,8,14,15]. The correlation between high pleural fluid flow rates and the failure of conservative treatment may reflect a large leakage site or high pressure in the lymphatic duct, which reduces the likelihood of spontaneous self-repair.
Marts et al. [8] reported that the lower serum albumin levels were associated with surgical treatment. In contrast, the present study found no significant association between serum albumin level at diagnosis and treatment outcome. This discrepancy may be due to differences in timing: our study assessed albumin at diagnosis, whereas Marts et al. [8] reported the lowest albumin levels during the treatment course.
Although the differences were not statistically significant, the successful conservative treatment group had higher ALC and lower initial 24-hour pleural fluid drainage volumes. These trends may reflect smaller chyle leaks and better immune-nutritional status. A low ALC or high initial drainage volume may serve as early indicators of conservative treatment failure. Further studies with larger cohorts are warranted to define clinically relevant cut-off values for these variables, which could help guide early decision-making.
Various indications for surgical or interventional treatment have been proposed, including chyle production exceeding 100 mL/kg/day or 100 mL/yr of age for 5 days, persistent chyle drainage of >100 mL/day for more than 2 weeks or >10 mL/kg/day after 1 week of conservative management, unchanged drainage output for 1–2 weeks, and chylothorax persisting after 2–4 weeks of medical management [1,11,16].
In this study, a time-to-event analysis was performed to determine the optimal duration of conservative treatment before considering surgical intervention. The cumulative treatment success curve over time indicated that the likelihood of successful conservative treatment decreases as time progresses. Among patients with successful conservative treatment, the median time to achieve a response was 5 days. Remarkably, postsurgical chylothorax had a success rate of 78% at 14 days. Based on these findings, we suggest that surgical intervention should be considered if pleural fluid drainage remains ≥10 mL/kg/day after 14 days of optimal conservative treatment. This proposed threshold offers a practical tool to identify patients at risk of conservative treatment failure. Early identification allows timely intervention, potentially reducing complications, shortening hospital stays, and improving overall outcomes.
Due to the relative rarity of the disease and the retrospective nature of this study, several limitations should be noted. First, the small sample size limited the scope of data analysis. Second, because lipoprotein analysis−considered the gold standard for diagnosing chylothorax−was unavailable at our institution, the diagnostic criteria in our study were based on the clinical context (e.g., recent cardiothoracic surgery or suspected lymphatic injury or disruption), as well as pleural fluid characteristics and biochemical profiles consistent with previous clinical studies and established diagnostic practices in resource-limited settings. Finally, the absence of some potentially relevant data, such as central venous pressure and right-sided heart pressure, limited the ability to explore their associations with treatment outcomes.
In conclusion, conservative treatment remains a highly effective first-line approach for managing pediatric chylothorax, particularly in cases involving postcardiac surgery for congenital heart disease. A surgically related etiology and lower peak pleural fluid flow rate were significantly associated with successful conservative management. Determining the optimal timing for surgical or interventional procedures is essential to minimizing complications and improving clinical outcomes.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
We would like to express our gratitude to Miss Nerisa Thornsri and Dr. Saowalak Hunnangkul of the Department of Research and Development, Faculty of Medicine Siriraj Hospital, for their valuable assistance with the statistical analysis in this study.
Author contribution
Conceptualization: PK, ND, SK, PS; Data curation: PK, PS; Formal analysis: PK, PS; Methodology: PK, ND, SK, PS; Project administration: PK, PS; Visualization: ND, SK, PS; Writing – original draft: PK; Writing – review & editing: ND, PS