Serological investigation of Ureaplasma urealyticum in Korean preterm infants
Article information
Abstract
Purpose
Ureaplasma colonization is related with perinatal complications in preterm infants. Little is known about the difference in virulence among various Ureaplasma urealyticum serovars. The aim of this study was to determine U. urealyticum serovars of preterm infants in order to assess whether any of the serovars were associated with bronchopulmonary dysplasia (BPD).
Methods
Three hundred forty-four preterm infants with a gestational age less than 34 weeks admitted to Gangnam Severance Hospital neonatal intensive care unit from July 2011 to December 2012 were included in this study. Tracheal and gastric aspirations were conducted on infants to confirm Ureaplasma colonization. Ureaplasma colonization was confirmed in 9% of infants, of these, serovars were determined by real-time polymerase chain reaction.
Results
A total of 31 infants (gestational age, 29.3±3.1 weeks; birth weight, 1,170±790 g) were U. urealyticum positive. The Ureaplasma positive group treated for more days with oxygen and ventilation than the negative group (P<0.05). Histologic chorioamnionitis and moderate to severe BPD were more frequent in the Ureaplasma positive group than in the negative group (P<0.05). U. urealyticum isolates were either found to be a mixture of multiple serovars (32%), serovar 9 alone or combined with other serovars (39%), serovar 11 (26%), 2 (13%), 8 (10%), 10 (13%), and 13 (25%). No individual serovars were significantly associated with moderate to severe BPD and chorioamnionitis.
Conclusion
This is the first study to describe the distribution of U. urealyticum serovars from Korean preterm infants. Ureaplasma-colonized infants showed higher incidence of BPD and chorioamnionitis.
Introduction
Ureaplasma colonization has been associated with pregnancy complications, neonatal morbidities, and perinatal death1). Vertical transmission rates have been documented at 45-66% in term infants and 58% in preterm infants; the lower the gestational age (GA), the higher the transmission rate2,3). Some reports have shown that Ureaplasma species not only colonize the respiratory tract but also invade the bloodstream and across the blood brain barrier in very low birth weight (BW) infants3,4). Ureaplasma infection is associated with bronchopulmonary dysplasia (BPD), intraventricular hemorrhage (IVH), respiratory distress syndrome (RDS), and pneumonia and increases the risk of developing BPD by 2.83-fold5).
Ureaplasma has 14 known serovars that are separated into Ureaplasma parvum (serovars 1, 3, 6, and 14) and U. urealyticum (serovars 2, 4, 5, and 7-13) biovars6). Controversy still remains regarding whether there are differences in virulence among the Ureaplasma serovars. It has been noted that some Ureaplasma serovars have a greater association with adverse pregnancy outcomes than others7,8). Some reports showed that Ureaplasma invasiveness is likely not limited to one or a few particular serotypes. U. urealyticum isolates are typically found as a mixture of multiple serovars. A recent report has suggested that serovar 11 alone or combined with other serovars is the most common serovar, and no individual species or serovars or serovar mixtures were associated with BPD1). It is possible that antigen variability and host factors may be important determinants for Ureaplasma infections rather than different serotypes; however further investigation is still needed. Moreover, there are no surveys regarding the serovars in Korean preterm infants.
The aim of this study was to determine the distribution of Ureaplasma serovars in preterm infants in a prospective cohort and to assess whether any of the serovars are related to BPD.
Materials and methods
1. Study design
In prospective study, preterm infants without congenital anomaly, below the GA of 34 weeks that were admitted to the neonatal intensive care unit at the Gangnam Severance Hospital between July 2011 and December 2012 were enrolled. For 301 intubated infants, both tracheal and gastric aspirates were obtained for Ureaplasma culture and polymerase chain reaction (PCR) at birth within 24 hours of age, however, only gastric aspirates were obtained for 33 nonintubated infants. Sterile saline (0.5 mL) was instilled in the endotracheal tube and immediately aspirated back into the suction trap, and the process was repeated. The institutional review board of Gangnam Severance Hospital approved this study.
2. Sample collection and real-time PCR
Specimens were vortexed and 0.2 mL of each specimen was added to 1.8 mL of prepared 10B broth9). Tubes were incubated at 37℃ and if a color change occurred, 0.2 mL of inoculum was plated onto A8 agar (Northeast Laboratory, Waterville, ME, USA). A positive culture was defined as a positive broth test confirmed by typical colony morphology on A8 agar. All remaining original samples and positive isolates were aliquoted and stored at -80℃ for further DNA extraction and amplification. DNA was extracted using the QiAmp DNA Blood Mini kit (Qiagen, Valencia, CA, USA) according to the manufacturer's protocol. To differentiate U. urealyticum serovars, the DNA was analyzed by multiplex real-time PCR using the Roche LightCycler 2.0 as previously described10). Each primer or probe set was confirmed to amplify only the designated serovar and none of the other 13 serovars when the optimized PCR conditions were used as described previously10). All primers were synthesized by Invitrogen (Carlsbad, CA, USA) and probes were manufactured by Roche Diagnostics (Indianapolis, IN,USA).
3. Clinical outcomes
As for comorbidities, RDS (defined by therapeutic surfactant treatment), patent ductus arteriosus (PDA), BPD (by National Institute of Health classification), necrotizing enterocolitis (NEC included by above stage II according to the modified Bell's staging criteria), IVH (included higher than grade 2 confirmed by brain ultrasonography or brain magnetic resonance imaging [MRI]), periventricular leukomalacia (PVL confirmed by brain MRI), retinopathy of prematurity (ROP included above stge II ROPclassified according to the International Classification of Acute Retinopathy of Prematurity) were analyzed. Histologic chorioamnionitis was diagnosed as invasion of 5 more than polymorphonuclear cells at amnion, chorio-decidua, umbilical cord or chorionic plate by pathologist. Other clinical variables included duration of ventilator and oxygen support, duration of hospitalization, occurrence of preterm premature rupture of the membrane (defined by above 18 hours), and demographic variables.
Statistical analyses were conducted with the Student t test and chi-square analysis for means and frequencies. Numeric data are presented as the mean and standard deviation as the data were normally distributed. The Fisher exact test was used to compare categorical variables. Univariate odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for the association of Ureaplasma species with BPD outcome. Calculations were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). A P value less than 0.05 was considered statistically significant.
Results
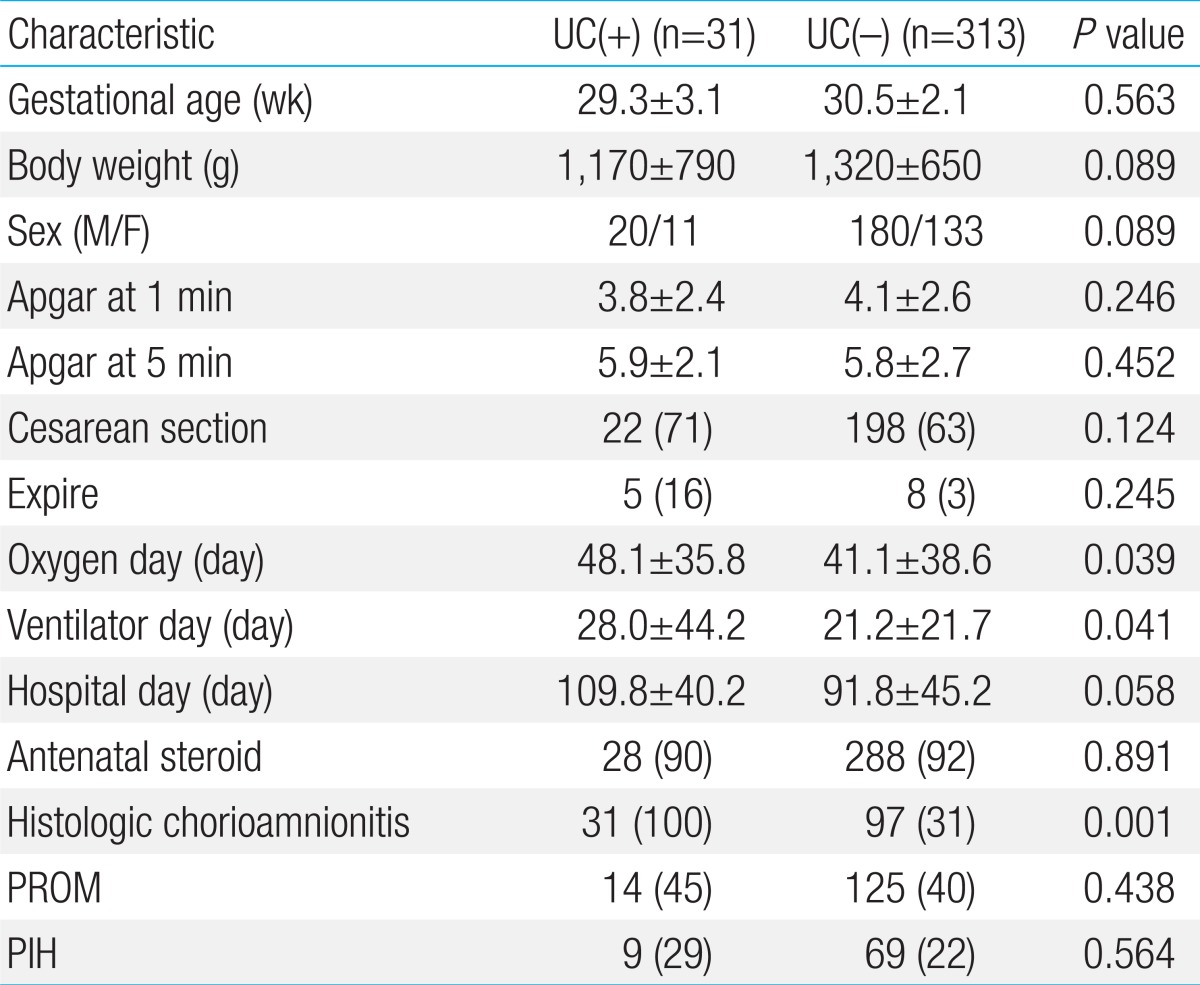
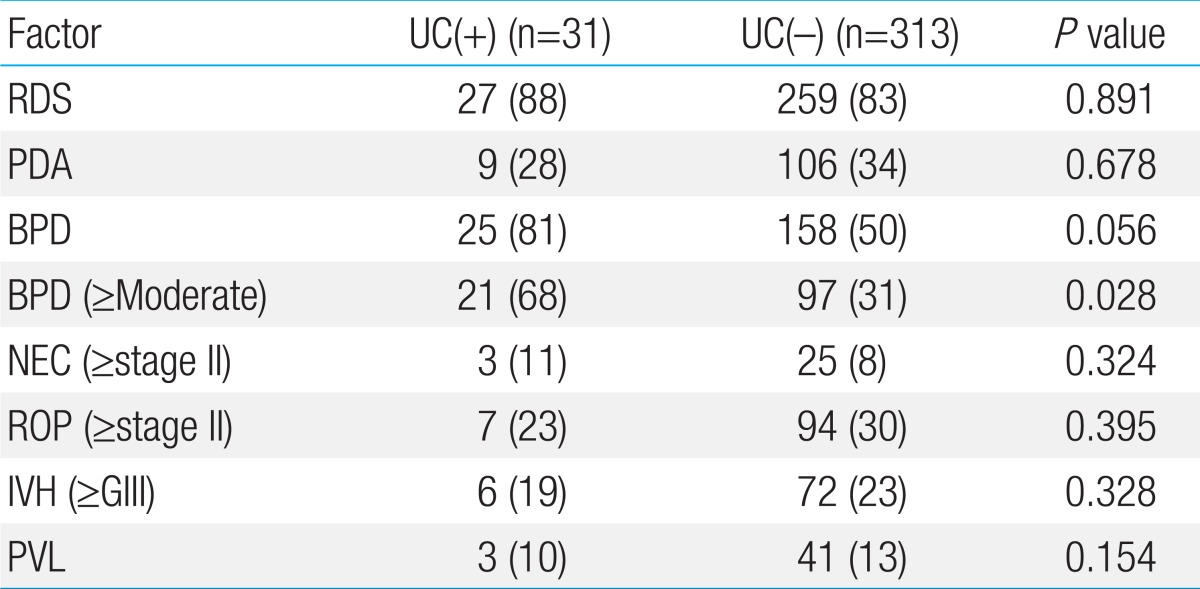
A total of 344 preterm infants less than 34 weeks gestation were enrolled and all endotracheal and gastric aspirates were analyzed by culture and PCR. Thirty one (9%) preterm infants (GA, 29.3±3.1 weeks; BW, 1,170±790 g) were positive for Ureaplasma cultures, and 313 preterm infants (GA, 30.5±2.1 weeks; BW, 1,320±650 g) were negative. There was no significant difference of gestation and BW between the two groups. Ureaplasma culture-positive (UC(+)) infants were under more days of oxygen and ventilator treatment than Ureaplasma culture-negative (UC(-)) infants (P<0.05) Histologic chorioamnionitis was confirmed more frequently in the UC(+) group than in the UC(-) group (100% vs. 31%, P=0.001) (Table 1). The incidence of common neonatal illnesses such as RDS, PDA, NEC, ROP, IVH, and PVL were not significantly different between the two groups. Moderate to severe BPD occurred more frequently in the UC(+) group than in the UC(-) group (68% vs. 31%, P=0.028) (Table 2).
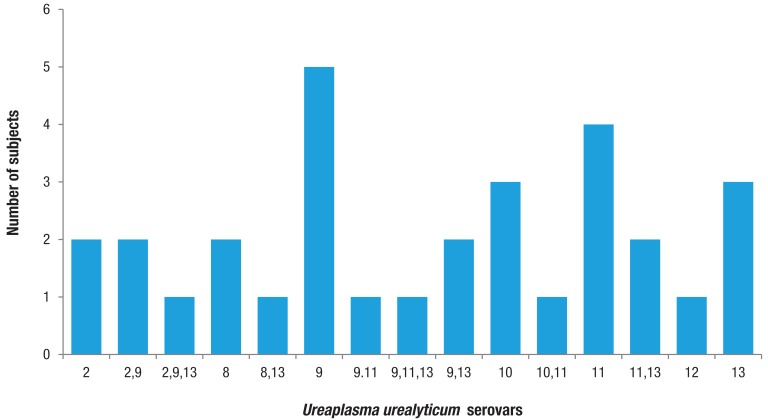
Serovar genotyping was performed from 31 of the UC(+) subjects. Ureaplasma colonization was detected inversely relative to the GA (OR, 0.65; 95% CI, 0.510 to 0.905, P=0.045). As shown in Fig. 1. U. urealyticum isolates were commonly detected as a mixture of multiple serovars (32%), with serovar 9 alone or combined with other serovars (39%) being the most common isolates, followed by serovar 11 (26%), 2 (13%), 8 (10%), 10 (13%), and 13 (25%). We analyzed the correlation of Ureaplasma colonization with pulmonary outcome. No individual serovars or serovar mixtures were significantly associated with moderate to severe BPD or chorioamnionitis.
Discussion
Recent studies have reported significant evidence that Ureaplasma infection may induce inflammatory processes early in utero and can lead to chorioamnionitis, lung injury including BPD, and other postnatal neonatal morbidities11-13). However, not much is known about the influence of Ureaplasma virulence factors, host immune factors, inflammatory variability, and interactions with environmental factors in the development of Ureaplasma-associated neonatal morbidities. This is the first study to investigate the association between Ureaplasma serovars and BPD in Korean preterm infants.
Ureaplasma spp. are the most frequently isolated microorganisms inside the amniotic cavity during pregnancy, and vertical transmission in up to 50% of preterm infants and 22-55% of term infants has been noted2,3,14). Infection of the infant with Ureaplasma spp. may occur in utero or perinatally and has been related with an increased risk of chorioamnionitis, abortion, stillbirth, premature birth, perinatal morbidity, pneumonia, bacteremia, and meningitis. In a prospective cohort, 23% of preterm infants with Ureaplasma respiratory colonization and 28% of infants with invasive Ureaplasma detected in the blood or cerebrospinal fluid were reported3). In another study, 78% of placentas from infants with Ureaplasma respiratory tract colonization showed evidence of histologic chorioamnionitis, in contrast to 36% of culture-negative infants1). In this study, 9% of preterm infants were confirmed with Ureaplasma respiratory colonization, and their entire placenta showed histologic chorioamnionitis.
Respiratory morbidities are significantly higher in infants with cultured Ureaplasma . Higher mortality due to respiratory complications was found to be significant in colonized infants and the risk of a combined outcome measure of BPD or death due to lung disease was 4.2-fold higher in the colonized than in the uncolonized very low birth weight infants15,16). Among the infants treated with mechanically applied ventilation, those with positive tracheal aspirate cultures had a 7.9-fold increased risk to develop moderate-to-severe BPD than those with a positive nasopharyngeal sample alone (OR, 7.86; 95% CI, 1.31 to 47)17). In this study, moderate to severe BPD occurred more frequently in the Ureaplasma positive group. Perinatal Ureaplasma infection may contribute to inflammation of the lung and disruption of alveolar development directly or via oxidant and ventilator-induced lung injury18,19). Therefore, the postnatal application of high oxygen concentrations and mechanical ventilation and the duration of exposure may potentiate the effects of Ureaplasma-associated injury to the lungs1).
Recently, Ureaplasma was divided into 2 species and 14 serovars. U. parvum, known as biovar 1, comprises serovars 1, 3, 6, and 14, and U. urealyticum (biovar 2) comprises the remaining serovars 2, 4, 5, and 7-13. Ureaplasma is characterized as lacking a cell wall, has limited biosynthetic abilities, has a small genome size, and has a mucosal association in the human host1). In advance of the genomic sequence information for all 14 Ureaplasma serovars, a multiplex real-time PCR assay for the rapid detection and discrimination of the two Ureaplasma biovars that targeted two conserved gene sequences in U. parvum or U. urealyticum was available. Compared to culture and traditional PCR, real-time PCR is suggested to be the most sensitive detection method for Ureaplasma species10,20). In this study, Ureaplasma serotyping was done by real-time PCR using serovar specific primers and probes.
Controversy remains as to whether there are differences in virulence among the 14 serovars and 2 biovars. For instance, recurrent abortions occurred 4 times more frequently in woman infected with serovar 4 compared with controls7). In addition, a report showed that pregnancy loss in mothers increased with a history of mean antibody titers for serovars 6 and 8 relative to mothers with elevated mean titers to serovars 4 and 821). Furthermore, some reports have suggested no difference in BPD rates between infants colonized with either biovar, but a higher rate of BPD in infants positive for both biovars8). In another report, a 2-fold higher rate of BPD was reported for U. urealyticum-colonized infants than the rate for U. parvum-colonized infants8). Serologic responses were assessed in preterm infants with respiratory disease22). Elevation of titers to serovars 4, 7, and 8 was shown in infants with lung disease. In respiratory complications, the mean titers of serovars 4 and 8 were higher in nonsurvivors than in survivors, whereas titers to serovar 5 were elevated in survivors. In another study, the most common serovars alone and in combination with other serovars were U. parvum serovars 3 and 6 and U. urealyticum serovar 11. Interestingly, serovars 4 and 5 were not detected in any sample17). No correlation was found between BPD severity according to the serovars. In our study, U. urealyticum isolates were commonly found as a mixture of multiple serovars, and serovar 9 alone or combined was the most common serovar. However, there was no significant association between any individual or combination of serovars and the occurrence of BPD.
This result is similar to reports that have shown that Ureaplasma virulence is independent of the serovars in regard to the development of BPD. Due to a small sample size and the limitation that we only identified Ureaplasma urealyticum in this study, we are not able to validate the real effects of virulence factors on clinical severity. Further only gastric culture for U. urealyticum were checked for nonintubated infants.
In conclusion, this is the first study to investigate the distribution of U. urealyticum serovars in tracheal aspirates of Korean preterm infants using serovar-specific real-time PCR. Ureaplasma colonized infants showed a higher incidence of BPD and chorioamnionitis. However, none of the serovars were strongly associated with the occurrence of BPD in this limited study. Further studies to identify targets that prevent the adverse effects of Ureaplasma infection in the immature lung are needed.
Acknowledgments
A grant from The Korean Pediatric Society, Kuhnil Fund (2011) supported this work.
Notes
No potential conflict of interest relevant to this article was reported.