Kikuchi-Fujimoto disease mimicking malignant lymphoma with 2-[18F]fluoro-2-deoxy-D-glucose PET/CT in children
Article information
Abstract
Purpose
Kikuchi-Fujimoto disease (KFD) is a benign disease, which is characterized by a cervical lymphadenopathy with fever, and it often mimics malignant lymphoma (ML). 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography (18F-FDG PET/CT) is a powerful imaging modality for the diagnosis, staging and monitoring of ML, with the limitations including the nonspecific FDG uptake in infectious or inflammatory processes. This study compared clinical manifestations and PET/CT findings between KFD and ML patients.
Methods
We retrospectively reviewed the medical records of 23 patients with KFD and 33 patients with ML, diagnosed histopathologically, between January 2000 and May 2013 at the Department of Pediatrics, Yeungnam University Medical Center. Among them, we analyzed the clinical manifestations, laboratory findings and characteristics, and the amount of 18F-FDG uptake between 8 KFD and 9 ML patients who had 18F-FDG PET/CT.
Results
The 18F-FDG PET/CT maximum standardized uptake values (SUVmax) ranged from 8.3 to 22.5 (mean, 12.0) in KFDs, and from 5.8 to 34.3 (mean, 15.9) in MLs. There were no significant differences in SUVmax between KFDs and MLs. 18F-FDG PET/CT with ML patients showed hot uptakes in the extranodal organs, such as bone marrow, small bowel, thymus, kidney, orbit and pleura. However, none of the KFD cases showed extranodal uptake (P<0.001). 18F-FDG PET/CT findings of KFD with nodal involvement only were indistinguishable from those of ML.
Conclusion
Patients who had extranodal involvement on PET/CT were more likely to have malignancy than KFD.
Introduction
Kikuchi-Fujimoto disease (KFD), necrotizing histiocytic lymphadenitis is a rare disorder in children, but a self-limited and a benign disease that was described in 1972, simultaneously by Kikuchi1) and Fujimoto et al.2). It is usually seen among young women in Asia. KFD is characterized by regional lymphadenopathy, accompanied by prolonged fever. Weight loss and night sweats, the two systemic symptoms frequently seen in lymphoid malignancy are rare, but have been reported in KFD3). Despite the lack of consistent laboratory findings in KFD, many cases have been reported in association with leukopenia, anemia and elevated lactate dehydrogenase (LDH) levels3). The clinical and laboratory presentations are frequently confused with those of malignant lymphoma4,5,6).
Lymphoma is the third most common cancer in children. Imaging plays an important role in the noninvasive assessment of patients with lymphoma, with its main purpose being to provide the means for assessment of risk and response-adapted therapy7). Metabolic imaging with 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography (18F-FDG PET/CT) has emerged as a powerful imaging modality for the diagnosis, staging and monitoring of various cancers8,9). 18F-FDG PET/CT enables semiquantitative analysis of tumor metabolism, commonly measured as standardized uptake value (SUV). A number of studies suggest a role for SUV analysis in the definition of the PET-positive tumor volume. Hutchings et al.9) showed differences in mean maximum SUVs (SUVmax) between the different histopathological subtypes of Hodgkin's lymphoma. However, this modality also has limitations related to several factors, including the nonspecific 18F-FDG uptake in physiologic, infectious or inflammatory processes such as KFD7). Recently, one study showed that 18F-FDG PET/CT images with generalized distribution of small to medium sized lymph nodes with high 18F-FDG uptake are more suggesting KFD10).
Herein, we analyzed and compared the clinical manifestations, laboratory findings and characteristics, and the amount of 18F-FDG uptake between 8 KFD and 9 malignant lymphoma patients who had 18F-FDG PET/CT.
Materials and methods
1. Subjects
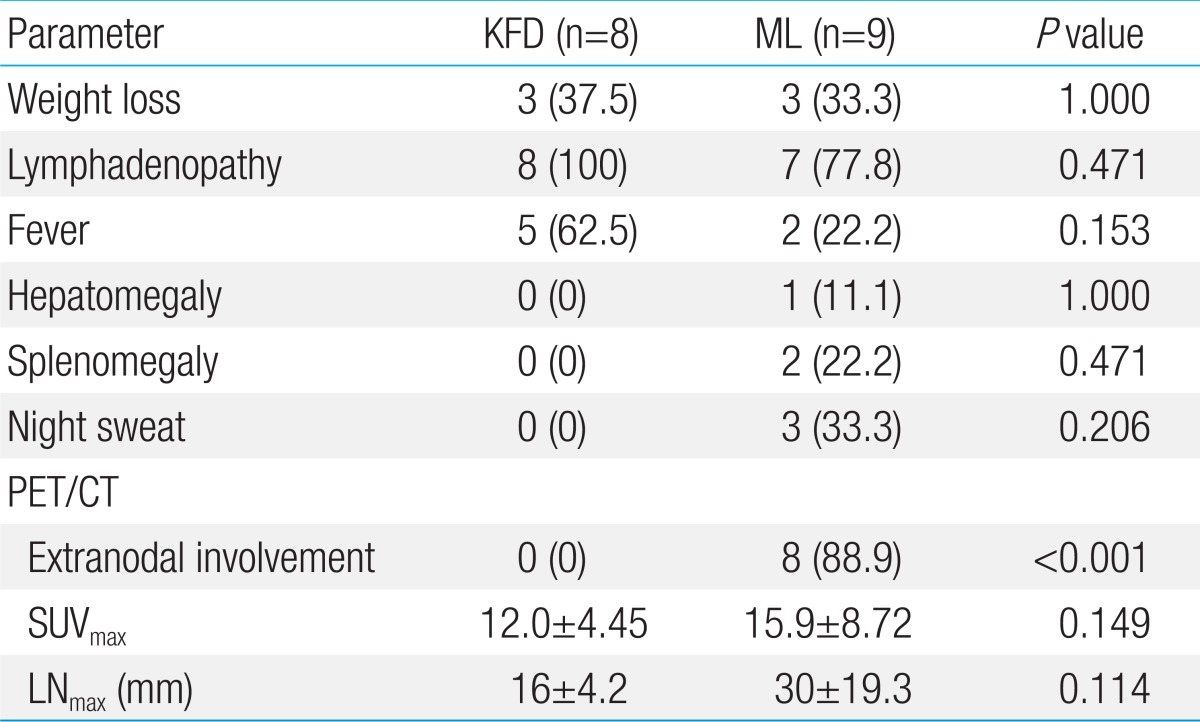
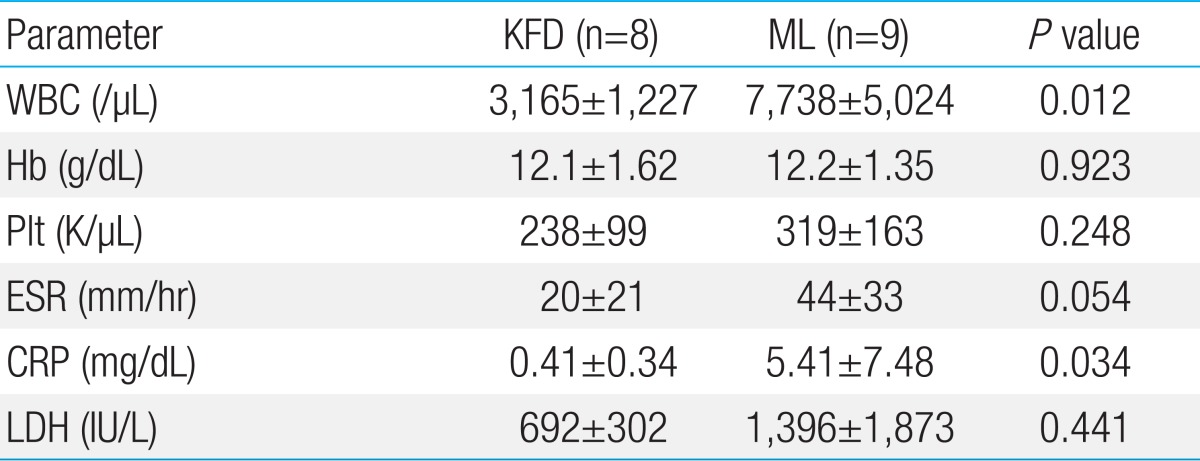
We retrospectively reviewed and analyzed the medical records and image findings of 23 patients histopathologically diagnosed with KFD and 33 patients with malignant lymphoma, between January 2000 and May 2013 at the Department of Pediatrics, Yeungnam University Medical Center. Eight of the 23 patients with KFD, who were strongly suspected to have malignant lymphoma from their clinical manifestations initially, had evaluated with 18F-FDG PET/CT for staging immediately. They were compared to the 9 patients with malignant lymphoma, who had same evaluations (Table 1).
Clinical presentations and laboratory findings of the patients with KFD or malignant lymphoma who had PET/CT
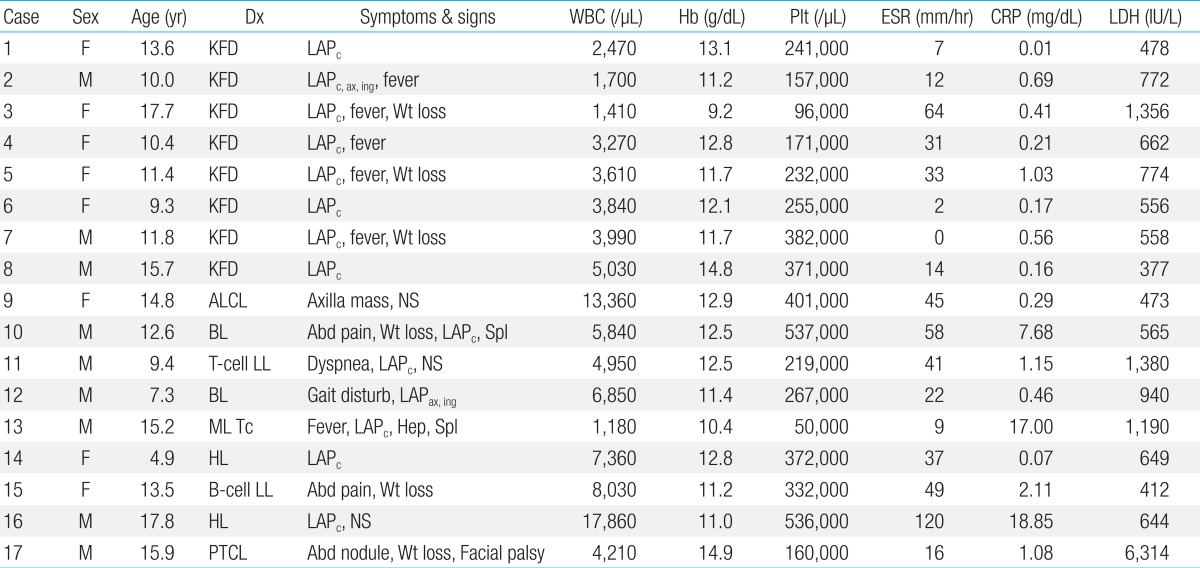
The final diagnosis was obtained from the biopsy specimen by one of three different pathologists. In KFD, the involved lymph nodes characteristically demonstrated a loss of nodal architecture and extensive fibrinoid necrosis with abundant karyorrhectic debris and absence of granuloma (Fig. 1).
(A) Low magnification shows necrotizing lesion in the subcapsular area (H&E, ×40). (B) Abundant karyorrhectic debris, fibrin deposits and histiocytes are present (H&E, ×200).
The number of cases with different subtypes of malignant lym-phoma included Hodgkin's lymphoma (n=2), Burkitt's lymphoma (n=2), lymphoblastic lymphoma (n=2), anaplastic large cell lymphoma (n=1), peripheral T-cell lymphoma (n=1) and T-cell lineage malignant lymphoma (n=1).
2. PET/CT imaging
Eight patients with KFD and 9 patients with malignant lymphoma underwent 18F-FDG PET/CT examination. Patients were prepared to fast for at least 6 hours and had a prescan blood glucose analysis to ensure the level was <200 mg/dL. Patients received an intravenous injection of about 3.7-5.2 MBq/kg of FDG and rested quietly for 60-120 minutes after the injection. Studies were performed using a VCT or DVCT PET/CT instruments (GE Medical Systems, Milwaukee, WI, USA). Then, patients had total-body acquisition. CT for attenuation correction and anatomical localization was acquired before a PET, with 100 mA/sec at 100 kV. All images were reconstructed with 3.75-mm slice thickness at 2.4-mm increments. After CT, a three-dimensional mode PET was performed, and iterative algorithms with two iterations and eight subsets were used for image reconstruction. The data were filtered (full width at half maximum, 5.0 mm) and corrected for scatter. Two experienced nuclear medicine physicians interpreted the images.
3. Statistical analysis
Clinical manifestations between Kikuchi and malignant lymphoma patients were analyzed by the Fisher exact test. Laboratory findings and 18F-FDG PET/CT findings were analyzed by the Mann-Whitney U test. Values of P<0.05 were considered as statistically significant, and analyses were performed using the PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA).
4. Ethics statement
Yeungnam University Medical Center Institutional Review Board approved this retrospective chart review clinical study (YUH-12-0486-D17). Due to the purely observational nature of the study, informed consent was not required.
Results
Patients diagnosed with KFD were aged between 6 to 17 years, with the mean age of 11.7 years (13 males, 10 females). 18F-FDG PET/CT images of 8 patients with KFD were available for evaluation (3 males, 5 females). Patients diagnosed with malignant lymphoma, who carried out 18F-FDG PET/CT, were aged between 4 to 17 years, with the mean age of 11.7 years (6 males, 3 females).
Five KFD cases had a prolonged fever with cervical lympha-denopathy. Three of our eight KFD patients were referred for cervical lymphadenopathy without a fever. Only case 2 had multiple lymphadenopathy, including cervical, inguinal, supraclavicular and axillary lymph nodes. No patient had hepatosplenomegaly or night sweating, although three patients had weight loss for several weeks (cases 3, 5, and 7). Laboratory findings revealed leucopenia with normal differential counts in seven cases. Case 3 had pancytopenia (white blood cell [WBC], 1,410/µL; hemoglobin, 9.2 g/dL; platelet, 96,000/µL). Bone marrow aspiration and biopsy of 4 cases (cases 1, 2, 3, and 5) showed normocellular marrow with no abnormal cells. The levels of LDH, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) were increased in six, three and two patients, respectively (Table 1).
In the malignant lymphoma group, three patients (cases 12, 13, and 15) had bone marrow involvement, but only one patient (case 13) showed pancytopenia. There were no significant differences between KFDs and malignant lymphomas in clinical manifestations, including weight loss, lymphadenopathy and fever. However, hepatomegaly, splenomegaly and night sweating were seen in only malignant lymphoma patients (in 1, 2, and 3 cases respectively) (Tables 1, 2).
Leucopenia was more frequently observed in KFDs (P=0.012). There were no significant differences in the levels of hemoglobin or platelet between the two groups. CRP and LDH levels were higher in malignant lymphoma group with statistical significance. Malignant lymphoma patients tended to have higher ESR level, although the difference was not statistically significant (Table 3).
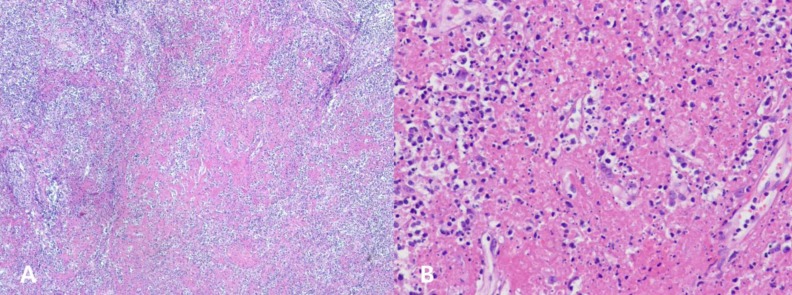
The 18F-FDG PET/CT SUVmax ranged from 8.3 to 22.5 (mean, 12.0) in KFDs, and from 5.8 to 34.3 (mean, 15.9) in malignant lymphomas (Tables 1, 2). There were no significant differences in SUVmax between KFDs and malignant lymphomas. 18F-FDG PET/CT detected generalized lymphadenopathies in five patients with KFDs (Fig. 2) which were not apparent on physical examination. Three patients had cervical lymphadenopathies only. Maximum diameters of involved lymph nodes on 18F-FDG PET/CT were ranged from 10 mm to 21 mm (mean, 16 mm) in KFDs, and from 12 mm to 67 mm (mean, 30 mm) in malignant lymphomas (Table 2). Larger lymph nodes were observed more frequently in the malignant lymphoma group with no statistically significant differences among the two groups (P=0.114).
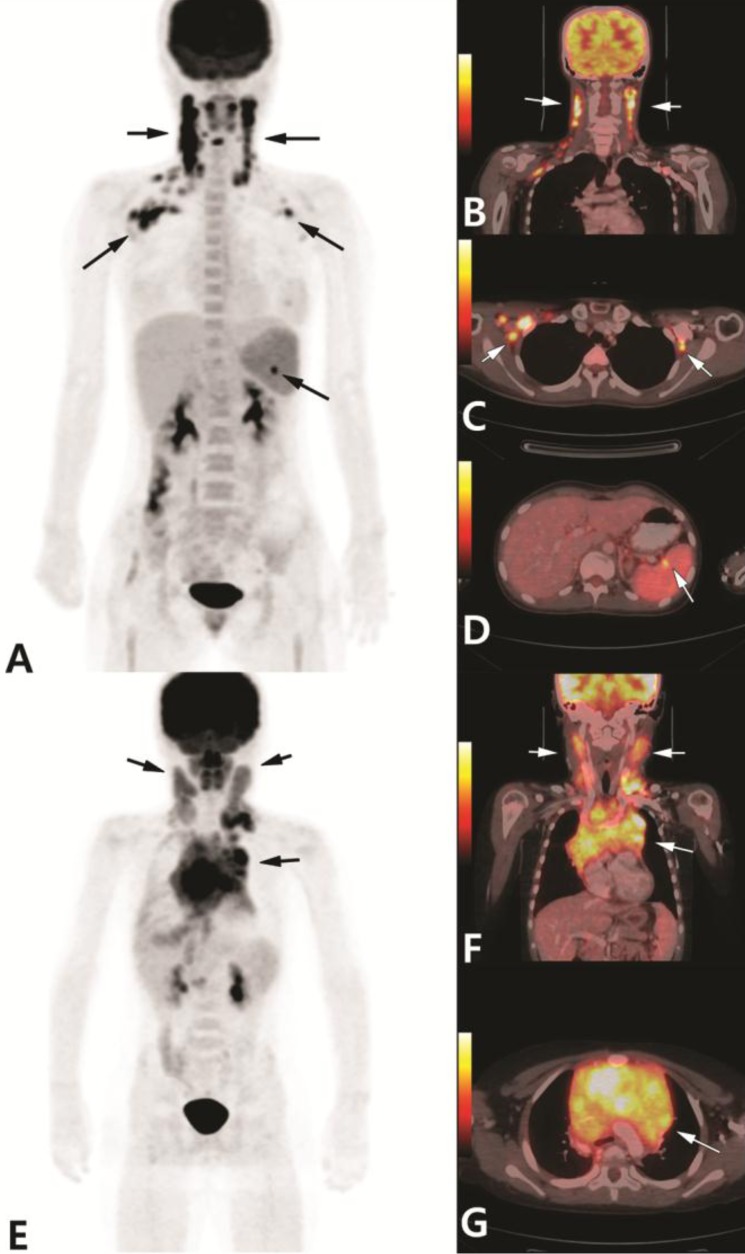
A 17-year-old girl with 2 weeks history of fever and neck masses who was referred for 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography-computed tomography (18F-FDG PET/CT) to evaluate lymphadenopathies. Anterior maximum intensity projection (MIP) image (A) and PET/CT fusion images (B-D) showed multiple hypermetabolic lymphadenopathies in both neck, both axilla and splenic hilum (arrows). Excisional biopsy of the right neck lymph node revealed Kikuchi-Fujimoto disease. MIP image also showed mild, homogeneous FDG uptake in bone marrow of vertebral bodies, both femurs and pelvic bone, which is due to reactive response. A 9-year-old boy with a week history of neck swelling was referred for FDG PET/CT. Anterior MIP image (E) and PET/CT fusion image (F,G) showed multiple hypermetabolic lymph nodes in both neck and intense FDG uptake in the anterior mediastinal mass (arrows). Histopathology of the left neck lymph node revealed T lymphoblastic leukemia/lymphoma.
The involvement of extranodal organs were observed only in malignant lymphomas (P<0.001) (Table 2). 18F-FDG PET/CT with malignant lymphoma patients showed hot uptakes in the extranodal organs, such as bone marrow, small bowel, thymus, kidney, orbit and pleura. Case 12 showed multiple hypermetabolic lymph nodes, anterior mediastinal mass and pleura (Fig. 2). However, none of the KFD cases showed extranodal uptake.
Discussion
KFD, subacute necrotizing histiocytic lymphadenitis, is known to have a worldwide distribution with a high prevalence among young women in Japan and other Asian countries, which is a rare but self-limited disorder. KFD has been increasingly reported in the literature, and its pathologic features and clinical presentations are well known. However, only a few pediatric cases have been reported4,5).
Cervical lymphadenopathy is present in 56% to 98% of cases, and prolonged fever in 30% to 50% of the cases; these are the most common manifestations of KFD3). Generalized lymphadenopathy has been reported rarely, and less common symptoms include weight loss, night sweats, and fatigue4). Leukopenia is frequently observed in 30% to 60% of the cases. Other findings include anemia, and elevated ESR, CRP, and LDH levels11). Excepting that patients showed generalized LAP more than cervical LAP only, other clinical and laboratory findings in our patients were similar to the previous reports. Kong reported that twenty-two patients (95%) with KFD showed generalized hypermetabolic lymph nodes with 18F-FDG PET/CT10).
Clinically and histologically, KFD can be misdiagnosed for lymphoid malignancy, systemic lupus erythematosus or infectious diseases. Due to the differences in management from KFD, these entities must be excluded before the diagnosis of KFD can be made3). Dorfman and Berry4) reported in 1988 that nearly 40% of patients with KFD had been initially misdiagnosed with malignant lymphoma. In our study, eight of the 23 KFD patients were initially suspected to have malignant lymphoma, as they showed massive cervical lymphadenopathy, prolonged fever, leukopenia or weight loss. 18F-FDG PET/CT findings were also mimicking malignant lymphoma. Thus, all the 8 cases had biopsies which showed typical findings of KFD without evidence of malignancy.
18F-FDG PET/CT is useful in diagnosis and follow-up of various malignant diseases8). However, FDG uptake is not specific for cancer. FDG avidity is due to increased glycolysis and glucose transporter activity. Thus, false-positive FDG uptake of 18F-FDG PET/CT scan for benign lesions are commonly encountered12,13,14). Therefore, it should be reminded for us that positive results should be interpreted with caution. Tsujikawa et al.15) reported the differences in PET/CT findings between KFD and malignant lymphoma. They reported KFD and aggressive non-Hodgkin's lymphoma (NHL) showed a significantly higher corrected SUV as compared with indolent NHL. And also, they indicated that PET/CT will be useful for making a distinction between KFD and malignant lymphoma, using both SUV and FDG uptake with partial volume correction. However, there are limitations of standardization and quantification with the 18F-FDG PET/CT scan14). Kong et al.10) reported that PET/CT images visualizing generalized distribution of relatively small sized lymph nodes with high FDG avidity are suggesting KFD but not crucial to the diagnosis of KFD.
In our study, patients with malignant lymphoma tended to present with extranodal involvement or huge conglomerated lymphadenopathies, in comparison with KFD patients who had generalized lymphadenopathy without extranodal involvement.
Thus, for the patients who show lymphadenopathies with extranodal involvement or huge conglomerated lymphadenopathies on 18F-FDG PET/CT, we suggest to prepare for chemotherapy with intravenous fluid hydration, urine alkalization and allopurinol while waiting for pathologic confirmation. For patients who show lymphadenopathies with only nodal involvement on 18F-FDG PET/CT, we suggest to wait for the confirmation of diagnosis with a pathologic examination. However, further study on a larger patient population is needed to validate our suggestion.
Notes
No potential conflict of interest relevant to this article was reported.