Ureaplasma urealyticum or Ureaplasma parvum: what's the difference?
Article information
Recently, birth of premature babies and low birth weight babies has been increasing and survival rate of very low birth weight babies even under 500 g not to mention under 1,000 g is remarkably enhanced thanks to the development of neonatology. With the enhanced birth rate and survival rate, the issue of pediatrics majoring in neonatology is not increasing survival rate anymore but making them healthier babies. While treating premature babies in the field, it is found that some premature babies have better prognoses while others have poor prognoses.
As a part of efforts to identify the factors influencing prognoses of newborns, studies on prenatal infections are actively made. One of the hottest topics is Ureaplasma infection. Although it has been studied before, it has been perceived as 'sexually-transmitted disease' and has been studied in gynecology or urology. Recently, however, it is expanded to the field of complications of premature babies1,2). Additionally, studies have been actively performed since strain known as Ureaplamsa urealyticum was segmented to Ureaplasma parvum (UPA hereunder) and Ureaplasma urealyticum (UUR hereunder), which were further segmented to 14 serovars2,3).
Past studies published before in Korea by Lim et al.4) and by Chang et al.5) were studies on overall prevalence before Ureaplasma colonization was segmented into two serovars. In this point, Eun et al.6) is encouraging because it studied serovars of Korean premature babies.
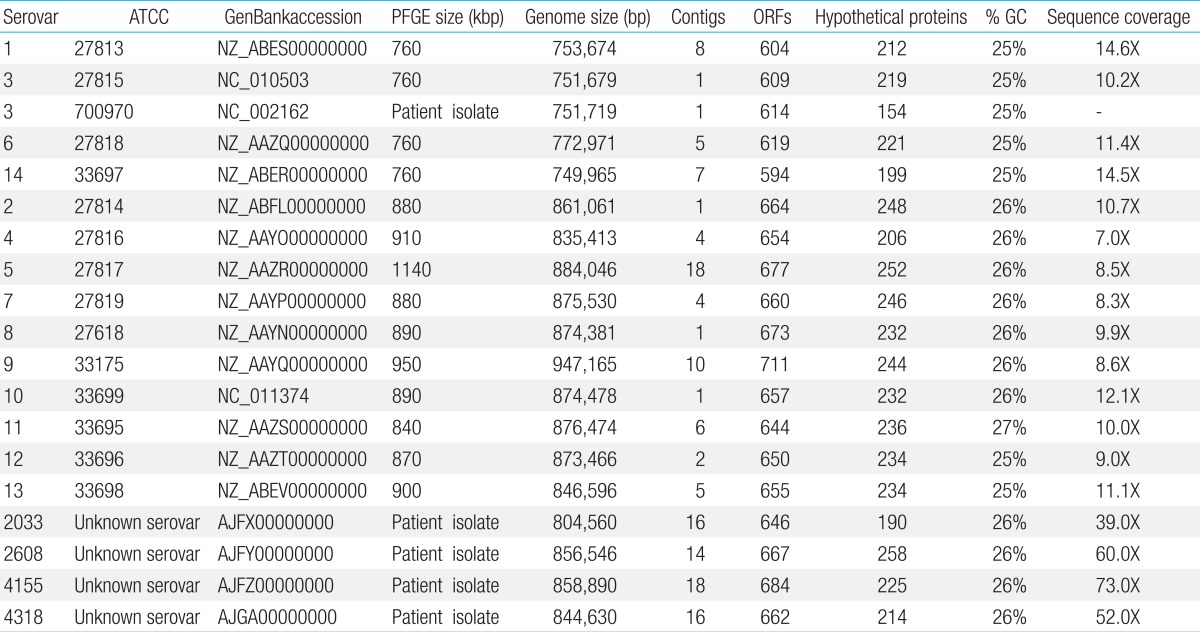
However, it has limitations at the same time. Although it is meaningful that it tried to analyze premature babies according to serovar, it dealt with UUR only and the conclusion that there would be no difference between Ureaplasma serovars may be misleading. As authors mentioned before, Ureaplasma spp is segmented to two biovars such as UPA and UUR. Such two biovars can be segmented according to genome size, 16S rRNA gene sequences, the 16S-23S rRNA intergenic region, enzyme polymorphisms, DNA-DNA hybridization, differential growth responses to manganese, and differences in the multiple banded antigen (mba) genes2,3). They are segmented to 14 serovars by polymerase chain reaction (PCR)-based methods based on the previously mentioned UPA (biovar 1, serovar 3, ATCC* 27815, NCTC** 11736), and UUA (biovar 2, serovar 8, ATCC* 27618, NCTC** 10177). According to characteristics of each serovar, serovar 1, 3, 6, and 14 fall under biovar 1, so to speak UPA, and rest of them fall under biovar 2, so to speak UUR. On the other hand strains that have not been clear in classification are more segmented and 5 more strains have been discovered7) (Table 1).
Accordingly, authors should discuss the difference between UPA and UUR serovars first to claim that there was no difference in bronchopulmonary dysplasia (BPD) incidence in each servoar. It seems misleading that they say there was no difference according to BPD and serovars because their study had very limited subjects and approximately 1/3 had mixed serovars. Additionally, some investigators consider these mixed strains as totally different serovars according to hybridization and wonder if studies investigating difference among serovars are meaningless8). Although it is one of major conclusions of Eun and et al.6) that there is no difference between UUR serovars, the conclusion is not well established and it is better to get to a conclusion after experiments using UPA and UUR together.
Ureaplasma is known as a strain difficult to culture in the laboratory because it is very small such as 15-25 micrometer diameter and has no cell wall. This strain produces adenosine triphosphate through urea hydrolysis and dissolves urea into ammonia (NH3) and carbon gas. When culturing in the laboratory, infection is judged through pH change in liquid culture using such principle. But recently, as studies have shown that PCR method is more sensitive, PCR method is preferred to classical culture1-3). To make more explanations on culture and PCR method, authors perform tracheal aspiration and gastric aspiration at the same time to identify correlations with BPD. As tracheal aspiration samples show whether there is lower respiratory colonization, which means infection in most cases, and may judge infection of Ureaplasma spp regardless of skills of testers, it is the most preferred method. However, it has a drawback that sampling can be made in newborns only with intubation. A probable alternative is nasopharyngeal swab. It is easy to get samples and can be repeated many times, although some authors said that we cannot judge infection only with the result of this test showing upper respiratory colonization1,2).
Interestingly, in Eun et al.6) study, UUR serovar 9 is found to be the most common serovar, which was deal with Koreans. Whereas Sung et al.9) studies on Caucasians and African-Americans found that serovar 11 was the most common. Such difference may imply difference between races, although it must be confirmed with further studies, because of small sample size of this study. In particular, as there have not been many studies regarding the difference between races, it will be an interesting field to perform a large-scale study including gene tests.
Many studies on relationship between Ureaplasma spp and complications of premature babies have been made recently and results are being published constantly. Among them, mechanism to make BPD by Ureaplasma spp. is considered as being made by activation of proinflammatory cytokines (tumor necrosis factor-α, interleukin [IL] 1β, IL-8) or blocking counterregulatory cytokines (IL-6, IL-10) rather than making direct damages on respiratory tract. There is a hypothesis that respiratory diseases and BPD of newborns are caused by phospholipase A2 created by other strains which coerces the creation of pulmonary surface activators. It is also know that infection in prenatal period stimulates infection consecutive infection of pulmonary alveoli, interferes the creation of pulmonary alveoli by directly or indirectly influencing respirator induced pulmonary damages, stimulates phagocytes composing cilliary disarray and clumping after composing colony on epithelial cells on respiratory tracts, and creates proinflammatory cytokine to cause BPD1,10,11). Such relationship with cytokines should be studied further in the future.
Conclusively, more studies are needed on the relationship between Ureaplasam and infection of newborns, in particular complications of premature babies including BPD. It is also needed to perform a large scale study on Korean newborns.
Notes
No potential conflict of interest relevant to this article was reported.