Lifestyle modifications in an adolescent dormitory: a clinical trial
Article information
Abstract
Purpose
Childhood obesity is an increasing public health issue worldwide. We examined dietary patterns among adolescents in a dormitory school, identified obese adolescents and tried to intervene to improve food habits and physical activity.
Methods
We conducted an experimental prospective longitudinal study based on 36 obese (body mass index [BMI]≥95th percentile) adolescents (aged 12-18 years) compared with controls (healthy children: normal age-appropriate BMI (BMI≤85th percentile). Six months' intervention included lifestyle-modification counseling (once a week by a clinical dietician), and an exercise regimen twice a week, 60 minutes each time, instructed by a professional pediatric trainer). Both groups underwent baseline measurements at the beginning of the study and 6 months later (arterial stiffness, blood pressure, pulse, weight and height, hemoglobin, creatinine, liver enzymes, highly sensitive C-reactive protein and complete lipid profile).
Results
Twenty-one participants completed the study. Low compliance from participants, school staff and parents was observed (participation in planned meetings; 71%-83%). BMI significantly decreased from 32.46±3.93 kg/m2 to 30.32±3.4 kg/m2 (P=0.002) in the study group. Arterial stiffness was not significantly different between the 2 groups and did not change significantly after 6 months' intervention (P=0.494). No significant changes in CRP and lipid profile were observed after the intervention.
Conclusion
Making lifestyle modifications among adolescents in a dormitory school is a complex task. Active intervention indeed ameliorates BMI parameters. However, in order to maximize the beneficial effects, a multidisciplinary well-trained team is needed, with emphasis on integrating parents and the school environment.
Introduction
Childhood obesity has been described as the primary childhood health problem in developed nations1), having been linked to many serious physical, social and psychological consequences. These include: an increased risk of cardiovascular dysfunction2), type 2 diabetes3), pulmonary4), hepatic5), renal6), and musculoskeletal7) complications; a lower health-related quality of life8); negative emotional states such as sadness, loneliness, and nervousness; an increased likelihood of engagement in high-risk behaviors9); and undesirable stereotyping including perceptions of poor health, academic and social ineptness, poor hygiene and laziness10).
While information on the dietary patterns of adolescents is limited in Israel, even less is known about the eating behaviors among adolescents from dormitory schools. It is important to intervene early because adolescence is an important developmental stage where behaviors can be influenced, setting the stage for lifelong habits. Eating patterns established early in life can persist11) and can have an impact on chronic diseases.
This study aimed to examine the dietary patterns among adolescents in a dormitory school, identify obese adolescents and try to intervene in order to modify their lifestyles.
Materials and methods
1. Study design: prospective longitudinal study
This was an experimental longitudinal study comparing healthy controls with adolescents (aged 12-18 years) recruited from "Ben Shemen" dormitory school. Children at "Ben-Shemen" dormitory school originate from a low socioeconomic background, and only leave for vacations every other weekend. The study was approved by the Institutional Ethical Review Committee and parental informed consent was obtained. A nutritionist checked the usual weekly food menu and the degree of physical activity at the dormitory school.
Obese male and female adolescents (BMI≥95th percentile) were included. The intervention included lifestyle-modification counseling, diet counseling once a week by a clinical dietician, and an exercise regimen twice a week, 60 minutes each time, instructed by a professional pediatric trainer. The diet counseling included a weekly group meeting for 1 hour. During the meetings several issues that can promote healthy lifestyles were discussed, like eating 5 servings of fruit and vegetables every day, eating skimmed dairy products, drinking water instead of soft drinks, and doing physical activity every day. The energy content of a healthy diet was in concordance with age and sex12). The intervention group was divided into 2 groups in order to make the meetings more personal. Observation of their activity was performed by young instructors and tutors aged 20-22 years.
The physical activity meetings were performed twice a week for 1 hour each, and were constructed by a professional Physical Activity Instructor for Children from Assaf Harofeh Medical Center. Those meetings included aerobic and anaerobic exercise like running, basketball and mattress exercises. The purpose of these meetings was to provide the participants with alternative options for physical activity after school hours. Only adolescents that participated in >70% of the meetings (physical activities and nutritionist counseling) were included in the study.
A control teenager group consisted of healthy adolescents with a BMI appropriate for their age (BMI of up to the 85th percentile).
Both groups underwent baseline blood pressure and arterial stiffness measurements (detailed below). Physical examination, and blood pressure, pulse, weight and height, hemoglobin, creatinine, liver enzymes, highly sensitive C-reactive protein and complete lipid profile measurements were conducted at the beginning of the study and after 6 months.
All measurements were performed between 6:30 PM and 8:30 AM, at least 10 hours following the last meal, sugar or coffee intake, and prior to the administration of any daily medications.
Assessment of arterial stiffness was performed, at baseline and 6 months later, by a noninvasive technique using the commercially-available SphygmoCor System (AtCor Medical Ltd., West Ryde, Australia) described elsewhere13). All the measurements were taken in the same sitting position, in a quiet, temperature-controlled room (23℃±1℃), after at least a 5-minute resting period.
2. Statistical analysis
Statistical analysis was performed with the IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA). Statistical significance was determined by a P value <0.05. Correlation between groups was examined by the Pearson test. The paired t test was used to compare anthropometric parameters, blood tests and measures of arterial stiffness before and after the intervention. The independent samples t test was used to compare the treatment and the control groups.
Results
The study group was divided into 2 groups: the intervention group and the control group. The intervention group (n=36) included 39% girls (n=14) and 61% boys (n=22) with a mean age of 15.17±1.74 years (range, 12-18 years), a mean body weight of 86.86±16.48 kg (range, 55-127 kg) and a mean BMI of 32.15±4.1 kg/m2 (range, 28.4-40 kg/m2). Twenty one participants were included in the final analysis.
The control group (n=8) included 2 healthy girls and 6 healthy boys with a mean age of 16±1.52 years (range, 12-18 years), a mean body weight of 64.4±10.4 kg (range, 49-75 kg) and a mean BMI of 21.4±2.1 kg/m2 (range, 18.5-25.5 kg/m2).
The participation in the planned meetings ranged from 71% to 83%, including sport activities with a personal trainer and participation in the individual meetings with the nutritionist.
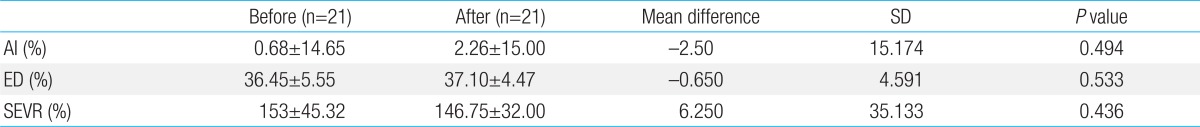
After 6 months, 100% of the control group and only 21 participants (58.3%) in the intervention group remained in the study. In the study group, BMI significantly decreased from 32.46±3.93 kg/m2 to 30.32±3.4 kg/m2 (P=0.002) as illustrated in Table 1. Arterial stiffness was not significantly different between the study and control groups and it did not change significantly after 6 months of intervention (Tables 2, 3).
The daily calorie intake was reduced from a mean of 2,827.3 kcal to a mean of 2,278.7 kcal, the percentage of fats was decreased from 34% to 31% and the consumption of fibers was increased from 19.7 to 26.3 g in the intervention group. The weekly physical activity was increased from 87±17 to 203±19 minutes in the intervention group.
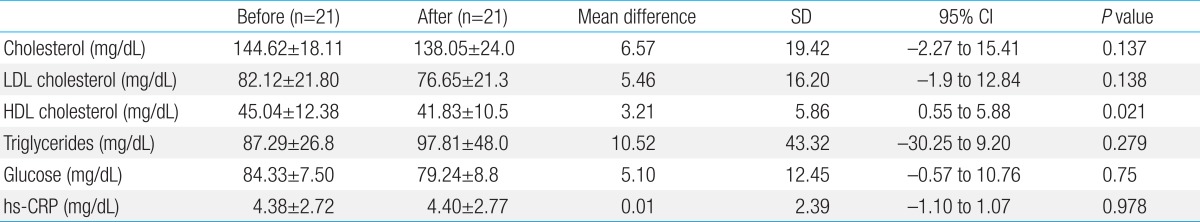
No association was found between arterial stiffness and anthropometric parameters (weight, height, BMI). C-reactive protein did not decrease significantly after the intervention (P=0.97). Low-density lipoprotein decreased, but not significantly, from 82.12±21.8 to 76.65±21.3 mg/dL. Table 4 summarizes the laboratory results of the participants.
Discussion
This study reports that a dormitory based program of lifestyle modifications, including nutritional intervention and encouraging physical activity had a positive effect on the food habits, physical activity and BMI parameters in obese adolescents, but it failed to illustrate correlations between a reduction in BMI and other parameters such as arterial stiffness and lipid profile. Also, we faced many problems whilst trying to make lifestyle changes among adolescents residing in a dormitory school.
In recent years, it has been shown that in children, individuals with obesity have increased aortic stiffness14). However, increased aortic stiffness has been shown to be more related to body fat repartition assessed by waist circumference15) and visceral adiposity16) than to an increase BMI. The current study refers only to the value of BMI as an expression of obesity, which may partially explain the results.
Previous studies suggested that regular endurance exercise is particularly helpful in improving the lipid lipoprotein profile of men with low HDL cholesterol levels along with abdominal obesity and elevated triglyceride concentrations17,18). The findings in our study, regarding the negative effect of regular endurance exercise on HDL level, is concordant with the common observation that it is very difficult in clinical practice to increase the cholesterol content of HDL when it is an isolated lipoprotein characteristic.
Consistent with previous studies19), adolescents in this study demonstrated suboptimal eating behaviors including poor vegetable and fruit intake. Data from the Health Behavior in School-Aged Children study in Canada suggests that 41% of students with a high family affluence score report eating fruit at least once per day, compared to 31 percent for students with low family affluence scores20). Many programs in school, community and clinic settings have attempted to modify the home environment by involving families, either through direct involvement or through activities the children completed with their families at home. Some programs in the home setting were small, short-term (<10 weeks) experimental interventions, which demonstrated that sedentary behaviors can be significantly modified in this setting21,22). One of the few effective obesity treatment programs for school-aged children demonstrated a sustainable change 10 years after the program, with a strong parent involvement component in the intervention23).
Most of the programs that did address the environment were in primary school settings and this mainly involved modification of school cafeteria menus and staff training to ensure healthier food and beverage options24,25). A few programs in the primary school setting implemented additional strategies to modify the food service and create more supportive environments by promoting exercise activities26).
Our current study attempted to combine between the 2 strategies by trying to modify school menus and increase physical activities among the participants. Indeed, the BMI of the participants was significantly reduced. However, the cooperation of the school staff in modifying the menu was unsuccessful. This can be partially explained by probable budget issues since extra funding was required in order to serve and maintain healthier food options.
The aforementioned studies intervened among preschool and primary school aged children. Preschool-age is a critical period of development that affects growth patterns and associated health outcomes into adulthood. Results of trials assessing children in preschool environments were not consistent. Some failed to demonstrate improvements in growth patterns27), others succeeded in attributing successfulness to the inclusion of parentchild dyads instead of preschool-aged children alone28).
Our study aimed its focus on a more problematic group consisting of adolescents residing in a dormitory setting remote from their families. Like the studies performed on preschool children, this study also illustrates the substantial importance of parental participation in diet programs from childhood to adulthood.
Given that adolescents typically interact with a variety of different people on a daily basis, the likelihood that these social interactions will in some way affect how these adolescents think and act about a health behavior, such as being active, seems apparent. The effects of social influence have been reported across a number of adolescent health behaviors including diet and physical activity29). We assume that because the intervention in the current study was directed only towards a specific group in the dormitory school without wider participation of the other students, it may have created some negativism amongst the other students, thus harmfully influencing the students and reducing their cooperation in the study.
Our study was unique because it tried to interfere and make lifestyle changes in a dormitory school setting. There are notable limitations to our study. Our sample size was small, the follow-up period was short, compliance of the participants and parent involvement were low and cooperation of the school staff was unsatisfactory.
Our study population included adolescents from the "Ben-Shemen" dormitory. The intervention trial in this specific population was challenging for a number of reasons. First, this population originates from a low socioeconomic background and they spend most of their time in the dormitory itself, leaving for vacations only every other weekend. Second, parent cooperation was minimal and they received most of the support during the intervention from the dormitory staff. Also, the surveillance and control of the adolescents during their weekend vacations was minimal. It is difficult to evaluate the parents' role when a diet program is implemented in a dormitory school. However, the fact that parents were not an active part in this current study might have had a negative effect on the compliance of the participants.
Additionally, our intervention team did not include psychiatrists or psychologists, which may have further reduced the chances of success. Previous studies have shown that up to fifty percent of obese adolescents have comorbid psychopathology (depression, behavioral problems and low self-esteem) and that treatment compliance was poor30,31).
The participants in the present study were from a low socioeconomic background. This confounding variable was not taken into consideration. A study that was performed in the United States revealed a high prevalence of overweight (43% in boys and 41% in girls) and a number of problems in the physical activity and eating patterns of children from low socioeconomic backgrounds32). Another study identified that to be successful, childhood obesity prevention programs likely need to address environmental and socioeconomic factors that go beyond the school setting33).
In order to make life style changes in an adolescent dormitory, there is a need for more active participation of parents at home and at the dormitory in collaboration with the dormitory staff; dormitory schools need to employ nutritionists and maintain healthier menus; adolescents in dormitory schools need periodic assessments by pediatricians and psychiatrists focusing on BMI and psychiatric evaluation; dormitory schools have to organize regular workshops in order to raise awareness of overweight damage, the need for healthy food and orderly sport activity; and finally dormitory school budgets must be raised in order to enable the children to maintain healthier lifestyles.
In conclusion, making lifestyle modifications amongst adolescents in a dormitory school is a complex task. Although active intervention managed to ameliorate BMI parameters, we believe that in order to maximize the beneficial effects of any intervention in a similar setting in the future, there is a need for a multidisciplinary well-trained team, with an emphasis on integrating parents and the school environment.
Notes
No potential conflict of interest relevant to this article was reported.