Articulation error of children with adenoid hypertrophy
Article information
Abstract
Purpose
Adenoid hypertrophy is a physical alteration that may affect speech, and a speech disorder can have other negative effects on a child's life. Airway obstruction leads to constricted oral breathing and causes postural alterations of several oro-facial structures, including the mouth, tongue, and hyoid bone. The postural modifications may affect several aspects of speech production.
Methods
In this study, we compared articulation errors in 19 children with adenoid hypertrophy (subject group) to those of 33 children with functional articulation disorders independent of anatomical problems (control group).
Results
The mean age of the subject group was significantly higher (P=0.016). Substitution was more frequent in the subject group (P=0.003; odds ratio [OR], 1.80; 95% confidence interval [CI], 1.23-2.62), while omission was less frequent (P<0.001; OR, 0.43; 95% CI, 0.27-0.67). Articulation errors were significantly less frequent in the palatal affricative in the subject group (P=0.047; OR, 0.25; 95% CI, 0.07-0.92). The number of articulation errors in other consonants was not different between the two groups. Nasalization and aspiration were significantly more frequent in the subject group (P=0.007 and 0.014; OR, 14.77 and 0.014; 95% CI, [1.62-135.04] and NA, respectively). Otherwise, there were no differences between the two groups.
Conclusion
We identified the characteristics of articulation errors in children with adenoid hypertrophy, but our data did not show the relationship between adenoid hypertrophy and oral motor function that has been observed in previous studies. The association between adenoid hypertrophy and oral motor function remains doubtful.
Introduction
Adenoid hypertrophy is a common condition in children and can cause symptoms such as mouth breathing, nasal discharge, snoring and sleep apnea1). The quality of life of children with adenoid hypertrophy may be affected, with emotional distress, reduced day-time functioning, and a high degree of concern from care-givers, apart from sleep disturbance2).
Adenoid hypertrophy is a physical alteration that may affect speech. Additionally, a speech disorder can have other negative effects on a child's life3). The airway obstruction leads to constricted oral breathing which, in turn, causes postural alterations of several oro-facial structures such as an open mouth, lower-anterior position of the tongue, and a lower position of the hyoid bone. Over time, these postural alterations may also effect dental occlusion and facial skeletal growth. The postural modifications may in turn affect several aspects of speech production4,5,6,7,8).
Several reports concerning articulation disorders and language difficulties of children with adenoid hypertrophy have been published9,10,11,12). However, to date, no comparative study exists that investigated articulation patterns of children with adenoid hypertrophy who developed articulation disorders compared to a control group.
In this study, we investigated articulation patterns of children with adenoid hypertrophy who developed articulation disorders and compared these patterns to those of children with functional articulation disorders independent of adenoid hypertrophy or other anatomical problems. We aimed to determine the relationship between adenoid hypertrophy and articulation disorders, and to detect children who have articulation disorders associated with adenoid hypertrophy in clinical practice.
Materials and methods
1. Subject and control groups
Fifty-four children aged between 4 and 6, who were admitted to the pediatric outpatient clinic of Uijeongbu St. Mary's Hospital for articulation difficulties from January 1, 2002 to December 31, 2012, were enrolled in this study. We set an age limit for homogeneity in the subjects of study. The previous study revealed that the percentages of correct consonants (PCC) were not different in children aged between 4 and 613). They were divided into two groups: the subject and control group. The subject group (19 children) included those who had adenoid hypertrophy and the control group (33 children) included those who didn't have adenoid hypertrophy. If they were clinically warranted, lateral x-rays of nasopharynx were performed and adenoid-nasopharyngeal ratio >0.7 was defined as adenoid hypertrophy. Children with other anatomical structure diseases such as tongue-tie or cleft palate, neurological problems, or speech/language development delays were excluded from this study.
2. Methods
1) Analysis of articulation patterns of the subject and control groups
Medical records were reviewed retrospectively, when the results of speech-language pathological evaluation were available. We also reviewed demographic data, detailed clinical histories, developmental profiles, neurological examination, and physical examination including tongue tip mobility.
All children underwent the Picture Consonant Articulation Test (PCAT) to investigate articulation patterns. Twenty-five words including 43 consonants in Korean language were evaluated by 21 picture cards. The analysis proceeds in a top-down direction meaning it begins with a word and finishes with an analysis of segments. The PCC was calculated to provide a quantitative measure between subjects.
Articulation errors were analyzed according to phonological processes. Articulation errors were divided into 4 types: substitution, distortion, omission, and addition. The distribution of articulation error types was then compared between the two groups. The number of articulation errors in each consonant according to types of articulation errors and positions in words was counted by a speech pathologist. The number of articulation errors that were classified as addition was not counted because they would not reflect the limit of articulation. The speech pathologist reported the main and continuous articulation errors based on careful observation from the raw PCAT data.
The number of children with articulation errors in each consonant type according to position and manner of articulation was counted. Next, articulation errors applicable to substitution and distortion were categorized according to phonological changes in the position of articulation, manner of articulation, and the level of tension and aspiration. The number of children with articulation errors according to the categories of phonological changes was also counted.
The Oral Speech Mechanism Screening Examination-Revised was administered to assess anatomical structures and physiological functions that are considered to be potentially related to speech or language disorders. The Preschool Receptive Expressive Language Scale was examined to assess other speech or language development. The Denver Development Screening Test II and further neurologic evaluation were also used if clinically warranted by a pediatrician's decision. As stated previously, Children with other anatomical structure diseases, neurological problems, or speech/language development delays were excluded from this study.
2) Comparison between the subject and control group
Demographic data, such as age and sex, as well as PCC were compared between the subject and control groups. Among summarized data of articulation errors in the subject and control groups, the numbers of articulation errors by type were compared. Next, the number of children with articulation errors according to each consonant type and the categories of phonological changes were compared between the two groups. The collected data between the subject and control groups were compared using Fisher exact test and odds ratios with 95% confidential intervals (CI) for the categorical variables and the independent Mann-Whitney U test for the continuous variables.
3. Ethics statement
The study protocol was approved by the Institutional Review Board of Uijeongbu St. Mary's Hospital (IRB No. UC13RISE0051).
Results
1. Demographic data
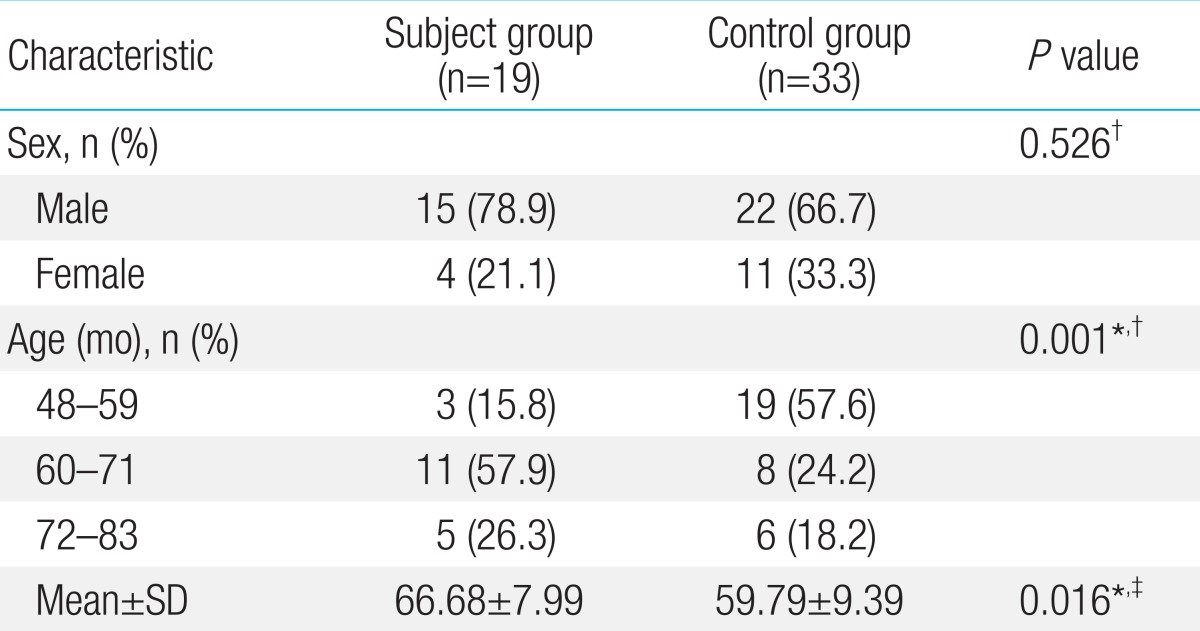
Demographic data of the subject and control groups are summarized in Table 1. The gender ratio between the two groups was not significantly different. The mean age of the subject group was significantly higher and the age distribution of the two groups was significantly different.
The mean PCC and standard deviation (SD) were 74.58%±16.69% in the subject group and 71.87%±12.94% in the control group. PCC was not significantly different between the two groups (P=0.418).
2. Summary of articulation errors in subject and control groups
The number of articulation errors for each consonant according to type of articulation error and position in words is summarized in Tables 2 and 3.

Number of articulation errors in each consonant according to type of articulation error and position in words (subject group)

Number of articulation errors in each consonant according to type of articulation error and position in words (control group)
In the subject group, the main types of articulation errors were substitution (118/165 cases, 71.5%), followed by omission (27/165 cases, 16.4%) and distortion (20/165 cases, 12.1%). Similarly, the main types of articulation errors were substitution (337/578 cases, 58.3%) in the control group, followed by omission (181/578 cases, 31.3%) and distortion (60/578 cases, 10.4%). But significant differences were found in the proportion of articulation errors by type between the two groups. Substitution was significantly more frequent in the subject group than in the control group (P=0.003; odds ratio [OR], 1.80; 95% CI, 1.23-2.62). Omission was significantly less frequent in the subject group than the control group (P<0.001; OR, 0.43; 95% CI, 0.27-0.67). Distortion was not significantly different between the two groups (P=0.569; OR, 1.19; 95% CI, 0.70-2.04).
In relation to each consonant, the sound /s/ was the most common (27/165 cases, 16.4%) in the subject group, followed by the sound /sh/ (25/165 cases, 15.2%), the sound /r/ (19/165 cases, 11.5%), the sound /ts'/ (18/165 cases, 10.9%), and the sound /tsh/ (18/165 cases, 10.9%). Conversely, the sound /ts'/ and /tsh/ was the most common (70/578 cases, 12.1% in both) in the control group, followed by the sound /sh/ (67/578 cases, 11.6%), the sound /s/ (65/578 cases, 11.2%), and the sound /k'/ (37/578 cases, 6.4%).
3. Comparison of articulation errors according to consonant type and category of phonological changes between the subject and control groups
A comparison of the number of children with articulation errors according to each consonant type is summarized in Table 4. Articulation errors were significantly less frequent in the palatal affricative in the subject group than in the control group (P=0.047; OR, 0.25; 95% CI, 0.07-0.92). The number of articulation errors in other consonants was not different between the two groups.
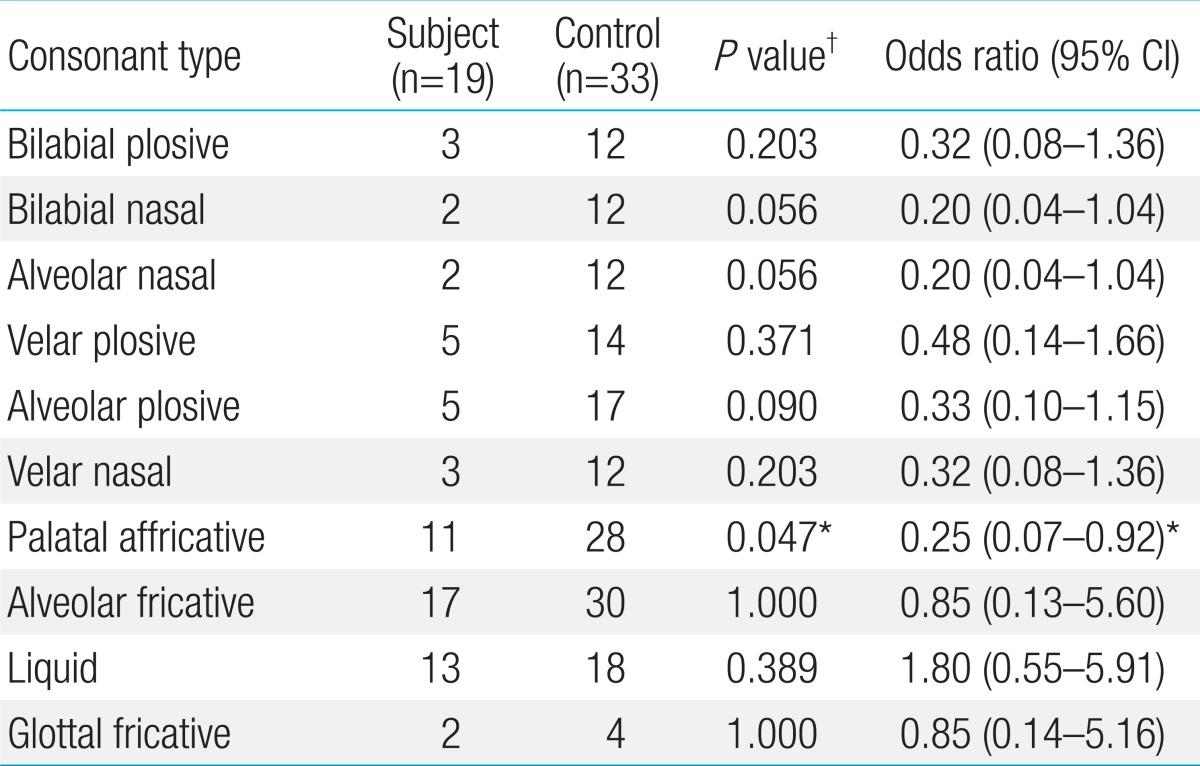
Number of children with articulation errors in each consonant type, between subject and control groups
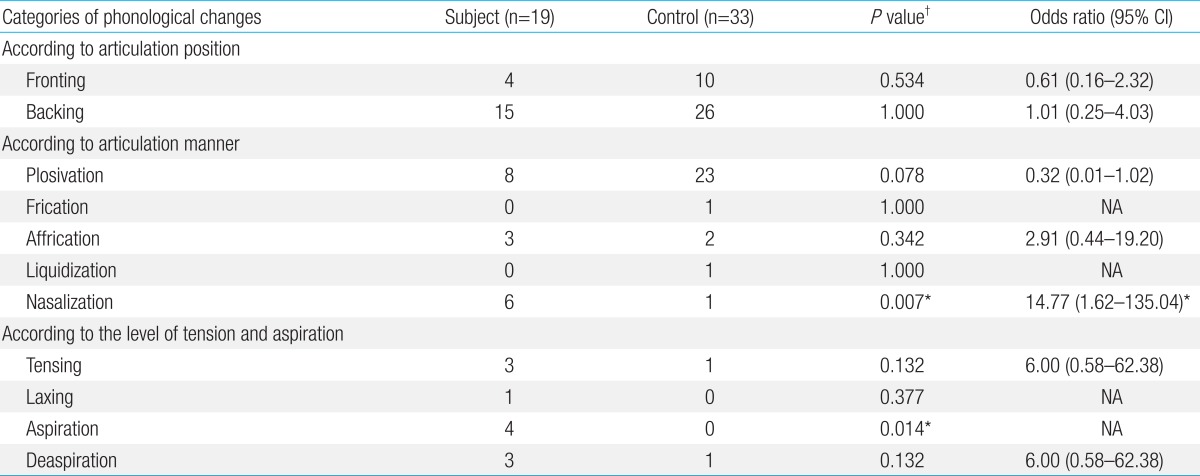
A comparison of the number of children with articulation errors according to phonological changes is summarized in Table 5. Nasalization and aspiration were significantly more frequent in the subject group than the control group (P=0.007 and P=0.014; OR, 14.77 and 0.014; 95% CI, [1.62-135.04] and [NA], respectively). Otherwise, there were no differences between the two groups.
Discussion
In this study, some characteristics were found in articulation error of children with adenoid hypertrophy.
First, this study showed the mean age of the subject group was significantly higher than the control group. Adenoids increase in size after birth, attain their maximum size at the age of four to six years, and remain the same until eight to nine years. So, the prevalence of adenoid hypertrophy generally increases with age in young children14), and it may be the reason of our result.
Second, this study demonstrated that the articulation errors of substitution were more frequent, while omission was less frequent in the children with adenoid hypertrophy than in the control group. These differences reflect that the articulation errors of children with adenoid hypertrophy resulted from anatomical or functional defects of articulation organs rather than children's phonological concept15,16).
Third, articulation errors in the palatal affricative were significantly less frequent in the subject group than the control group in this study. However, the number of articulation errors in other consonants including alveolar fricative was not different between the two groups. The previous study reported that children with adenoid hypertrophy are affected regarding the sound /s/3,17). The sound /s/ production requires a very precise placement of the articulators18). The sound 's' is produced with a low tongue-tip and the tongue blade at the site of maximum constriction which is consistently in the region mentioned. Meanwhile, as a consequence of a reduced oro-pharyngeal space, children with adenoid hypertrophy drop the mandible and tongue to maximize the oral airway. This affects the craniofacial development and causes deviations of the dental occlusion with a significantly more open intermaxillary jaw relationship, retrognathic inclined mandible, lateral cross-bite, and narrower intercanine width when compared to healthy controls3,5,19). Furthermore, articulation errors in the palatal affricative were rather less frequent in the subject group. The palatal affricative requires the delicate oral motor control similar to the alveolar fricative20). These results suggested that adenoid hypertrophy might not be related to the oral motor problems and were not consistent with previous studies. Lundeborg et al.3) reported that children with adenoid hypertrophy were affected regarding the /s/ sound, significantly more than normal controls without articulation disorders. In the study by Salami et al.17), surgery in children with adenoid hypertrophy led to significant improvements of the acoustic parameters. But these results could not exclude that the articulation errors might result from the other factors rather than adenoid hypertrophy, and oral motor dysfunctions might be present only in certain of individuals with adenoid hypertrophy. In addition, Lunderborg et al.3) failed to reveal that post surgery speech productions were improved significantly compared to preoperative ratings.
Fourth, nasalization and aspiration were significantly more frequent in the subject group than the control group in relation to phonological changes. Previous studies showed that adenoid hypertrophy contributes to hypernasal speech. Hypertrophic adenoids could alter oropharyngeal resonance characteristics. Adenoid hypertrophy may intrude into the pharyngeal airway and alter the pharyngeal resonance of speech, which would result in a muffled resonance and possibly hypernasality if they interfere with palatal or pharyngeal motion21,22,23). And, previous studies also showed that adenoid hypertrophy causes changes in the dimensions of the vocal tract that are evident as increased shimmer values. Change in shimmer in turn is reflected in the roughness of the voice. So adenoid hypertrophy may result in articulation errors of aspiration and our results were consistent with previous studies24,25).
The limitations of this study are the small number of enrolled children and its retrospective design. And this study could not explain which factors the articulation errors of children with adenoid hypertrophy actually resulted from, although it showed that the errors regarding the alveolar fricative and palatal affricative were not more frequent in those children. Only a few studies related to this topic have been conducted, so a more expanded analytical study related to anatomy, physiology, and phonetics is necessary.
To our knowledge, this is the first study that compared articulation errors in children with and without adenoid hypertrophy. We found some characteristics of articulation errors in children with adenoid hypertrophy. These results can help to determine the relationship between adenoid hypertrophy and articulation disorders and to detect children who have articulation disorders associated with adenoid hypertrophy in clinical practice. But this study did not reveal the relation between adenoid hypertrophy and the oral motor function which were observed in previous studies. The articulation errors of children with adenoid hypertrophy may result from other factors rather than adenoid hypertrophy and oral motor dysfunctions may be present only in certain of individuals with adenoid hypertrophy. The relation between adenoid hypertrophy and the oral motor function remains doubtful. Therefore, clinicians should be careful when determining the relationship between adenoid hypertrophy and oral motor function.
Acknowledgments
The authors would like to thank Prof. Hyeon-Woo Lim for the statistical consultation for this article.
Notes
No potential conflict of interest relevant to this article was reported.