Developmental profiles of preschool children with delayed language development
Article information
Abstract
Purpose
This study examines changes in developmental profiles of children with language delay over time and the clinical significance of assessment conducted at age 2-3 years.
Methods
We retrospectively reviewed the medical records of 70 children (62 male, 8 female), who had visited the hospital because of delayed language development at 2-3 years, and were reassessed at ages 5-6. Language and cognitive abilities were assessed using multiple scales at the initial and follow-up visits.
Results
At the initial test, 62 of the 70 children had mental development index (MDI) below 70 of Bayley Scales of Infant Development Test II. Of the 62 children in the follow-up assessment, 30 children (48.4%) remained within the same cognitive range (full-scale intelligence quotient, FSIQ<70 of Wechsler preschool and primary scale of intelligence), 12 had borderline intellectual functioning (FSIQ, 70-85), 6 improved to average intellectual functioning (FSIQ>85), and 5 had specific language impairment, 9 had autism spectrum disorders. At the initial test, 38 of the 70 children had cognitive developmental quotients (C-DQ) below 70. Of the 38 children in the follow-up assessment, 23 children (60.5%) remained within the same cognitive range (FSIQ<70). The correlation coefficient for MDI and FSIQ was 0.530 (P<0.0001) and that for C-DQ and FSIQ was 0.727 (P<0.0001). There was a strong correlation between C-DQ and FSIQ, and a moderate correlation between MDI and FSIQ.
Conclusion
Low MDI scores reflect a specific delay in cognitive abilities, communication skills, or both. The C-DQ, receptive language development quotient, and social maturity quotient also help to distinguish between children with isolated language delay and children with cooccurring cognitive impairment. Moreover, changes in the developmental profile during preschool years are not unusual in children with language delay. Follow-up reassessments prior to the start of school are required for a more accurate diagnosis and intervention.
Introduction
It is thought that all typically developing children in all cultures master the basics of their language by 4 years of age1). However, 5% to 8% of children experience speech-language delays or disorders in preschool years that may be associated with subsequent learning, socioemotional, or behavioral problems1).
There are marked variations among normal children in the rate of development of the comprehension of words, production of single words, and use of combinational forms within the first 2-3 years of life. Up to 20% of a 2-year-old children have delayed expressive language2,3), which resolves by 4 to 5 years of age in about 50%-60% of cases4,5). Children with speech and language impairment persisting at age 5 years were at high risk for language, literacy, and educational difficulties throughout childhood and into adolescence6,7).
Some children began speaking between 2 and 3 years of age. Parents often wait until the child is 3 years old before requesting an evaluation for a child who is not talking. However, a language developmental quotient of <75 by 16 to 24 months of age is considered significant8). Clinicians should not wait until children are ≥3 years of age to evaluate delayed language or speech8). The major considerations in the differential diagnosis of expressive language delay are isolated language delay, language delay as part of a more general developmental condition, hearing impairment, or poor linguistic environment. However, it is difficult to predict which of the children showing initial delays are likely to develop disorders. Determining whether a developmental difference is significant or not, and thus warranting further evaluation and intervention or not, is one of the clinician's greatest challenges.
The objective of this study was to assess the change in developmental profiles over time in children with language delay and the clinical significance of assessment conducted at age 2-3 years.
Materials and methods
1. Subjects
We retrospectively reviewed the medical records of 70 children (62 males and 8 females) who visited the hospital because of delayed development of language at the age of 2-3 years, and who were reassessed at the age of 4-6 years at the Pediatric Clinic of Daegu Catholic University Hospital from January 2003 to December 2013.
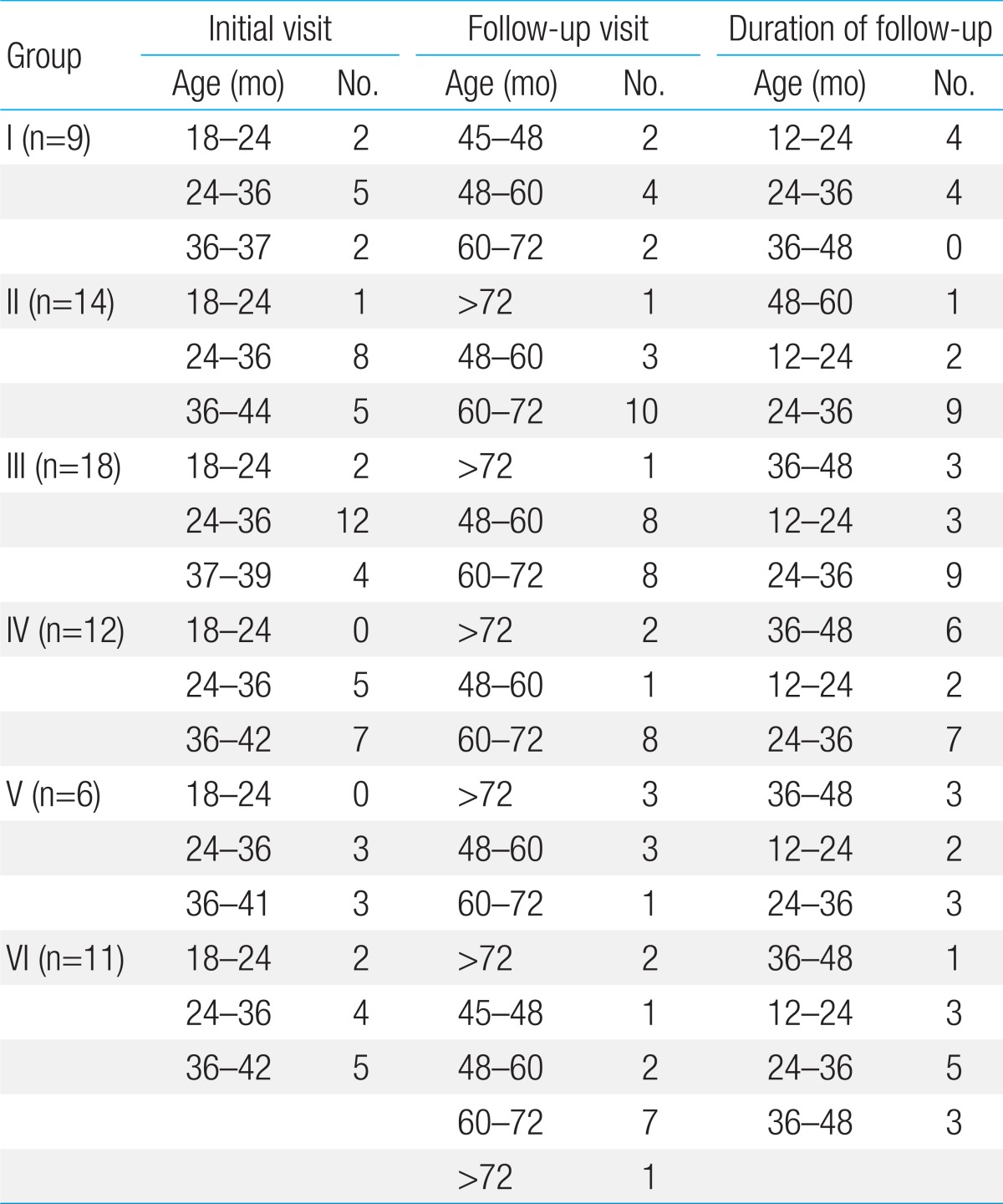
At the initial visit, the 70 children had a mean age of 33.8±6 months (age distribution: 18-24 months, 7; 24-36 months, 37; 36-42 months, 26). At the follow-up visit, they were assessed at a mean age of 63.37±8.52 months (age distribution: 45-48 months, 3; 48-60 months, 21; 60-72 months, 36; >72 months, 10). The mean follow-up duration was 29.6±8.64 months (12-56 months) (Table 1).
Children were underwent medical and physical examinations. In some cases, hearing tests, brain magnetic resonance imaging (MRI) scan, cytogenetic/molecular genetic studies, and inborn errors of metabolism workup were performed. Sixty-five children were born at term with mean birth weight of 3.4±0.47 kg and 5 children were born preterm (gestational age: 35-37 weeks) with mean birth weight of 2.58±0.58 kg. Eight children had a family history of speech and language impairment, mental retardation, or autism spectrum disorders. There was 1 case of Fragile X syndrome, 1 case of Cornelia de Lange syndrome, who has neither major congenital malformations nor hearing defect, and 2 cases of microcephaly. Children who were affected by an organic cause (major congenital malformations), metabolic disorders, neurological complications, visual or hearing defects, or epilepsy were excluded.
2. Methods
The children were examined for language and cognitive abilities assessed at initial visit, 2-3 years later, reassessed at follow-up visit. The Sequenced Language Scale for Infants9) or Preschool Receptive-Expressive Language Scale10) are applied taking into account each subject's age and language development level. To identify a child with language development delay, we use a criterion of 1.25 standard deviations (SD) below the mean of standardized measures or <10th percentile as a clinical cutoff1). In addition, the receptive language development quotient (RL-DQ) and expressive language development quotient were calculated to compare subjects with developmental language delay.
Bayley Scales of Infant Development Test II (BSID-II)11) has become a gold standard for assessment of early child development. The BSID-II11,12) is used to assess cognitive function in children aged 1 month through to 42 months. The mental and motor dimensions can be categorized into the finer domains of cognitive, language, social, and motor. Mental development index (MDI) was used both as a continuous variable (mean±SD, 100±15) and as a categorical variable. A significant delay was defined as an MDI<70 (-2 SD or less) and a mild delay as 70-84 (-2 SD<MDI<-1 SD). MDI≥85 (-1 SD or more) was considered average. In the MDI, the individual scores for language and nonverbal cognitive abilities were not reported separately, so we used the cognitive developmental quotient (C-DQ) (developmental age/chronological age×100) from the cognitive developmental age, which is the child's level of cognitive function on the mental and motor scale facets of BSID II.
The Wechsler Preschool and Primary Scale of Intelligence (WPPSI)13) is used to assess the cognitive function of preschool children (aged 3 years through to 7 years). WPPSI13) provides 3 intelligence scores: a performance intelligence quotient (PIQ), verbal IQ (VIQ), and full-scale IQ (FSIQ). All 3 IQ scores have a mean of 100 and a SD of 15. An IQ≥85 (-1 SD or more) is considered average and an IQ<70 (-2 SD or less) as mental retardation; an IQ between 70 and 84 (-2 SD<IQ<-1 SD) is considered borderline intellectual functioning.
The Korean Social Maturity Scale (K-SMS)14) is a measure of personal and social skills needed for everyday living of individuals of aged 0 years through to 30 years. The items of the scale represent progressive maturation in the domains of self-help, self-direction, locomotion, occupation, communication, and social skills. It provides the social maturity quotient (SQ; social age/chronological age×100). K-SMS14) was used at initial assessment and follow-up. The Korean version of the Childhood Autism Rating Scale15) was used for the diagnosis of autism spectrum disorder.
3. Diagnostic criteria
Mental retardation (non-autistic-intellectual disability), autism spectrum disorders, and developmental language disorder were classified based on the diagnostic and statistical manual of mental disorders, 4th edition classification system16). For the diagnosis of specific language impairment, we also used the clinical research definition, which requires as a combination of normal intelligence (performance IQ>85) and language impairment (a composite language measure falling more than 1.25 SD below the mean). A -1.25 SD cutoff for language impairment is approximately equivalent to the 10th percentile or below17).
4. Statistical analysis
Statistical analyses were conducted using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Results are reported as mean±SD. The associations between MDI, C-DQ, RL-DQ, SQ from initial visit test results, and FSIQ from follow-up visit test results were studied by using Spearman's correlation. The level of significance was set at <0.05.
Results
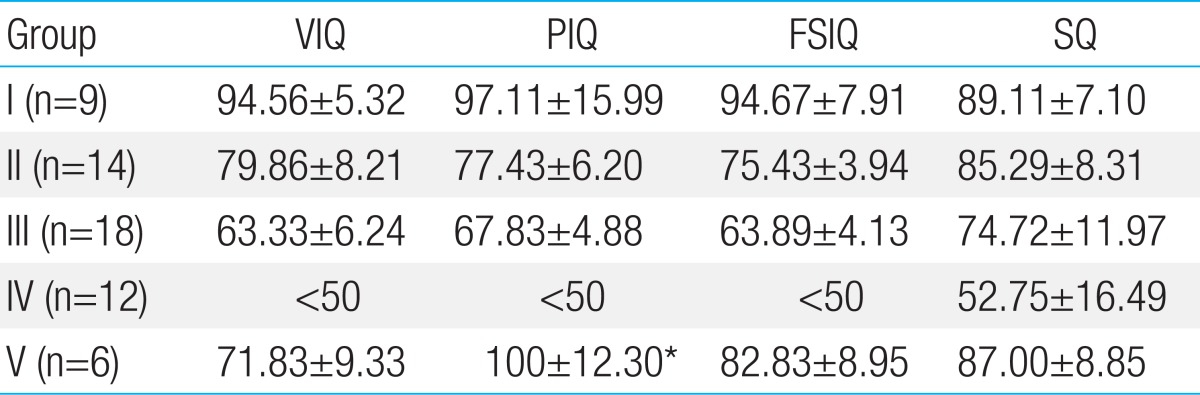
On the basis of reassessment test results at follow-up, the 70 children were divided to 6 groups (Tables 1,2,3). Group I included 9 children with average intelligence (VIQ≥85, PIQ≥85, FSIQ≥85) without language impairment. The mean VIQ was 94.56±5.32, mean PIQ was 97.11±15.99, mean FSIQ was 94.67±7.91, and mean SQ was 89.11±7.10. The language skills of these 9 children, who had delayed language development at the initial visit, had caught up at the follow-up visit. Their mean age was 30.33±6.78 months at initial visit, and 58.33±11.87 months at follow-up visit. Group II included 14 children with borderline intellectual functioning (FSIQ, 70-84). The mean VIQ was 79.86±8.21, mean PIQ was 77.43±6.2, mean FSIQ was 75.43±3.94, and mean SQ was 85.29±8.31. Their mean age was 33.71±5.71 months, at initial visit and 64.07±5.69 months at follow-up visit. Group III included 18 children with mild mental retardation (FSIQ, 50-69). The mean VIQ was 63.33±6.24, mean PIQ was 67.83±4.88, mean FSIQ was 63.89±4.13, and mean SQ was 74.72±11.97. Their mean age was 32.39±5.52 months at initial visit and 63.11±8.39 months at follow-up visit. Group IV included 12 children with moderate to severe mental retardation (FSIQ<50). The mean VIQ was <50, mean PIQ was <50, mean FSIQ was <50, mean SQ was <50. Their mean age was 36.42±5.21 months at initial visit and 66.58±7.13 months at follow-up visit. Group V included 6 children with specific language impairment (PIQ≥85, and persistent language impairment, language measure<10th percentile). The mean VIQ was 71.83±9.33, mean PIQ was 100±12.30, mean FSIQ was 82.83±8.95, and mean SQ was 87±8.85. VIQ of one of the 6 children had a VIQ score of ≥85. Two children had a VIQ score of 70-84, Three children had a VIQ score of 50-69. These children had delayed language development at initial visit (mean age, 37.5±3.51 months), Their expressive language had not caught up at follow-up visit (mean age, 64.0±10.2 months).
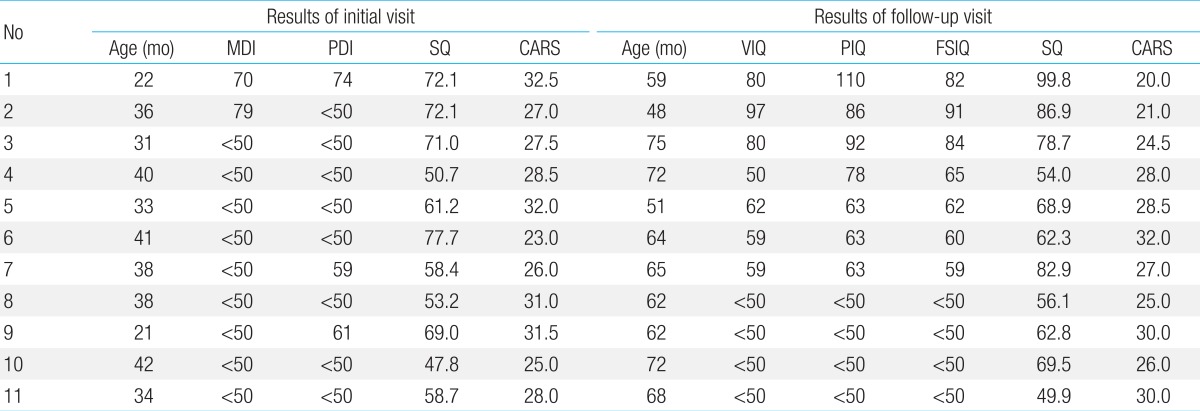
Group VI included 11 children with autism spectrum disorders. FSIQ of one of the 11 ASD children had a FSIQ score of ≥85. Two children had a FSIQ score of 70-84, Four children had a FSIQ score of 50-69. Four children had a FSIQ score of <50. Their mean age was 34.18±7.13 months at initial visit and 63.18±9.1 months at follow-up visit.
1. Whole group analysis
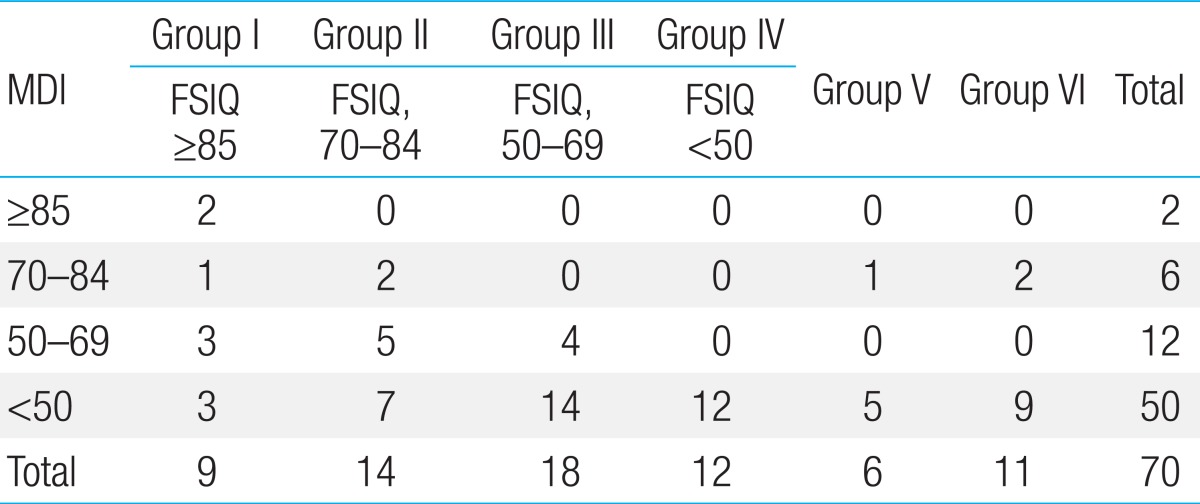
Sixty-two of the 70 children had MDI<70 at initial test: 9.6% (6/62) had average intellectual functioning. 19% (12/62) had borderline intellectual functioning, 48.4% (30/62) had mental retardation, 8% (5/62) had specific language impairment, and 14.5% (9/62) had autism spectrum disorders at follow-up assessment (Table 4).
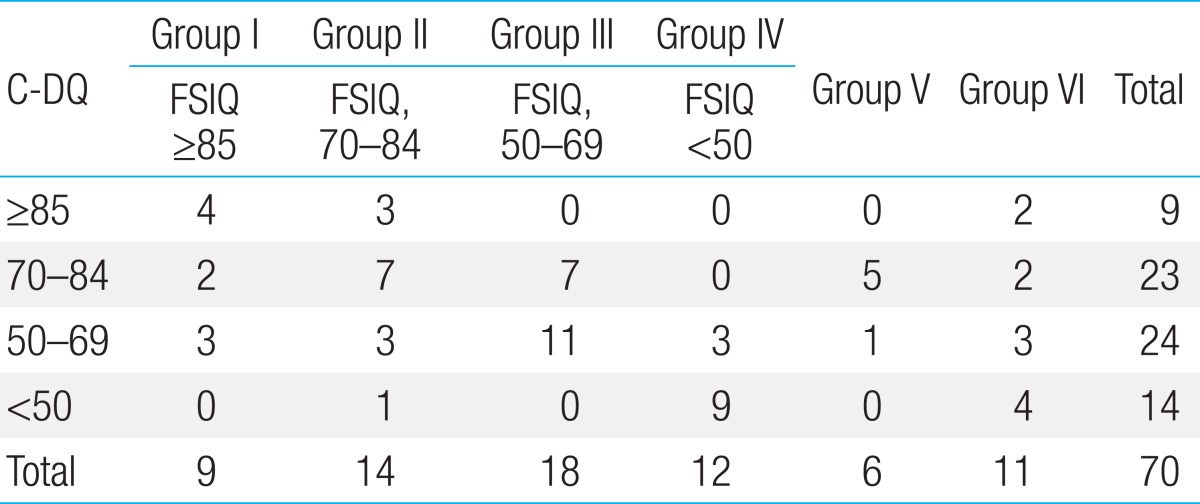
Thirty-eight of the 70 children had C-DQ<70 at initial test: 7.8% (3/38) had average intellectual functioning. 10.5% (4/38) had borderline intellectual functioning, 60.5% (23/38) had mental retardation, 2.6% (1/38) had specific language impairment, and 18.4% (7/38) had autism spectrum disorders at follow-up assessment (Table 5).
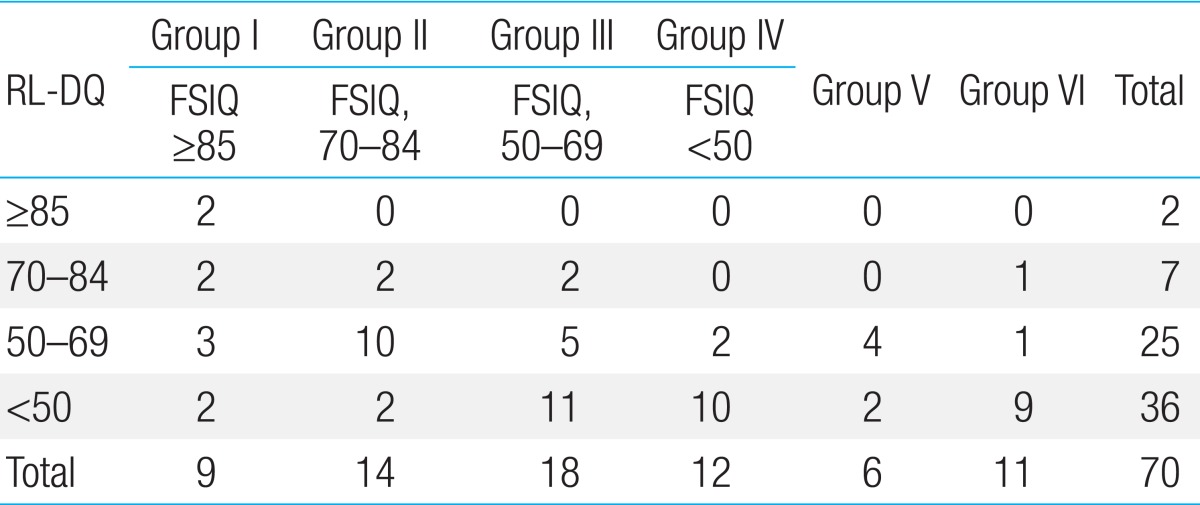
Sixty-one of the 70 children had RL-DQ<70 at initial test: 8.2% (5/61) had average intellectual functioning. 19.7% (12/61) were borderline intellectual functioning, 45.9% (28/61) had mental retardation, 9.8% (6/61) had specific language impairment, 16.4% (10/61) had autism spectrum disorders at follow-up assessment (Table 6).
Thirty-two of the 70 children had SQ<70 at initial test: 6.25% (2/32) children had average intellectual functioning. 9.4% (3/32) had borderline intellectual functioning, 56.2% (18/32) had mental retardation, 6.3% (2/32) had specific language impairment, and 21.9% (7/32) had autism spectrum disorders at follow-up assessment (Table 7).
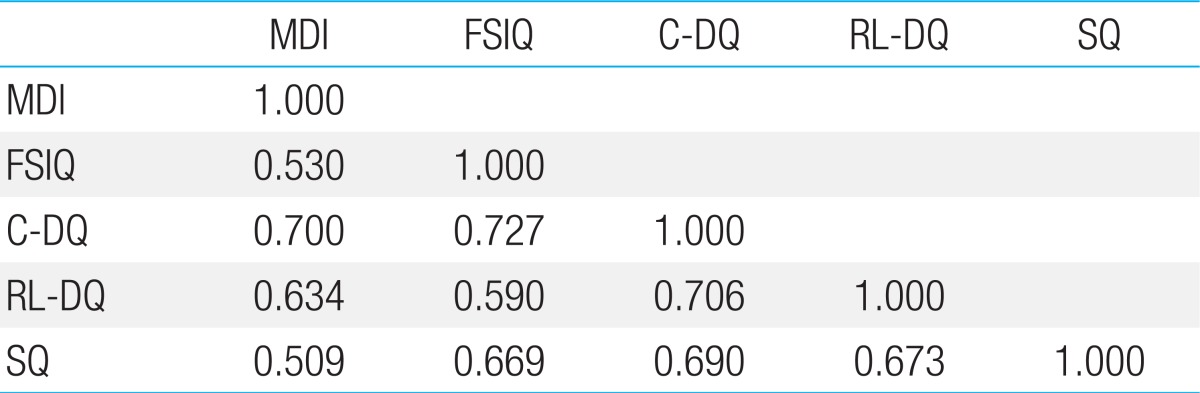
The correlation coefficient for MDI and FSIQ was 0.530 (P<0.0001) (Table 8). The correlation coefficient for C-DQ and FSIQ was 0.727 (P<0.0001). The correlation coefficient for RL-DQ and FSIQ was 0.590 (P<0.0001). The correlation coefficient for SQ and FSIQ was 0.669 (P<0.0001). There was strong correlation between C-DQ and FSIQ, and a moderate correlation between MDI and FSIQ.
2. Diagnostic subgroup analysis
In the 9 children in group I at initial assessment, 2 children had MDI≥85, 1 had MDI, 70-84, 6 had MDI<70 (Table 4); 4 had C-DQ≥85, 2 had C-DQ, 70-84, 3 had C-DQ<70 (Table 5); 2 had RL-DQ≥85, 2 had RL-DQ, 70-84, 5 had RL-DQ<70 (Table 6); 4 had SQ≥85, 3 had SQ, 70-84; 2 had SQ<70 (Table 7).
In the 14 children in group II at initial assessment, 0 had MDI≥85, 2 had MDI, 70-84, 12 had MDI<70 (Table 4); 3 had C-DQ≥85, 7 had C-DQ, 70-84, 4 had C-DQ<70 (Table 5); 0 had RL-DQ≥85, 2 had RL-DQ, 70-84, 12 had RL-DQ<70 (Table 6); 1 had SQ≥85, 10 had SQ, 70-84, 3 had SQ<70 (Table 7).
In the 18 children in group III at initial assessment, 0 had MDI≥85, 0 had MDI, 70-84, 18 had MDI<70 (Table 4); 0 had C-DQ≥85, 7 had C-DQ, 70-84, 11 had C-DQ<70 (Table 5); 0 had RL-DQ≥85, 2 had RL-DQ, 70-84, 16 had RL-DQ<70 (Table 6); 2 had SQ≥85, 10 had SQ, 70-84, 6 had SQ<70 (Table 7).
In the 12 children in group IV at initial assessment, 0 had MDI≥85, 0 had MDI, 70-84, 12 had MDI<70 (Table 4); 0 had C-DQ≥85, 0 had C-DQ, 70-84, 12 had C-DQ<70 (Table 5); 0 had RL-DQ≥85, 0 had RL-DQ, 70-84, 12 had RL-DQ<70 (Table 6); 0 had SQ≥85, 0 had SQ, 70-84, 12 had SQ<70 (Table 7).
In the 6 children in group V at initial assessment, 0 had MDI≥85, 1 had MDI, 70-84, 5 had MDI<70 (Table 4); 0 had C-DQ≥85, 5 had C-DQ, 70-84, 1 had C-DQ<70 (Table 5); 0 had RL-DQ≥85, 0 had RL-DQ, 70-84, 6 had RL-DQ<70 (Table 6); 0 had SQ≥85, 4 had SQ, 70-84, 2 had SQ<70 (Table 7).
In the 11 children in group VI at initial assessment, 0 had MDI≥85, 2 had MDI, 70-84, 9 had MDI<70 (Table 4); 2 had C-DQ≥85, 2 had C-DQ, 70-84, 7 had C-DQ<70 (Table 5); 0 had RL-DQ≥85, 1 had RL-DQ, 70-84, 10 had RL-DQ<70 (Table 6); 0 had SQ≥85, 4 had SQ, 70-84, 7 had SQ<70 (Table 7).
All the children in groups III and IV had MDI<70 (Table 4). They remained within the same cognitive range for both assessment scales.
Discussion
Our study demonstrated that early language delay is a useful indicator of several neurodevelopmental disorders. Of the 70 children in this study, 62 were male. Boys are more likely to have language delay compared with girls18).
Some children with language delay "catch up" during the preschool years (late bloomer), whereas others have persistent delay. Previous studies have documented the existence of "late bloomers"3,19,20,21). These children, who have limited expressive vocabulary and/or receptive language, do not have any other deficits such as cognitive, neurological, socio-emotional, or sensory deficit18). Therefore, their parents often wait and delay visiting the hospital. Of those who visited hospital at age 2-3 years, the majority had caught up with their peers in expressive language skills by 3-4 years of age18,21). Thus, most of them did not visit hospital again. However, even though these "late bloomers" had improved to achieve the normal range on standardized language measures, they continued to have significantly weaker language skills compared with their typically developing counterparts18). In addition, some children, whose language delays at age 3 or 4 years had apparently resolved, show difficulties in reading7,8).
Several factors that have been associated with resolution of language delay in the preschool years include isolated speech/language problem (i.e., normal developmental milestones in other domains), no receptive language difficulties, average intelligence, normal nonverbal skills and gestural communication, and capacity for symbolic thinking22,23,24). However, in this study, the initial assessment results for 9 children with average intelligence with improved language ability at the follow-up assessment (group I) were that only 3 children had isolated expressive language delay. Two children of group I had receptive-language delay, and the other 4 children had indications of impairments of cognitive or social skills. However, the language ability of these 6 children improved.
Children with persistent language delay are typically identified as children with specific language impairment. They will continue to experience difficulties throughout their school years and into adulthood18,21). Specific language impairment is a developmental language disorder involving significant language impairments in the context of normal nonverbal ability, hearing, and neurological status17). It is characterized by a significant discrepancy between the child's overall cognitive level (typically nonverbal measures of intelligence) and functional language level. Children with specific language impairment appear to learn visually and demonstrate their ability on nonverbal tests of intelligence. There is strong evidence that specific language impairment runs in families21). In this study, 2 children had a family history of delayed language development in their fathers. As has been found previously, boys are somewhat more likely than girls to have specific language impairment25). In addition, conditions that are associated with language delay, such as mental retardation and autism spectrum disorders, are more common in boys than girls26,27). The proportion of specific language impairment was lower than the proportion of cognitive impairment or autism spectrum disorders in this study. However, specific language impairment is more prevalent disorder. Estimates vary between 3% and 7% depending on definitions and statistical criteria employed21,28). Follow-up studies into childhood and adolescence showed that this disorder is persistent in a significant proportion of children21). Some children, in whom this disorder resolves, can experience language-related and other information-processing difficulties in later childhood21).
The language profile of children with autism is indistinguishable from that in children with specific language impairment. Longitudinal follow-up studies of preschool age children who have autistic features and do not meet the diagnostic criteria for autism at that age often found that they meet diagnostic criteria at school age, although some children improve over time8). The prevalence of autism spectrum disorders in Korea is approximately 9.2 per 10,000 in preschool children, 2.64% in school children29).
Mental retardation may be difficult to distinguish from autism spectrum disorders. In addition, a high percentage of individuals with autism spectrum disorders have cognitive deficits, and this can limit their ability to develop functional communication skills. In this study, the highest proportion of the cause of hospital visits in children suspected of delayed language development was cognitive impairment. A high prevalence of children with language delay and additional cognitive impairment has also been found in several other studies30,31,32). Because of the poor prognosis, it is important to identify such children as early as possible. Mental retardation is estimated to occur in 1%-10% of the population26). Detection of mental retardation is based on early recognition of cognitive delay, with the most common initial presenting symptom being language delay33). By careful attention to delay in language, visual problem solving, and adaptive development, most children who have moderate, severe, or profound mental retardation can be identified by 12 months of age. Mild mental retardation, often not recognized until school age, usually can be detected by 2 to 3 years of age in this way33).
The MDI of BSID-II of the 30 children with mental retardation (FSIQ<70) was all <70. The findings of this study suggest that if MDI is <70, the child is likely to be mental retardation in later years. This supports the utility of BSID-II as a child developmental test for early identification of mental retardation. However, in a group of 15 other children (9 children with average intelligence and 6 children with specific language impairment), 11 had MDI<70. These results showed that the low MDI scores reflect a specific delay in communication skills, cognitive abilities, or both. This broad nature of the MDI is the main limitation of the BSID-II.
Adequate intervention requires a clear distinction between isolated language delay and language delay associated with other neurodevelopmental problems such as cognitive impairment or autism spectrum disorders. Appropriate standardized developmental assessments are important. In addition, pediatricians should be knowledgeable about what each test is designed to measure. Each test is limited by what it was designed to measure, and no one test on its own captures all aspects of a child's functioning.
For developmental assessment, we used not only BSID-II, but also other assessment tools such as the Sequenced Language Scale for Infants and the K-SMS. The results of our study showed that not only MDI, but also C-DQ, RL-DQ, or SQ help to distinguish between children with isolated language delay and children with cooccurring cognitive impairment.
Early evaluation can help to identify children with language delay who will benefit from intervention and/or additional evaluation. However, accurate assessment is challenging because of the low frequency of verbal output, low motivation and the difficulty that young children have in cooperating with clinicians.
Children with language delay need to be followed up for several years. Because changes in the developmental profile during preschool years are not unusual, follow-up reassessments prior to the start to school will yield a more accurate diagnosis and form a better basis for educational planning and intervention.
Notes
No potential conflict of interest relevant to this article was reported.