Comparison of gastric and other bowel perforations in preterm infants: a review of 20 years' experience in a single institution
Article information
Abstract
Purpose
In this study, we aimed to review the clinical presentation of preterm infants with gastrointestinal perforations and compare the clinical features of gastric perforation with other intestinal perforations.
Methods
The medical records of preterm neonates with pneumoperitoneum, admitted to the neonatal intensive care unit (NICU) between January 1994 and December 2013, were retrospectively reviewed.
Results
Twenty-one preterm infants underwent exploratory laparotomy to investigate the cause of the pneumoperitoneum. The sample consisted of five patients (23.8%) with gastric perforation and 16 patients (76.2%) with intestinal perforation. No statistical differences were found in the birth history and other perinatal factors between the two groups. Underlying necrotizing enterocolitis, bilious vomiting, and paralytic ileus preceding the perforation were statistically more common in the intestinal perforation group. All preterm infants with gastric perforation survived to discharge; however, six preterm infants with intestinal perforation expired during treatment in the NICU. In the gastric perforation group, sudden pneumoperitoneum was the most common finding, and the mean age at diagnosis was 4.4±1.7 days of life. The location and size of the perforations varied, and simple closure or partial gastrectomy was performed.
Conclusion
Patients with gastric perforation did not have a common clinical finding preceding the perforation diagnosis. Although mortality in previous studies was high, all patients survived to discharge in the present study. When a preterm infant aged less than one week presents with sudden abdominal distension and pneumoperitoneum, gastric perforation should first be excluded. Prompt exploratory laparotomy will increase the survival rates of these infants.
Introduction
Despite advances in neonatology, gastrointestinal perforation remains a rare but fatal surgical emergency in the newborn infant. Pneumoperitoneum is the most common presenting symptom of gastrointestinal perforation in the newborn, and diverse underlying causes such as necrotizing enterocolitis (NEC), abdominal trauma, mechanical disruption from an orogastric tube insertion, sepsis, and distal gastrointestinal obstruction are often identified1). The location of perforation can vary from the esophagus to the colon. Among gastrointestinal perforations in newborns, gastric perforation is often associated with lower gestational age, lower birth weight, and a higher mortality rate2).
The etiology and pathogenesis of newborn gastrointestinal perforations are expected to differ depending on the perforation's location. However, not much has been reported on the topic. The purpose of this study was to review gastrointestinal perforations in our institution for the past 20 years and to compare the clinical features of gastric perforation with other intestinal perforations in the preterm infant. Furthermore, we reviewed our experiences of treating premature infants with gastric perforation and discuss the characteristics.
Materials and methods
1. Study population and methods
We retrospectively analyzed the medical records of 21 preterm infants who were diagnosed with pneumoperitoneum and underwent exploratory laparotomy at Ewha Womans University Mokdong Hospital's NICU from January 1994 to December 2013. We compared the clinical features of five patients who were diagnosed with gastric perforation to 16 patients who were diagnosed with other intestinal perforations.
The perinatal factors such as gestational age, birth weight, 1- and 5-minute Apgar score, mode of delivery, sex, maternal diseases, and the neonatal history including clinical course in the NICU, associated anomaly, signs and symptoms, radiologic findings, surgical findings, and outcome were analyzed between the two groups. The day of perforation was defined as the day when pneumoperitoneum was diagnosed with a simple radiograph. Pneumatosis intestinalis was diagnosed with a simple radiograph, and portal venous gas was diagnosed with an abdominal ultrasonogram. The site of perforation was confirmed during the exploratory laparotomy.
We used the following clinical definitions. Small-for-gestational-age (SGA) was defined as a birth weight less than the 10th percentile for gestational age. The fetal-infant growth chart for preterm infants by Fenton3) was used for the classification of SGA. Sepsis was defined as a positive blood culture with clinical symptoms indicative of sepsis. Respiratory distress syndrome (RDS) was diagnosed in infants with respiratory distress, an increased oxygen requirement, and a radiological finding consistent with RDS. NEC was defined as stage 2 or higher according to modified Bell's criteria4) or confirmed by operation findings. Patent ductus arteriosus (PDA) was diagnosed and considered hemodynamically significant if the diameter (mm) ratio of the left atrium to aortic root was more than 1.4 in the parasternal long axis view or ratio of the diameter of the ductus arteriosus (mm) to body weight (kg) was more than 1.4 by echocardiography5). Premature rupture of membrane (PROM) was defined as a positive nitrazine test or gross rupture of amniotic membranes for more than 24 hours prior to the delivery of the infant. Antenatal steroid exposure was defined as maternal receipt of dexamethasone during admission for delivery. A complete course of dexamethasone was defined as four 5-mg intramuscular doses given at 12-hour intervals, although the study included infants who received incomplete courses. Chorioamnionitis was confirmed through pathologic examination of the placenta showing acute inflammation with polymorphonuclear leukocyte infiltration into the chorionic-plate fibrin, fibrous chorion or amnion, and graded more than grade 2 according to the grading system suggested by Salafia et al.6). Disseminated intravascular coagulation (DIC) was defined as hemorrhagic symptoms with thrombocytopenia, prolonged prothrombin time and activated partial thromboplastin time, reduced level of fibrinogen, increased levels of fibrin degradation product and D-dimer, or reduced percentage of antithrombin III. Meconium stained was defined as the presence of meconium in the amniotic fluid at birth.
2. Statistical analyses
Statistical analyses were performed with the PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were analyzed by the Student t test or the Mann-Whitney U test, and categorical variables were analyzed with the chi-square test or the Fisher exact test. P<0.05 was considered statistically significant.
Results
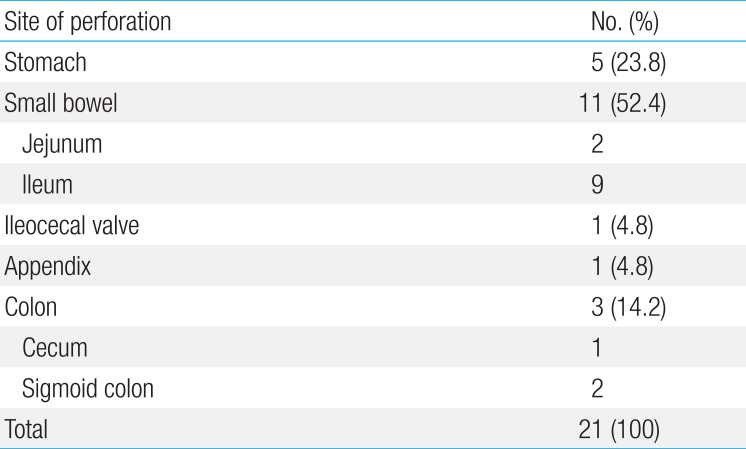
Among the 3,401 patients admitted to the NICU of Ewha Womans University Mokdong Hospital during the study's 20-year time period (January 1994 to December 2013), 21 patients were included for analysis. Patients (n=127) who did not survive to 48 hours after birth or were transferred to other hospitals were excluded, but 21 preterm infants with pneumoperitoneum underwent exploratory laparotomy; 5 cases of gastric perforation (0.147%) and 16 cases of intestinal perforations (0.470%). Table 1 describes the site of perforation in detail; five cases of stomach, 11 cases of small intestine, one case of ileocecal valve, one case of appendix, and three cases of colon (Table 1).
1. Comparison of gastric perforation and other intestinal perforations in preterm infants
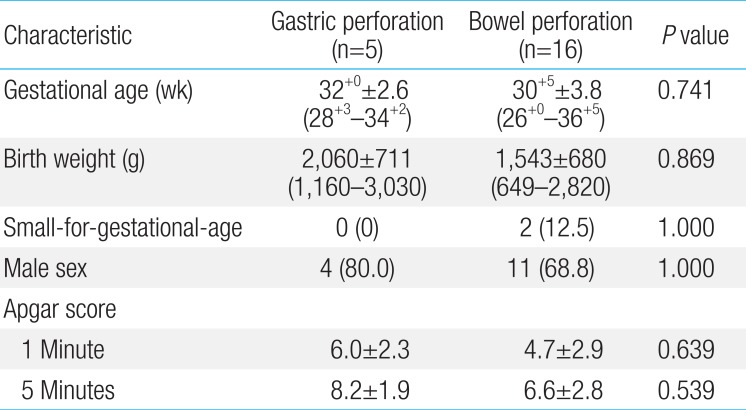
Of the 21 preterm infants diagnosed with pneumoperitoneum, five (23.8%) had gastric perforation, and 16 (76.2%) had other intestinal perforations. The mean gestational age and birth weight was not statistically different between the two groups; the gastric perforation was 32+0±2.6 weeks (28+3-34+2), 2,060±711 g, and the intestinal perforation was 30+5±3.8 weeks (26+0-36+5), 1,543±680 g. Male sex was dominant in both groups; 4/5 (80%) in the gastric perforation group and 11/16 (68.8%) in the other intestinal perforations group. The 1- and 5-minute Apgar scores were not different (Table 2). Perinatal history including incidence of PROMs, use of antenatal steroids, presence of chorioamnionitis, and meconium stained amniotic fluid were not different between the two groups.
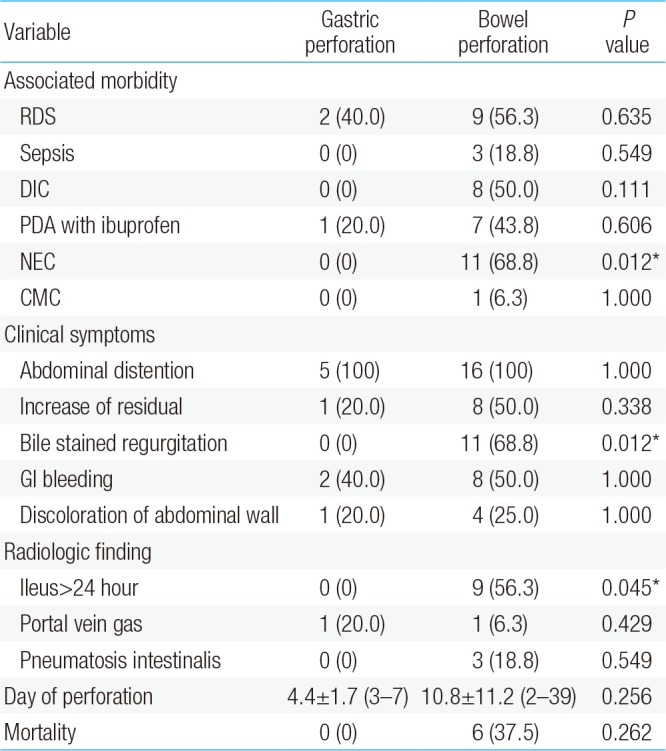
Associated clinical conditions were compared. The incidence of RDS, PDA, and sepsis were not statistically different between the two groups. Eight infants out of the 16 in the intestinal perforation group were more likely to be diagnosed with DIC (50%), but this difference was not statistically significant. They also had more comorbid conditions, although this was not statistically significant either. One infant of the intestinal perforation group accompanied by Hirschsprung disease, but none of gastric perforation group had preceding gastrointestinal abnormality. A significant difference in NEC diagnosis (P<0.05) was seen between the two groups, with 11 cases in the intestinal perforation group only. None of gastric perforation infants were accompanied by NEC.
Abdominal distension was present in all cases, but bile-stained regurgitation was present in seven cases (56.3%) in the intestinal perforation group, a statistically significant difference compared to the gastric perforation group (P<0.05). The intestinal perforation group also demonstrated vomiting, diarrhea, gastrointestinal bleeding, and abdominal wall discoloration while patients in the gastric perforation group presented only with abdominal distension. One infant in the gastric perforation had discoloration of the abdominal wall and an increase in the gastric residual volume. Two had mild gastrointestinal bleeding via the orogastric tube.
The age at pneumoperitoneum diagnosis was 4.4±1.7 days of life (median, 4 days; range, 3-7 days) in the gastric perforation group, whereas the mean age of diagnosis in the intestinal perforation group was more variable and later in life at 10.8±11.2 days of life (median, 7.5 days; range, 2-39 days). Radiologic findings demonstrated sudden pneumoperitoneum without other prominent preceding clinical symptoms in the gastric perforation group, whereas the intestinal perforation group demonstrated ileus in the 24 hours preceding the pneumoperitoneum in nine cases (56.3%), which was statistically significant. Pneumatosis intestinalis was detected in three intestinal perforation cases. The mortality rate in the intestinal perforation group was 37.5%, whereas all patients with gastric perforation survived to discharge. This difference was not statistically significant (Table 3).
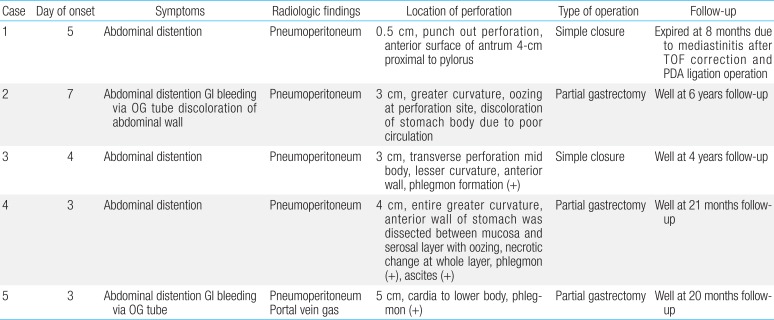
2. Case review of patients with gastric perforation
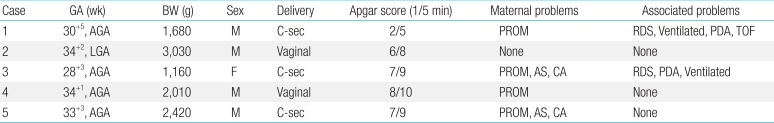
Gestation age of the gastric perforation group was 28+3-34+2 weeks (32+0±2.6 weeks) and the mean birth weight was 2,060±711 g. No infants in this group were born SGA. Male dominance was evident as four cases were males. Four cases were preceded by PROM, two cases were given antenatal steroids, and two cases had chorioamnionitis. Furthermore, two cases had RDS (cases 1 and 3), congenital heart disease, tetralogy of Fallot and hemodynamically significant PDA (cases 1 and 3), and meconium stained amniotic fluid (case 3), but three cases had no comorbid conditions (Table 4).
Gastric perforation occurred within the first week of life. All cases demonstrated abdominal distension. In the gastric perforation group, one infant (case 2) had discoloration of the abdominal wall, most likely due to a delay in diagnosis, as he was diagnosed at 7 days old. Another case had portal venous gas on the simple abdomen and abdominal ultrasonogram (case 5). In this patient, relatively large perforation (5 cm) was detected lower portion of stomach but there was no evidence of NEC by pathological finding.
All cases of gastric perforation underwent exploratory laparotomy on the day of diagnosis. Partial gastrectomy followed by primary closure was performed. The site of perforation was the greater curvature in two cases, lesser curvature in one case, antrum in one case, and cardia in one case. The length of perforation ranged from 0.5 to 5.0 cm.
All five patients with gastric perforation survived to discharge, although one patient died at eight months from postoperative complications after corrective operations for tetralogy of Fallot and PDA. The remaining four patients are undergoing follow-up at the outpatient clinic and are demonstrating optimal growth (Table 5).
Discussion
The incidence of pneumoperitoneum in newborns has not been reported but is thought to occur in 1%7) of patients admitted to the NICU. The review of our hospital data showed an incidence of 0.6%. Most gastrointestinal perforations are detected in the small intestine and colon with NEC as the most common underlying diagnosis. Other cases have been associated with distal bowel obstruction, mechanical ventilation, volvulus, and sepsis1). Gastric perforation in the newborn is thought to have a different pathogenesis than intestinal perforation. The etiology of gastric perforation has been reported from various perspectives; the congenital absence of muscle8), gastric ulcer with high acidity9), intestinal ischemia induced by asphyxia10), increased intragastric pressure from distal obstruction or aerophagia, and lack of C-KIT+mast cells or intestinal pacemaker cells1112). Elevation of intragastric pressure from immaturity and poor neurologic control in the newborn with uncoordinated vomiting from the dilated stomach is also thought to play a role13). In our study population, only two infants were ventilated and used an orogastric tube (cases 1 and 3). Those patients were on low pressure ventilation and the location of the orogastric tube was confirmed to be in the correct location by simple x-ray. In case 1, gastric perforation from ischemic injury could be the cause since the infant had low Apgar scores and cardiac anomalies (TOF and PDA), but we were not able to confirm this. The remaining three infants had no specific risk factors other than prematurity itself. Thus we speculate that the gastric perforation was spontaneous in most cases. The incidence of gastric perforation in the newborn is unknown. Leone Jr and Krasna14) reported an incidence of 7/84,000 newborns. The percentage of gastric perforation is thought to be 9%-10% among gastrointestinal perforations1). From our review of 20 years, we obtained a higher incidence (5/21, 23.8%) of gastric perforations, but this may be explained by the selection criteria for our study. We included only preterm infants who underwent exploratory laparotomy after being diagnosed with pneumoperitoneum. Male predominance in gastrointestinal perforation is well known, and our study confirmed this trend815). Whether gastric perforation is more common premature infants is controversial, but all of our cases occurred in the premature infant. We reviewed the literature for reports of gastric perforation in the newborn and, out of 153 cases reported, 70 cases (45.7%) were in preterm infants (Table 6).
Clinical symptoms of gastric perforation develop suddenly and are sometimes preceded by abdominal distension, ileus, or a decrease in bowel sounds. Other researchers have reported bile of blood stained vomiting, respiratory distress, dehydration, cyanosis, and shock as associated signs and symptoms. However, these signs and symptoms are general to all gastrointestinal perforations and, in our cases, sudden abdominal distension was the only specific clinical sign and symptom detected.
The time of diagnosis varies in the current literature. Most cases occur in the first week of life, especially in the first 3-4 days815). All of our cases occurred in the first week of life with a mean of 4.4 days. Miller9) reported that the gastric acidity in the newborn is highest in the first 24 hours of life and gradually decreases to the level of adults. Thus, the high acidity in the first week of life could explain the timing of gastric perforation in the newborn.
The most important diagnostic sign of gastric perforation is pneumoperitoneum on a simple radiograph. Gastric perforation in the newborn occurs suddenly, and the characteristic saddlebag or football sign may be evident from the vast amount of intraperitoneal gas816). Immediate exploratory laparotomy is needed, and partial gastrectomy and primary closure is the standard of care depending on the area of necrotic tissues.
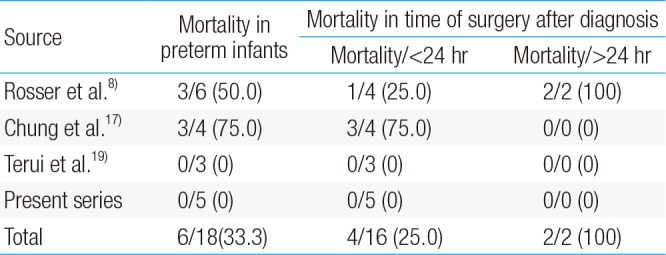
Gastric perforation in the newborn is associated with a high mortality rate of 25%-100%2815171819). The mortality rate is decreasing as a result of faster diagnosis, more aggressive management of the problem, and the advancement of neonatal practices. The time to operation from diagnosis seems to be significant factor associated with prognosis and mortality, confirmed by review of recent literatures (Table 7). In addition to, prematurity, low birth weight, the presence of associated conditions, and other associated anomalies are reported to be risk factors associated with poor prognosis and higher mortality215). All of our patients survived to discharge and have remained well through their most recent follow-up. We infer that this result was made possible by prompt diagnosis, absence of associated anomalies, and absence of comorbid conditions.
This is the first report comparing gastric perforation and other bowel perforation in preterm infant in Korea. We suggest that the differences of etiology and symptoms between gastric perforation and other bowel perforation were recognized and when a preterm infant presents with sudden pneumoperitoneum, gastric perforation should be ruled out. Prompt exploratory laparotomy will increase survival rate. Values are presented as mean±standard deviation (range) or number (%)
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.