Iron and vitamin D status in breastfed infants and their mothers
Article information
Abstract
Purpose
We assessed the relationships between iron and vitamin D statuses in breastfed infants and their mothers and evaluated the determinants of iron and vitamin D deficiencies in breastfed infants.
Methods
Seventy breastfed infants aged 4-24 months and their mothers participated in this study from February 2012 to May 2013. Complete blood counts, total iron binding capacity, and levels of C-reactive protein, iron, ferritin, calcium, phosphate, alkaline phosphatase, and 25-hydroxyvitamin D (25(OH)D) in infants and their mothers were measured.
Results
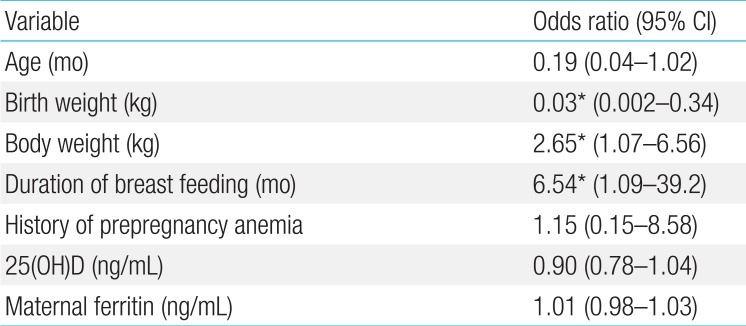
A history of maternal prepregnancy anemia was associated with lower ferritin and 25(OH)D levels in both infants and their mothers. The 25(OH)D level of infants correlated with maternal 25(OH) D levels. The independent risk factors for iron deficiency in breastfed infants were the duration of breastfeeding (odds ratio [OR], 6.54; 95% confidence interval [CI], 1.09-39.2; P=0.04) and infant body weight (OR, 2.65; 95% CI, 1.07-6.56; P=0.04). The determinants for vitamin D deficiency were the infant's age (OR, 0.15; 95% CI, 0.02-0.97; P=0.046) and maternal 25(OH)D level (OR, 0.74; 95% CI, 0.59-0.92; P=0.01).
Conclusion
A maternal history of prepregnancy anemia requiring iron therapy was associated with lower current ferritin and 25(OH)D levels in both infants and their mothers. Therefore, physicians should monitor not only iron but also vitamin D levels in infants who are breastfed by mothers who had prepregnancy anemia.
Introduction
There has been debate about the adequacy of the human milk for maintaining an ideal iron status and for providing other micronutrients in exclusively breastfed infants1). Given that maternal nutritional status affects the contents of breast milk, it can be hypothesized that the deficiency of iron and other nutrients in mothers may reduce the micronutrient stores in their infants.
It has been reported that infants born to anemic mothers have low iron stores and are more likely to develop anemia23). The American Academy of Pediatrics' (AAP) recommendations indicate that supplementation of oral iron drops before 6 months to breastfed infants may be needed to support iron stores4). However, several studies have shown that there is little correlation between maternal and neonatal ferritin concentrations56), and that maternal anemia does not affect breast milk iron or lactoferrin concentration at birth and during early lactation7).
Vitamin D stores in the fetus depend on maternal vitamin D status and breastfed infants continue to rely upon their mother's nutritional status. Previous studies have reported a high prevalence of Vitamin D deficiency (VDD) in breastfed infants8910), and AAP recommended that all breastfed infants routinely should receive an oral supplement of vitamin D, 400 IU per day, beginning at hospital discharge to maintain an adequate serum vitamin D concentration11).
A concurrent deficit of micronutrients, including iron and vitamin D, in breastfed infants may result in a wide spectrum of adverse effects on growth, development and performance12). However, the iron and vitamin D status of breastfed infants in relation to the status of their mothers has not yet been sufficiently evaluated.
This retrospective study was performed to investigate the relationships between the iron and vitamin D status of breastfed infants and their mothers and to evaluate the risk factors for iron deficiency (ID) and VDD in breastfed infants.
Materials and methods
Seventy breastfed infants aged 4 to 24 months and their mothers who visited Pediatric Department at the CHA Bundang Medical Center (Seongnam, Korea) were included in our study from February 2012 to May 2013. Exclusion criteria were (1) births at <35 weeks of gestation age or with low birth weight (≤2,500 g), (2) formula fed infants, and (3) mothers and infants who had taken micronutrient supplements including iron or vitamin D at enrollment.
Through the questionnaire, information about maternal history of pre- or postpregnancy anemia requiring iron supplementation, the pattern of menstruation after childbirth, maternal history of additional iron supplementation both during pregnancy and after delivery, the birth-related history, the duration of breast feeding and the weaning pattern were retrospectively checked. Additionally, laboratory test including the complete blood count, reticulocyte count, C-reactive protein (CRP), iron, total iron binding capacity, ferritin, calcium, phosphate, alkaline phosphatase, and 25-hydroxyvitamin D (25(OH)D) levels were performed both in infants and mothers. CRP was measured by high-sensitivity methods using an immunoturbidimetric assay. Serum ferritin was measured by chemiluminescence immunoassay. If the CRP level was greater than 0.3 mg/dL, we considered that serum ferritin had been affected by inflammation and as such excluded the ferritin data from statistical analysis (n=25). The serum 25(OH)D levels were measured by a radioimmunoassay kit from DiaSorin (Stillwater, MN, USA).
The infants were classified into iron deficiency anemia (IDA), ID, and normal groups. IDA was defined as hemoglobin (Hb)≤11 g/dL and ferritin≤12 ng/mL. IDA in infants with a CRP of more than 0.3 mg/dL was diagnosed as Hb≤11 g/dL with a mean corpuscular volume<70 fL and a transferrin saturation<16% (n=16). ID was defined as Hb>11 g/dL and ferritin≤12 ng/13). The maternal iron status was defined as ID if ferritin<50 ng/mL14). VDD was defined as 25(OH)D≤20 ng/mL, and vitamin D insufficiency (VDI) as 25(OH)D of 20-30 ng/mL15).
Data are expressed as means±standard deviations. The quantitative parameters of the groups were compared by t test. For comparing the 25(OH)D levels, we used analysis of variance to avoid interference by seasonal variation. Pearson correlation was performed to evaluate the relationship between the hematologic parameters and the 25(OH)D levels of infants and their mothers. Multivariable logistic regression was used to examine the influence of several variables on the iron and vitamin D status of breastfed infants. The PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. A P value < 0.05 and a confidence interval of 95% were considered statistically significant. This study was approved by the Institutional Review Board of the Medical Faculty at CHA University (BD 2014-0740).
Results
The demographic and clinical characteristics of our study participants are shown in Table 1. The average birth weight was 3.2±0.4 kg. Eleven infants (16%) were born between 35 and 37 weeks of gestation, and no one before 35 weeks. The number of mothers with prepregnancy anemia was 21 (30%). The number of mothers who had taken additional iron supplements during pregnancy was 34 (49%).
Among 70 infants, 81% (n=57) had VDD. In terms of iron status, 60% (n=42) in infants had IDA, 10% (n=7) had ID, and 30% (n=21) had normal. Infants with IDA and VDD were 53% (n=37). Among mothers, 89% (n=62) had VDD and only 1% (n=1) had IDA.
Mothers with history of anemia before pregnancy had lower ferritin level than those without (P=0.034) (Table 2). The level of 25(OH)D was significantly lower in infants and their mothers with history of prepregnancy anemia than in those without. There was no difference in ferritin and 25(OH)D levels of mothers and infants according to the history of iron supplementation during pregnancy (data not shown).

Hemoglobin, ferritin, and 25-hydroxyvitamin D levels in mothers and their infants depending on the history of prepregnancy anemia
The independent risk factors for ID or IDA in infants were body weight (P=0.04), and the duration of breast feeding (P=0.04) (Table 3).
The 25(OH)D levels of infants were significantly related with the maternal 25(OH)D levels (Fig. 1). By multivariable logistic regression, younger age and lower maternal vitamin D level were found to be independently associated with VDD (P=0.046 and P=0.01, respectively) (Table 4).
Discussion
Our data show that a maternal prepregnancy history of anemia was associated with lower current ferritin and lower 25(OH)D in both infant and their mothers. The duration of breast feeding was the independent risk factors for ID. Maternal vitamin D levels significantly affected the level of vitamin D in their infants.
It was reported that deficiencies of vitamins, iron, and zinc occur concurrently in lactating mothers and their infants in rural villages in Indonesia16). In recent years, breast feeding has become more common in Korea. A recent epidemiologic survey in 2009 showed that the overall breast feeding rate in Korea was 89.0% and the exclusive BMF rate at 6 months of age was 49.3%17). The concurrent VDD and IDA in infants have also been observed in recent Korean studies1819).
In this study, ferritin in mothers with prepregnancy anemia was significantly lower than in those mothers without a history of anemia. Neither maternal anemia nor prepregnancy history of anemia was related with ID in their infants. Several studies have shown that there is little correlation between maternal and neonatal ferritin concentration516). No correlation between maternal and neonatal ferritin level may come from the fact that breast milk iron concentration is usually consistent in various maternal iron status7). In lactating rats with different iron status, mammary gland transferrin receptors were inversely related to iron status20). It can be hypothesized that an anemic woman would have a large number of transferrin receptors in her mammary glands, to extract iron more efficiently from her serum.
More than half of breastfed infants had both VDD and IDA in the present study. In addition, the vitamin D of infants as well as mothers with prepregnancy anemia was lower than those without. Several possible mechanisms have been suggested to explain the association of VDD with anemia or ID in previous studies; ID decreased the levels of 1,25-dihydroxycholecalciferol in a rat model21). On the other hand, lower 25(OH)D levels were associated with an increased risk of anemia in a cross sectional study of 10,410 children and adolescents in the United States22). It was hypothesized that decreased calcitriol in bone marrow due to inadequate levels of 25(OH)D may limit erythropoiesis; calcitriol has a direct proliferative effect on erythroid burst-forming units that is synergistic with endogenously produced erythropoietin, and it also up-regulates expression of the erythropoietin receptor on erythroid progenitor cells23).
We found that lower birth weight or larger body weight increased the risk of ID. Previous studies have suggested that preterm or marginal low birth weight has a higher risk for ID, with smaller iron stores at birth and rapid growth24). An association between ID and overweight status has been observed in children2526). Several factors have been proposed to explain this association, including genetic influences, alterations in iron metabolism, inadequate diet, and increased growth and body surface area27). We also found that the longer the duration of breastfeeding without supplement of iron-forified food, the greater ID in breastfed infants. Previous studies have suggested that breastfed infants rarely show IDA during the first six months as long as a sufficient amount of breast milk is provided, because the iron transferred through breast milk has high bioavailability2829). The declining Hb and serum ferritin of infants beyond six months may be attributable to the normal depletion of iron stores not balanced by the exogenous supply of iron and the decline in the bioavailability of breast milk iron and the lactoferrin concentration30).
The close correlation between the vitamin D levels of infants and their mothers found in this study was also observed in previous research31). About 20% of maternal vitamin D is delivered through milk to the infant. A high prevalence of maternal VDD during lactation could contribute to VDD in exclusively breastfed infants32). In a study from Finland, it was found that an adequate supply of vitamin D in breast milk for breastfed infants could be accomplished only by increasing maternal vitamin D3 supplementation to 2,000 IU/day33). Recent studies have also shown that higher dose maternal vitamin D supplementation during lactation at 6,400 IU/day substantially increases vitamin D levels in mothers and infants without adverse effects34).
We found that the risk of vitamin D deficiency decreases with age in infants. It can be hypothesized that outdoor activities are increased with age, resulting in a positive effect on the cutaneous production of vitamin D.
The limitations of our study include its small number of subjects and the fact that this is a hospital-based study with possible selection bias. In addition, there was a lack of maternal medical record information including details of the amount of bleeding and the time of cord clamping at delivery as well as the socioeconomic data for our study group. There were also problems related to analyzing the ferritin level in infants who might have had inflammation without elevated CRP. Laboratory tests such as hepcidin, principal regulator of iron homeostasis to regulate iron transport across the gut mucosa, might be necessary in this situation35).
In conclusion, the maternal prepregnancy iron status and current maternal vitamin D has an effect on vitamin D of their breastfed infants. The prevalence of ID in infants significantly increased with the duration of breast feeding. Therefore, it is needed to concern about vitamin D as well as iron in breastfed infants with maternal prepregnancy anemia. In addition, a prospective research with a large number of subjects is needed to clarify micronutrient needs in pregnancy and during lactation for breastfed infants.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.