Virtual, augmented, and mixed reality: potential clinical and training applications in pediatrics
Article information
Abstract
Background
COVID-19 pandemic has significantly impacted the field of medical training, necessitating innovative approaches to education and practice. During this period, the use of novel technologies like virtual reality (VR), augmented reality (AR), and mixed reality (MR) has become increasingly vital. These technologies offer the advantage of transcending the limitations of time and space, thus enabling medical professionals to access various personalized programs for both education and service delivery. This shift is particularly relevant in the realm of pediatric medicine, where traditional training and clinical methods face unique challenges.
Purpose
The primary aim of this study is to explore the application of VR, AR, and MR technologies in pediatric medical settings, with a focus on both clinical applications and the training of pediatric medical professionals. We aim to comprehensively search and review studies that have utilized these technologies in the treatment of pediatric patients and the education of healthcare providers in this field.
Methods
Peer-reviewed articles published in PubMed, the Cochrane Library, ScienceDirect, Google Scholar, and Scopus from January 1, 2018, to March 1, 2023, were comprehensively searched. The review was conducted according to the PRISMA (Preferred Reporting Items for Systematic review and Meta-Analyses) guidelines. Among the 89 studies, 63 investigated the clinical applications of VR (n=60) or AR (n=3) in pediatric patients, and 25 investigated the applications of VR (n=19), AR (n=5), or MR (n=1) for training medical professionals.
Results
A total of 36 randomized controlled trials (RCTs) for clinical application (n=31) and medical training (n=5) were retrieved. Among the RCTs, 21 reported significant improvements in clinical applications (n=17) and medical training (n=4).
Conclusion
Despite a few limitations in conducting research on innovative technology, such research has rapidly expanded, indicating that an increasing number of researchers are involved in pediatric research using these technologies.
Key message
· Review of articles that investigated the applications of virtual, augmented, or mixed reality in pediatric clinical settings and in the training of pediatric medical professionals was conducted.
· A total of 89 studies were retrieved, with 36 randomized controlled trials.
· In most studies, intervention using the novel technology was at least as effective or more effective than the traditional method.
· Use of virtual, augmented, and mixed reality has potential in pediatrics.
Graphical abstract. The review includes the applications of new technologies for medical services targeting pediatric patients and training methods for medical professionals. There are programs designed to reduce children’s pain, anxiety, and fear during in-hospital treatment (left), and medical staff’s education for child patients (right).
Introduction
In the healthcare industry, virtual reality (VR), augmented reality (AR), and mixed reality (MR) are being extensively used for various purposes [1]. Digital technology, with its pervasive use and relentless advancement, is considered a promising source of effective and efficient training and education for health professionals [2]. In particular, the integration of digital strategies has led to a paradigm shift in healthcare education [3]. Furthermore, the research results demonstrate the ability of VR, AR, and MR to ameliorate the inconveniences often associated with traditional medical care; reduce the number of incidents of medical malpractice caused by unskilled operations, and decrease the cost of medical education and training [4]. Moreover, higher acceptance of the latest technologies by children can render new technologies more easily applicable to them than to older populations [5], and help increase treatment compliance in pediatric populations that have a lower understanding of the disease and treatment within the traditional medical care setting [6].
Differentiation between VR, AR, and MR is important for proper analysis of the field, and VR is the use of computer modeling and simulation, which enable a person to interact with an artificial three-dimensional visual or other sensory environment [7]. It immerses the user by making them feel as if they if they are experiencing simulated reality first, primarily by stimulating vision and hearing in real-time [8]. The two primary features of VR are immersion and interaction. Immersion refers to the sense of presence in a virtual setting and interaction, which involves the operator’s ability to modify performance [9]. By contrast, AR superimposes a computer-generated virtual element on existing to enhance sensory sensory perception [10]. MR is the merging of real and virtual worlds to produce new environments and visualizations in which physical and digital objects coexist and interact in real-time. MR is not confined exclusively in either the physical or the virtual world [11].
To date, most reviews have focused on research using VR, AR, and MR technologies in adults [12]. Therefore, this study has focused on pediatric research, aiming to map the literature on the clinical applications of VR, AR, and MR technologies for pediatric patients and the training of pediatric medical professionals [13,14].
Methods
This study was conducted in accordance with the Preferred Reporting Items for Systematic review and Meta-Analyses (PRISMA) guidelines [15]. A meta-analysis was not possible due to the heterogeneity of the publications. It was conducted by two independent reviewers with diverse academic backgrounds to ensure inter-rater reliability and comprehensive coverage of various research perspectives on VR, AR, and MR applications.
1. Data source, search strategy, and inclusion and exclusion criteria
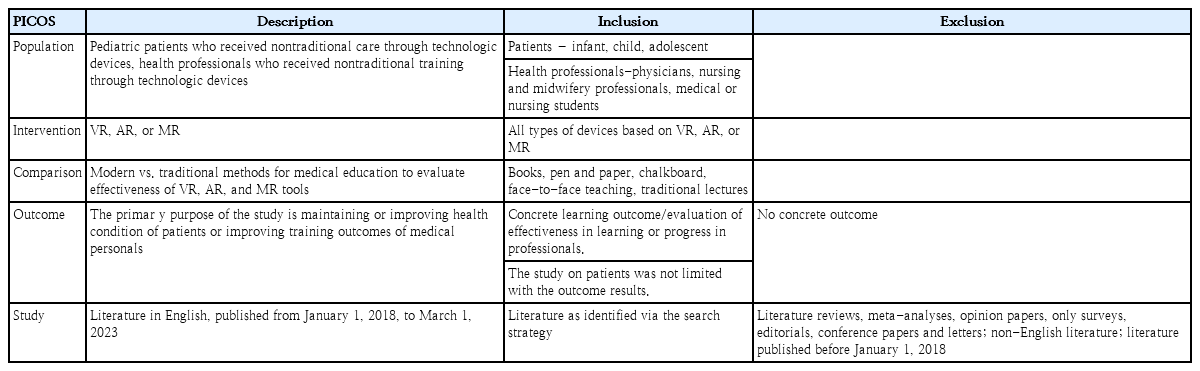
The initial search was conducted on March 1, 2023, using six electronic databases: PubMed, Cochrane Library, ScienceDirect, Google Scholar, ERIC, and Scopus. The WorldCat database was searched [16], and 105 papers obtained using three search keywords: VR, AR, and MR. The following search terms or keywords were used in combination: pediatric, virtual reality, augmented reality, mixed reality, practice, training, and education (Supplementary Table 1). To identify detailed search terms, we used the PICOS (population, intervention, comparison, outcome, study design) search strategy (Table 1) [17-19]. Publications were only included if they were published between January 1, 2018, and March 1, 2023, and restricted to English. Papers published in peer-reviewed journals were included; surveys, editorials, conference proceedings, and letters were excluded, as were literature and systematic reviews that that lacked an abstract or full text were excluded. The analytical PRISMA flowchart was used for screening (Fig. 1) [20].
2. Eligibility criteria
A 2-stage screening process was utilized to assess the relevance of studies identified in the search [21]. Studies on VR, AR, or MR applications for education, training, or practice in pediatric departments were included and screened to identify and characterize the subjects and objects of the studies. When the same data was reported in multiple publication (for example, in journal article or electronic report), only articles reporting the most comprehensive datasets were used.
3. Data extraction and study quality assessment
Supplementary Table 1 presents a comprehensive outline of the study selection process employed in this scoping review. The initial search yielded a total of 18,963 articles, of which 218 were identified as duplicates and were subsequently excluded. Among the remaining 18,745 articles, 17,660 were deemed ineligible for inclusion based on the criteria applied through automated tools. additionally, any non-English language papers were excluded. Consequently, 2 authors independently evaluated the identified studies, ensuring adherence to the predetermined inclusion and exclusion criteria primarily through the examination of titles and abstracts. As a result, 157 out of the initial pool of 1,085 studies were selected for further analysis. Subsequently, both authors independently screened the full texts of these selected articles. Any discrepancies or conflicts that arose during this screening process were resolved through discussions between the 2 screening authors. Relevant characteristics were extracted from the included studies, encompassing information such as authorship, publication year, journal sources, countries of study, study designs, evaluation methods, number of evaluation methods employed, types of data analysis, effectiveness outcomes, study population characteristics, medical disciplines under investigation, type of learning approaches utilized, study durations, and references used [22,23]. Other reasons for exclusion, detailed in Supplementary Table 1, included but were not limited to studies focusing on a different age group or those not involving pediatric patients. Consequently, the final selection comprised 89 studies deemed suitable for inclusion in this scoping review.
Results
The review incorporated a total of 89 studies, in which the utilization of VR, AR, and MR technologies was observed in 80, 8, and 1 study, respectively. All included studies were conducted within academic or hospital settings and predominantly focused on comparing VR or AR environments with conventional clinical applications or traditional face-to-face training methods [24].
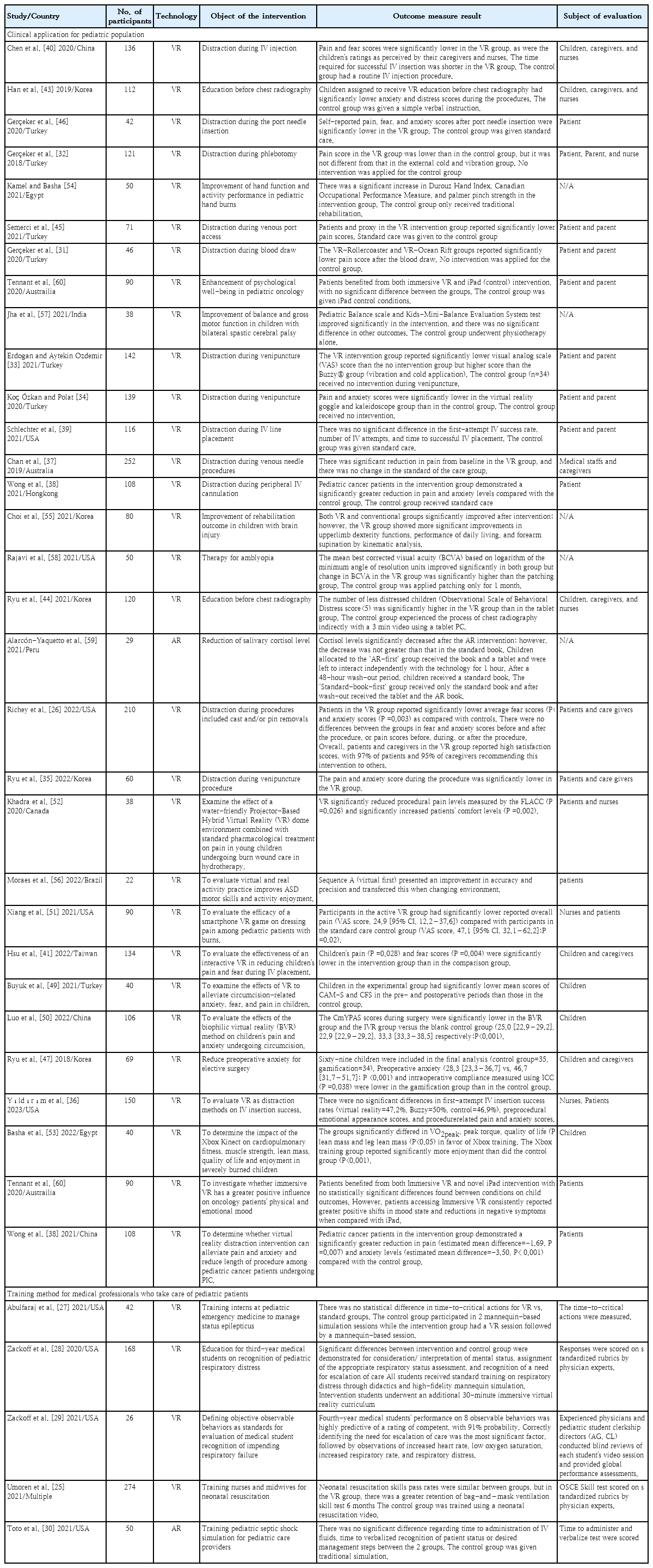
The scoping review revealed that the mean sample size of participants in the reviewed publications was 62.69, with a standard deviation of 55.20. Among the total studies, 25 articles (28.08%) reported a participant pool exceeding 80 individuals. Furthermore, 32 studies (35.95%) were conducted in the United States, with a significant number of studies originating from Korea (10 studies) and Turkey (9 studies), as specified in Table 2.
1. Object of the study
Out of the 89 studies included in the scoping review, a total of 64 focused on the clinical applications of VR (n=61) or AR (n=3) in pediatric patients. Additionally, 25 studies examined the utilization of VR (n=19), AR (n=5), or MR (n=1) in the training of medical professionals or students.
The 89 studies included in the scoping review were classified into five primary categories: clinical assessment or management, patient treatment, educational skills, educational knowledge, and practical educational attitudes. Among these, 38 studies specifically addressed clinical assessment or management, focusing on aspects such as patient pain and anxiety. Additionally, 24 studies explored patient treatment, encompassing rehabilitation and other medical care approaches. Education skills were the focus of 16 studies, targeting both patients and medical staff. Furthermore, educational knowledge was examined in six studies, while five studies delved into practical educational attitudes.
A total of 36 randomized controlled trials (RCTs) were analyzed in the scoping review, with 31 studies focusing on clinical applications and 5 studies focusing on medical training. The majority of the RCTs utilized VR (n=34) as the intervention, except for 2 studies [25,26], that employed AR.
The scoping review included a variety of studies that focused on training methods for medical professionals in pediatric care. These studies covered a range of topics, including managing epilepsy [27], recognizing childhood conditions involving difficulty in breathing [28,29], providing neonatal resuscitation education [25], and offering septic shock simulation training [30].
The aim of the major clinical study was to alleviate fear, pain, and anxiety experienced by children during invasive procedures such as blood drawing [31], phlebotomy [32], and venipuncture [33-35]. Intravenous injection [36-41] PIVC insertion [42], chest radiography [43,44], and port needle insertion [45,46] in pediatric patients. Some studies also focused on surgical fear, such as pre- or postoperative scenarios [47,48] and circumcision [49,50]. Serve various purposes, such as enhancing rehabilitation capabilities with distraction techniques in burned patients [47,51-54], physical rehabilitation [55-57], therapy for amblyopia [58], psychological well-being [59,60], and stress reduction during orthopedic cast room procedure [26].
Within the realm of clinical applications, the primary objective across studies was to alleviate pain and anxiety in pediatric patients through the implementation of distracting interventions during medical procedures. Nine of ten researchers reported the intervention as effective in reducing pain or anxiety experienced during painful procedures. In medical training settings, four studies employed VR and 1 study utilized AR [30] implementing scenario-based learning approaches in diverse clinical settings for medical students, nurses, and interns. Detailed information regarding the 36 RCTs can be found in Table 3. The scoping review also included a variety of studies that focused on training methods for medical professionals in pediatric care. These studies covered a range of topics, including managing epilepsy [29], recognizing childhood conditions involving difficulty in breathing [27,28], providing neonatal resuscitation education [25], and offering septic shock simulation training [30].
2. Evaluation methods
Of the 89 identified studies, the majority (n=69, 77.52%) used a quantitative study design, followed by mixed methods (n=14, 15.73%) [61-74], and a small number of studies utilized a qualitative study design (n=6, 6.74%) [24,75-79].
The findings of the scoping review indicated a preference for objective measurement and data analysis methods in the included studies. Qualitative studies focused on exploring the subjective experiences and perceptions of the participants, while mixed-method studies utilized both quantitative and qualitative data collection and analysis techniques to provide a more comprehensive understanding of the investigated topic.
In contrast to other classification standards that solely rely on factors such as country, year of publication, and effectiveness, the present evaluation method employed multiple evaluation techniques. Across the 89 studies, a total of ten evaluation methods were utilized to assess the effects of VR, AR, and MR interventions. These evaluation methods encompassed skills tests, surveys, recordings, knowledge tests, interviews, observations, self-assessments, measuring tools, physical assessments (including vital signs and cortisol levels), and counting by standard (e.g., time and count). Each evaluation method was counted separately, even if it was utilized in multiple studies. As a result, a total of 244 evaluation methods were identified within the 89 studies included in the analysis.
Among the evaluation methods used, 14 studies (5.74%) employed skills tests, while 22 studies (9.02%) utilized questionnaires. Recordings were employed in a single study, accounting for 0.41% of all evaluations. Knowledge tests were employed in 13 studies (5.33%), interviews in 20 studies (8.2%), observations in 20 studies (8.2%), and self-assessments in 18 studies (7.38%). Measuring tools were employed in 79 studies, representing 32.38% of the evaluations. Physical assessments, including vital signs, length of stay, and cortisol levels, were utilized in 34 studies, accounting for 13.93% of the evaluations. Counting by standard, such as measuring time or count, was employed in 23 studies, representing 9.43% of the evaluations.
The measuring tools used in the studies encompassed the evaluation of children's anxiety, enjoyment, and fear during magnetic resonance imaging on a ten-point scale, as well as the use of verbal evaluation tools to assess anxiety in children with concerns about academic achievement. Studies evaluated through observation involved experts or experienced evaluators determining the educational effects of VR devices through observation, or guardians and medical staff evaluating children's pain, distraction, and social behavior. Questionnaire-based evaluations involved medical staff, parents, and guardians providing assessments of fear and loneliness in children receiving inpatient care, or medical staff with training and experience in device usage evaluating feasibility and usability through questionnaires.
3. Effectiveness of the applied methods
Out of the 89 studies included in the review, a significant majority of 80 studies (89.8%) reported the effectiveness or partial effectiveness of VR or AR interventions. Among these, 65 studies (73.03%) reported full effectiveness, while 15 studies (16.85%) reported partial effectiveness. Four studies recognized the utility of VR or AR devices as supplementary tools. However, five studies either did not report the effectiveness of the interventions or did not observe any significant differences between the experimental groups [29,62,67,69,80].
Among the 65 studies deemed effective, various evaluation methods were employed. Measurement tools were utilized in 20 studies, observations in 11 studies, knowledge tests in ten studies, and skill tests in nine studies. Notably, out of the effective studies, 18 focused on evaluating the impact of VR and AR interventions on medical staff, while 47 studies assessed their effectiveness in pediatric patients.
However, it is important to acknowledge that despite most studies reporting positive effectiveness, there were limitations to the research. Specifically, four studies indicated a lack of conclusive evidence regarding the effectiveness of VR and AR interventions, highlighting the necessity for further investigation in this area.
4. Devices
A comprehensive analysis of the studies revealed that a total of 78 devices utilized across the various research investigations. The most frequently employed device was the Oculus Rift, which featured in 19 studies, accounting for 24.36% of the total. The Samsung Gear VR ranked second, utilized in 7 studies (8.97%). Other frequently employed devices included the HTC VIVE Cosmos Elite, HoloLens, and Oculus Go, each utilized in three studies (3.85%). Additionally, several studies incorporated a combination of devices including the Oculus Rift Touch, Oculus Rift DK2, Google Daydream, MediqVR, and RAPAEL Smart Kids.
However, a significant portion of the devices used in the studies was not specifically identified in the provided list. Seven studies did not mention the name of the device, while 11 entries simply referred to the device as a "monitor," "smartphone," or "tablet." These unspecified devices accounted for 17.95% of the total number of devices employed in the studies.
Discussion
The utilization of VR, AR, and MR technologies is extending beyond their traditional recreational and gaming applications and finding increased usage in various domains, including the medical field. This scoping review specifically examines the application of VR, AR, and MR technologies in pediatric research. The review was conducted by a team comprising two researchers and one pediatrician, employing a methodology akin to that used in previous review papers.
The field of pediatrics has witnessed the undertaking of diverse and significant studies. In contrast to studies focusing on adult patients, which extensively employ VR, AR, and MR technologies to assist in treatment, numerous studies have focused on providing supportive care to alleviate pain and anxiety in children. Children, due to their comparatively limited understanding of their disease and treatment processes, often exhibit lower treatment compliance [71]. Moreover, the experience of pain and fear in children can induce excessive stress in patients, guardians, and medical staff, potentially resulting in treatment refusal. These factors not only subject children to considerable stress but may also lead to decreased sociability and feelings of alienation. Accordingly, most studies have endeavored to address these specific challenges and characteristics associated with children.
Moreover, the evaluation of research effects in the context of pediatric patients presents distinct challenges. Due to the nature of pediatric patients, it is relatively difficult to employ devices, patient self-reports, and standardized evaluation indices for evaluating research outcomes. Consequently, studies in this area have primarily relied on evaluations conducted through the observation of medical staff or guardians. It is plausible that these factors have influenced researchers to employ observational evaluations by guardians or medical staff more frequently as a means of assessing the outcomes of interventions in pediatric populations.
These technologies are also used in various fields to train medical staff in performing medical activities involving children. Education employing VR, AR, and MR devices can provide an immersive environment that surpasses traditional approaches such as books or person-to-person training, thereby overcoming time constraints, preventing ethical concerns, and offering nearly unlimited practice opportunities. This not only represents a new paradigm for educational methods but also sees VR, AR, and MR applied as educational evaluation tools, either replacing or supporting existing evaluation systems.
Similar to reviews of studies involving adult populations, a majority of the research in this domain has been conducted in a few countries, particularly the United States. This trend can be attributed to the nature of the research, which necessitates the use of cutting-edge devices and is influenced by device availability. Furthermore, most studies have primarily focused on VR, reflecting the stage of technological development and research conducted thus far. In comparison with other clinical studies, the majority of studies reviewed here evaluated interventions after a relatively brief application period. Moreover, most studies assessed the effectiveness of training interventions following a short duration ranging from a day to a month.
Among the 5 studies that utilized VR and AR for medical staff education, three confirmed the effectiveness of interventions in enhancing objective competence in assessing respiratory distress and recognizing the need for escalated care for patients [28], and standards for assessment of entrustable professional activity attainment [27] and neonatal resuscitation skills [25]. Two studies showed no significant difference in time-to-critical actions for VR verus standard groups [29], and no difference in primary outcomes, but only in secondary outcomes [30]. This does not imply that learning with VR, AR, or MR is less effective than traditional learning methods. However, comparing and assessing the learning effects of novel devices based solely on a short duration of experience can be challenging.
Furthermore, environmental constraints may impede the smooth utilization of new technologies and hinder the determination of their effectiveness in educational settings. Despite certain limitations inherent in conducting research on innovative technologies, such research has experienced rapid expansion after 2020, indicating an increasing involvement of researchers in pediatric research employing these technologies. Furthermore, given that most studies have reported positive self-contained effectiveness, further studies pertaining to this subject should be pursued. The realm of research involving VR, AR, and MR devices for pediatric patients and medical professionals is expected to expand to encompass a variety of clinical and training purposes.
Supplementary materials
Supplementary Table 1 can be found via https://doi.org/10.3345/cep.2022.00731.
The combinations of search terms used in each database
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contribution
Conceptualization: MHS; Data curation: YS; Formal analysis: YS, Funding acquisition: MHS; Methodology: MHS; Project administration: MHS; Visualization: HHH; Writing-original draft: YS; Writing- review & editing: MHS
Acknowledgements
We are grateful to HI Jung for her assistance in searching for and processing the data, and HH Hwang for illustrating the graphical abstract.