Incidence, causative organisms, and risk factors of bloodstream infections in pediatric liver transplant patients: a systematic review
Article information
Abstract
Bacterial bloodstream infections (BSI) are the leading cause of mortality and morbidity in pediatric solid organ transplant recipients. This systematic review aimed to pool global data from leading transplant institutions and identify the overall incidence, risk factors, and causative organisms of BSI in pediatric liver transplant recipients. A systematic review of the PubMed and OVID databases was conducted from 2000 to 2022. The initial search yielded 252 unique articles, which were independently reviewed by 2 authors. Articles that reported pediatric-specific data on BSI in isolated liver transplant patients were included, including the incidence of BSI, isolated organisms, and involved risk factors involved. This systematic review was registered with PROSPERO (ID: CRD42023403206). Fourteen articles from the United States, France, Iran, Japan, Korea, South Africa, Thailand, and Turkey were included. A total of 4,812 liver transplants were included in the final analysis. The mean patient age was 25 months (age range, 0–18 years), and 50.9% were male. The overall incidence of BSI was 23.5% (range, 14.7%–55%). The most commonly reported organisms were Staphylococcus epidermidis, Enterococcus, Klebsiella spp., and Escherichia coli. Among the risk factors studied, postope rative biliary complications, a medical history of biliary atresia, and younger age were the risk factors most commonly associated with BSI. Bacterial BSI after pediatric liver transplantation occur at a high incidence, with a unique organism profile notable for a higher percentage of gram-negative organisms. Further studies are required to de-termine the most appropriate prophylactic and empirical antibiotic management strategies for this population.
Key message
The overall incidence of bloodstream infections was 23.5%. Gram-negative organisms occur at a much higher rate in pediatric liver transplant recipients then that the general pediatric population. However, when comparing pediatric and adult liver transplant recipients Gram-positive organisms occur with a much higher rate in the pediatric population highlighting the importance of early and broad spectrum antimicrobial coverage when bloodstream infections are suspected.
Introduction
Liver transplantation (LT) is an effective and life-saving procedure for patients with end-stage liver disease. According to the United Network of Organ Sharing, 5,167 liver transplants were performed through July 2023 in the United States (US) alone, a dramatic increase over the past several years [1]. The Society of Pediatric Liver Transplantation reported that biliary atresia (38.5%) is the most common indication for LT in children in the US, followed by metabolic diseases, tumors, and fulminant liver failure [2].
The Centers for Disease Control and Prevention defines bloodstream infections (BSI) as blood cultures growing a recognized non-commensal bacterial or fungal organism not related to an infection at another site or the presence of at least one clinical sign (fever, chills, or hypotension) alongside 2 separate blood cultures growing the same organism [3].
Despite rapid advances in surgical techniques, antibiotic prophylaxis, immunosuppressive regimens, and infection control protocols, BSI remains an important cause of morbidity and mortality in pediatric LT recipients, with reported incidences of 38%–65% [4-6]. This could be attributed to frequent and prolonged hospitalizations along with the need for indwelling catheters, such as central venous catheters [7]. Moreover, the use of immunosuppressive medications has the dual effect of mitigating rejection rates while increasing the risk of infection [7].
Considering the heavy burden of BSI, understanding the spectrum of involved organisms is essential for choosing prophylactic and empirical antimicrobials, especially in the context of the global threat of antimicrobial resistance. The causative bacterial organisms vary among different patient subgroups based on their underlying morbidities, and pediatric LT recipients present unique risk factors for BSI. In addition, the transplant institutions included in this systematic review selected different antimicrobial regimens based on the rate of BSI and specific organisms encountered at each center. Although bacterial pathogens are the most common cause of BSI [8], fungal organisms have been reported to occur at rates of 5%–42% in LT recipients [9,10], with a mortality rate as high as 80% [11].
To the best of our knowledge, there have been no systematic reviews on BSI post-LT in an evidently vulnerable pediatric population. We performed a systematic review of published studies to determine the incidence, organisms involved, and risk factors for BSI in pediatric LT recipients.
Methods
1. Data sources and search strategy
A systematic review was performed according to the 2015 Preferred Reporting Items for Systematic Reviews on Meta-Analyses 2015 guidelines [12]. Two reviewers (MS and RH) independently identified relevant studies through an electronic search of the PubMed and OVID databases from inception to May 2023. The following search terms and keywords were used: BSI, sepsis, liver transplant, and LT. This systematic review was registered in the International Prospective Register of Systematic Reviews (No. CRD42023403206).
2. Study selection
Two reviewers (MS and RH) independently assessed study eligibility based on title, abstract, and full-text report reviews. Eligible studies included information about the prevalence, risk factors, and involved organisms in BSI in pediatric LT recipients (0–21 years of age). The exclusion criteria were as follows: (1) pediatric cases not reported separately in studies including adults; (2) duplicate publications; (3) studies on patients with multivisceral transplantation; and (4) reviews, editorials, letters, and nonhuman studies. Only studies published in English were included in this systematic review.
3. Data extraction and quality assessment
Two investigators (MS and RH) independently extracted the data (prevalence, organisms, risk factors reported, demographics, indications for LT, and antimicrobial prophylactic medications used) using a standardized data abstraction form. Study methodological quality was assessed systematically using the Newcastle-Ottawa Scale for Observational Studies.
4. Outcome measures
The coprimary outcomes for study selection were the prevalence, organisms, and risk factors for BSI in LT patients. The indications for LT and prophylactic antimicrobial agents used were the secondary outcomes.
Results
1. Demographics and final article selection
The initial database search identified 276 studies, of which 24 were duplicates and 3 were not retrievable and, therefore, excluded. Following the screening of titles and abstracts against the inclusion and exclusion criteria, 17 full-text reviews were performed, of which 3 were excluded. Finally, 14 full-text studies were included in this systematic review (Table 1) [5,13-25]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for the study search and selection process is displayed in Fig. 1.
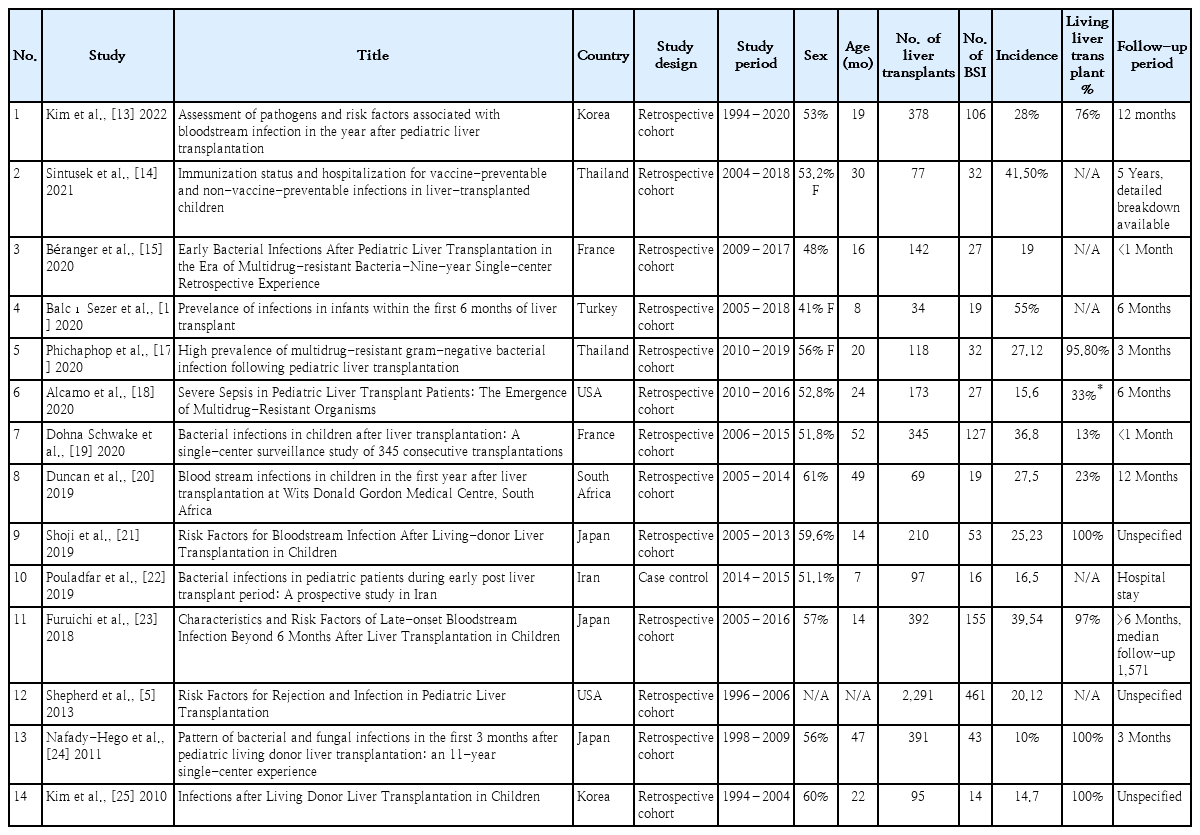
Detailed breakdown of included studies, patient demographics, incidence of bloodstream infections (BSI), and follow-up period
PRISMA (Preferred Reporting Items for Systematic Reviews on Meta- Analyses) flow diagram summarizing the study screening process.
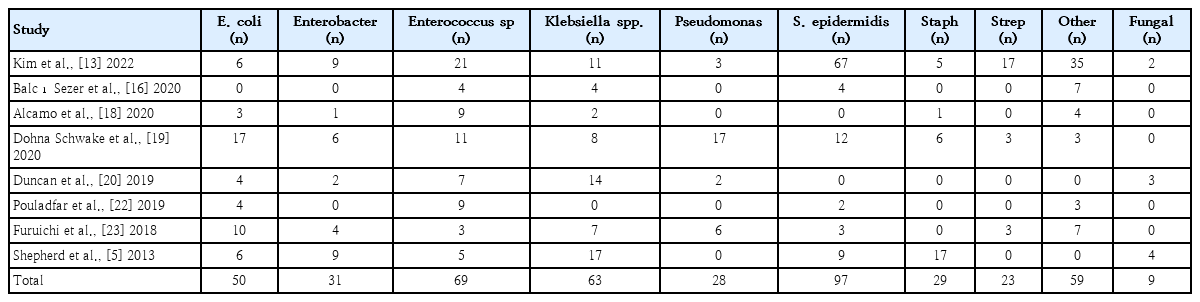
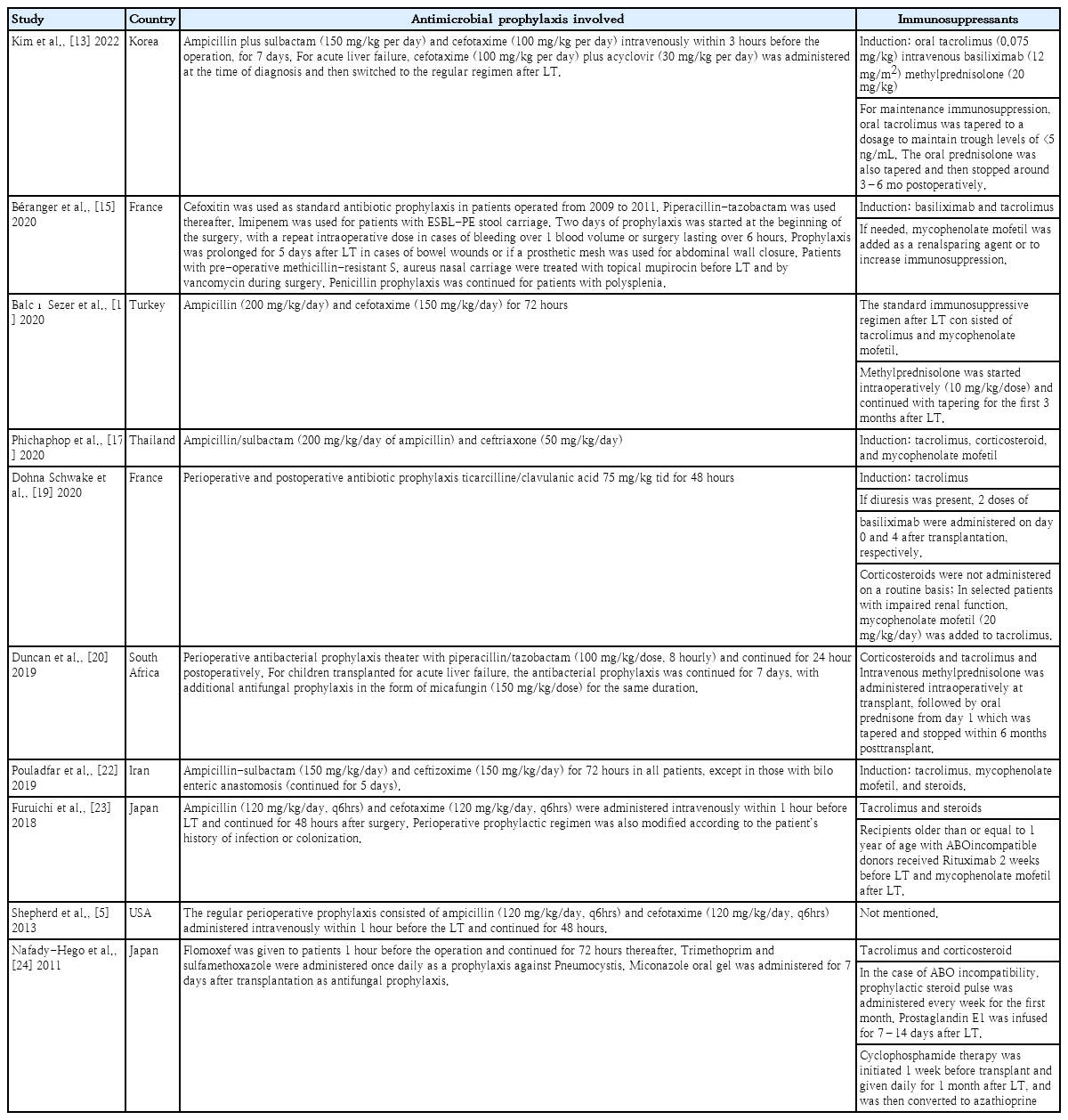
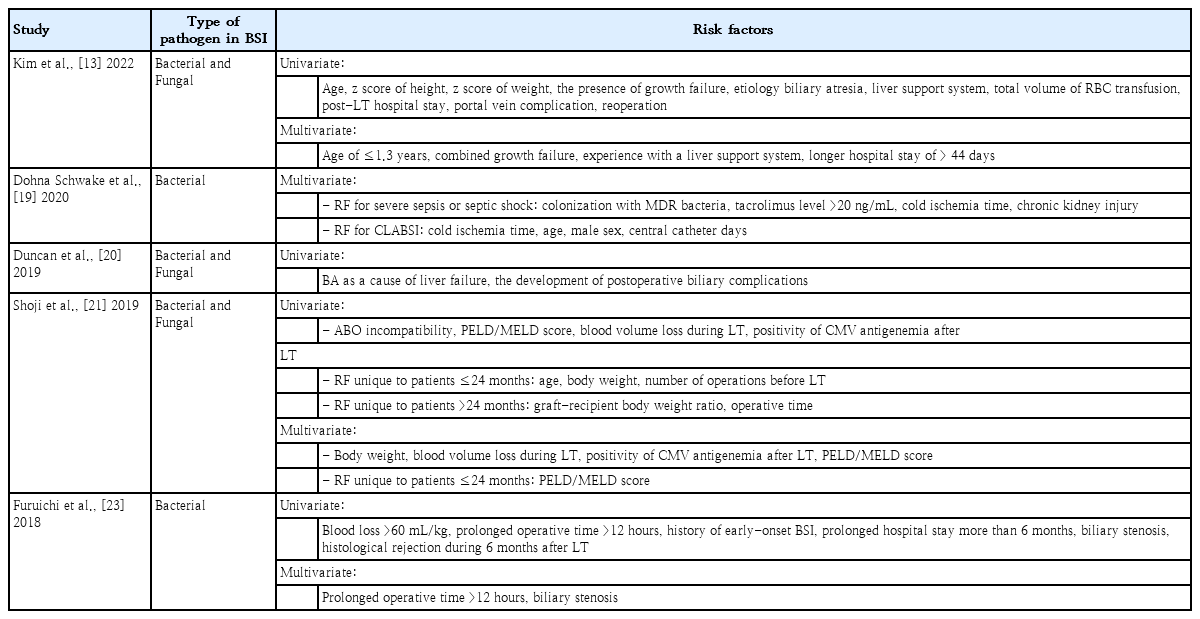
In this review, 13 retrospective cohort studies and one case control study were included for a total of 14 studies from France, Iran, Japan, Korea, South Africa, Thailand, Turkey, and the US. The extracted data included the BSI rates (Table 1), organisms identified (Table 2) [5,13,16,18-20,22,23], prophylactic antibiotics used (Table 3) [5,13,15-17,19,20,22-24], and risk factors (Table 4) [13,19-21,23]. The patient population comprised 50.9% males (n=1,283), with a mean age of 25 months. A total of 4,812 LT were performed, 68% (n=1,481) of which were from living donors. The most common indications for LT were biliary atresia, inherited or intrinsic liver problems, and metabolic disorders (Fig. 2).
2. Incidence of BSI
The incidence of BSI in the combined population was 23.5% (range, 14.7%–55%)(Fig. 3).
3. Organisms identified in cases of BSI
Gram-positive bacteria accounted for 59.5% of BSI cases, with Staphylococcus epidermidis and Enterococcus spp. being the leading causative agents. The most commonly identified gram-negative pathogens were Klebsiella spp. and Escherichia coli (Fig. 4, Table 2).
4. Antimicrobial prophylaxis and immunosuppressants used
Considering the different institutes from across the globe included in this review, there were differences in the choice of perioperative prophylactic antibiotics and their doses. The most common prophylactic antibacterial agents used were ampicillin, ampicillin-sulbactam, piperacillin-tazobactam, and cephalosporins. Regarding antifungals, most institutions started fluconazole postoperatively, with a few notable exceptions, such as micafungin in the South African study reported by Duncan et al. [20] (Table 3).
The immunosuppressants tacrolimus and methylprednisolone were administered universally during the induction phase. Other agents with different efficacies include basiliximab, mycophenolate mofetil, and azathioprine (Table 3).
5. Identified risk factors for BSI
Although many studies have reported the risk factors for infections post-LT, only those listed in Table 4 specifically detailed the risk factors for BSI. Risk factors can be divided into 3 categories: preoperative (e.g., age, biliary atresia as the underlying indication, Pediatric End-Stage Liver Disease/Model for End-Stage Liver Disease [PELD/MELD] score, weight/height/growth failure, colonization with multidrug-resistant organisms, use of a liver support system), intraoperative (e.g., operative time, biliary and portal vein complications, blood volume lost and transfused, cold ischemia time, need for reoperation, ABO incompatibility), and postoperative (e.g., central catheter time, length of stay, and histological rejection).
Discussion
Here we conducted a systematic review to examine the incidence, risk factors, and causative organisms of BSI among pediatric patients following LT worldwide. Our key findings were as follows:(1)the global incidence of BSI in LT patients was 24.61%; (2) the most common organisms were S. epidermidis, Enterococcus spp., and Klebsiella spp.; and (3) the most common risk factors identified were younger age at the time of LT, volume of blood loss, and medical history of biliary atresia.
Indications for LT in the pediatric population (Fig. 2) differ from those in adults. As highlighted in a review by Graziadei et al. [26] the most common indications for LT in adults include nonalcoholic steatohepatitis, alcoholic liver cirrhosis, and chronic hepatitis C. The underlying etiology plays a role in the prognosis of LT, as shown by Kim et al. [13] and Duncan et al. [20], which further emphasizes the importance of studying pediatric populations independently.
This review demonstrated that the incidence of BSI varies greatly among participating transplant centers (Fig. 3), which may be due to specific patient care-related factors (i.e., infection control measures, antimicrobial prophylaxis used) or to study-related factors (i.e., sample size, selection, and other potential biases). For example, while BSI prevalence was the highest in Turkey, it is important to note the small population in the Turkish study of 34 LT recipients; therefore, this may not reflect an accurate measure.
Other potential explanations for this variation include the use of different antimicrobial prophylactic regimens. France had the second highest incidence of BSI among the analyzed studies. Interestingly, the center in France relied on cefoxitin monotherapy from 2009 to 2011, which did not cover Enterococcus spp. and Pseudomonas spp., both of which are frequently isolated organisms.Additionally, donor population plays an important role in the risk of BSI. It is noteworthy that the study from Japan involved 97%–100% living donors, which is classically associated with fewer postoperative complications and better outcomes. The reported rates must be interpreted in conjunction with the follow-up period (Table 1). Iran had the lowest incidence. However, this finding was likely confounded by the short follow-up period (duration of hospital stay alone).
Outlining the spectrum of bacterial and fungal organisms involved in BSI is essential for the choice of prophylactic and empirical antimicrobials, especially in specialized populations such as pediatric LT recipients. The high prevalence of S. epidermidis and other gram-positive organisms is consistent with that in the general pediatric population [26].
However, gram-negative organisms occurred in BSI at a higher rate in LT recipients than in the general pediatric population. Kolesnichenko et al. [27] noted that the ratio of gram-positive to gram-negative organisms involved in BSI in the general pediatric population was 86%:11.6%, whereas our review found a ratio of 59.5%:40.5%.
Although the variable antibiotic regimens between centers (Table 3) could be due to local antibiograms and different resistance patterns, this finding emphasizes the need for empirical gram-negative coverage when choosing antimicrobials. Future studies are needed to examine whether there is a correlation between the use of certain antimicrobials and the incidence of BSI.
Identifying pre- and postoperative risk factors for BSI can potentially lead to stricter monitoring, with a lower threshold for collecting blood cultures and starting empiric antimicrobials in vulnerable groups. Many risk factors are shared between adult and pediatric LT recipients, including male sex, PELD/MELD score, operative time, blood loss, and ABO incompatibility [28]. However, some risk factors are unique to pediatric patients, such as biliary atresia as the underlying cause, younger age, and the graft-recipient body weight ratio.
A multicenter retrospective study of adult LT patients published in 2016 highlighted 2 important differences compared to our pediatric population: (1) the incidence of BSI was 29.4% (vs. the 24.6% rate found in our study in the pediatric population); (2) notably, an almost equal distribution of gram-positive (51%) and gram-negative (49%) organisms (vs. in the pediatric population, gram-positive organisms were more predominant at 59.5%). Another valuable observation was that older age was a significant risk factor in adults (vs. younger age in the pediatric population), suggesting that age extremes are a risk factor for BSI [29].
The limitations of our systematic review include the following: (1) different follow-up periods were used in the various selected articles, ranging from a few months to multiple years, suggesting that some late-onset BSI cases may have been overlooked; (2) multiple articles highlighted the risk factors for infection after pediatric LT without any BSI-specific risk factors, indicating that the information was not reported; and (3) certain populations, specifically in the US, were more fully represented (55% of the total population in our study) due to the higher research output.
In conclusion, bacterial BSI after pediatric LT has a high incidence, with a unique profile notable for a higher percentage of gram-negative organisms. Further studies are required to determine the most appropriate prophylactic and empirical antibiotic management strategies for this population.
Notes
Conflicts of interest
The authors have nothing to disclose.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors would like to thank Medstar Health, Georgetown University, Global Remote Research Scholars Program and Al Jalila Childrens’ Hospital for their continuous support.