Use of virtual reality in children in a broad range of medical settings: a systematic narrative review of recent meta-analyses
Article information
Abstract
Virtual reality (VR) is an emerging method that can be used in many scenarios involving children. VR has been increasingly studied as it has become cheaper, more widely available, and of better quality. In this review of current meta-analyses on the use of VR in children in the medical setting, we examined its role in 5 broad settings where it is used to alleviate pain and anxiety as well as in therapeutic scenarios. The study scope was purposefully broad to highlight a wide range of cases. We searched the ScienceDirect, SpringerLink, Cochrane Library, PubMed, and PMC databases for meta-analyses using VR in pediatric populations in medical settings. The National Institutes of Health quality assessment tool and Quality of Reporting of Meta-analyses statement checklist were used to verify study quality. Six hundred fifty-three articles were retrieved; after the application of the inclusion and exclusion criteria, 11 remained. These meta-analyses included cerebral palsy (4 meta-analyses), attention deficit/hyperactivity disorder (2 meta-analyses), burn care (1 meta-analysis), preoperative anxiety (2 meta-analyses), and needle-involving procedures (2 meta-analyses). The meta-analyses showed broadly positive results, with VR being useful in the areas in which it was applied. This study had several limitations. The meta-analyses consistently highlighted a high level of heterogeneity, making it challenging to draw clear conclusions. Most meta-analyses across all fields yielded encouraging results. However, further studies are required to confirm these findings. Guidelines must be established for future experiments to provide a standard and uniform procedure for reducing the heterogeneity of experimental methods.
Key message
· Virtual reality (VR) is becoming increasingly common for entertainment and in medical settings.
· VR is useful for treating children with cerebral palsy.
· VR can help with attention deficit/hyperactivity disorder symptoms.
· VR can decrease pain perception in children undergoing burn wound care.
· VR can reduce preoperative anxiety.
· VR can reduce fear and pain during needle-involving procedures.
Introduction
With the recent increase in the popularity and availability of virtual reality (VR) headsets, their use within hospitals has become more feasible for helping patients, with pediatrics being a fascinating use case.
VR is defined as an artificial environment experienced through sensory stimuli, generally auditory and visual, provided by a computer and headset combination in which one’s actions partially influence what happens in the environment [1]. Within this definition, however, there is a range of experiences, from relatively passive to very active, with various degrees of interaction with the virtual environment. VR is thought to function through distraction, helping users cope by paying less attention to painful, fear-inducing, or otherwise adverse stimuli [2].
Several studies have been conducted since the popularity of VR has increased. However, these studies often used small study groups, differing methodologies, and various hardware and software packages, thus rendering direct comparisons difficult. Many meta-analyses have aimed to draw conclusions regarding the effectiveness of VR in specific settings.
In this narrative review, we examine the current state of the literature and summarize recent meta-analyses conducted through July 2022 to provide a broad overview of VR use in pediatric medical settings. With our purposefully broad scope, we highlight the various benefits of VR to help clinicians become more aware of VR and provide a starting point for interested clinicians. Finally, we hope to help clinicians examine how VR technology can be useful in their practice.
We segmented our analysis along the lines of broad research areas because different use cases were not directly comparable. These categories include attention deficit/hyperactivity disorder (ADHD), burns, cerebral palsy (CP), needle-involving procedures, and preoperative anxiety.
Methods
This systematic review followed the updated 2020 version of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [3]. The review was not registered, and no protocols were prepared.
1. Inclusion criteria
Meta-analyses reporting the effects of VR on pediatric patients were considered eligible for review. For this study, pediatric patients were defined as those aged 18 and under, and no differentiation was made between the active and passive VR techniques. There were no limitations regarding study timing, setting, language, or date, and all studies involving a medical setting were included.
2. Exclusion criteria
Studies other than meta-analyses were not eligible for review. Meta-analyses that aimed to study the effects of tools other than VR were excluded. Meta-analyses of the use of VR in adult patients and studies with unverifiable data or that were lacking full-text availability were also excluded. Studies conducted outside medical settings were also excluded.
Some studies involved adults and children but provided a breakdown of their data according to age. If this was the case and a separate analysis of adults and children was possible, the pediatric data were extracted and analyzed.
3. Search strategy
Two authors conducted sequential searches of the PubMed, PMC, ScienceDirect, SpringerLink, and Cochrane Library databases. Multiple databases were searched to reduce selection bias. Furthermore, both British and American English spellings of “pediatrics” were used to avoid missing studies. The search terms used were: paediatric, pediatric, child, children, VR, virtual reality, and meta-analysis. Titles and abstracts were independently reviewed by 2 authors. In cases of disagreement, the decision to include a study was resolved through discussion. The full texts were examined by the same authors, and their acceptance or rejection was based on discussion. The references lists of the selected studies were manually reviewed to search for additional meta-analyses.
4. Data
Searches of various databases resulted in 653 matches (ScienceDirect, 127; SpringerLink, 237; Cochrane Library, 0; PubMed, 64; PMC, 225). Of these, 48 (ScienceDirect, 7; SpringerLink, 5; Cochrane Library, 0; PubMed, 27; and PMC, 9) were retained based on the title screening. Five additional studies were excluded based on the abstract screening. After duplicates were removed, 29 studies remained for review (ScienceDirect, 7; SpringerLink, 4; Cochrane Library, 0; PubMed, 24; PMC, 8). Four studies were excluded after the full-text review. The first was on the grounds of not being a meta-analysis,the second was on the grounds of containing only a single pediatric randomized control trial, and the last was because it was retracted after publication.
Fig. 1 shows a flowchart of the article selection process according to PRISMA guidelines.
Results
Following the selection process, 11 meta-analyses were included. The meta-analyses included in the study were then divided into subcategories based on the broad fields investigated and analyzed as separate groups to draw more cohesive conclusions.
Categories
· CP (4 studies)
· ADHD (2 studies)
· Burns (1 study)
· Preoperative anxiety (2 studies)
· Needle-involving procedures (2 studies)
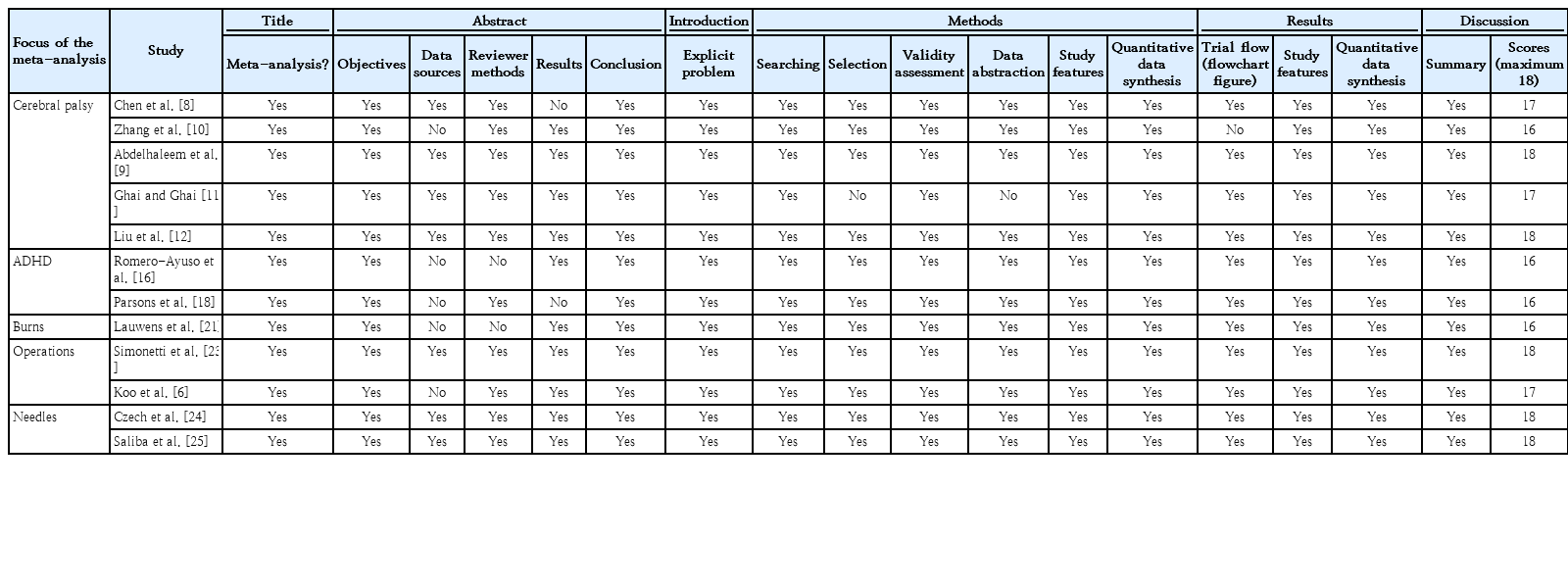
The meta-analyses were then analyzed using the eight-item National Institutes of Health (NIH) quality assessment tool to assess the quality of the meta-analyses and systematic reviews [4]. No studies had a score of <5 on the NIH scale (Table 1). Studies were also checked against the Quality of Reporting of Meta-analyses checklist used to assess the meta-analyses (Table 2) [5]. No study was found to have a score of less than 16. The main characteristics of the meta-analyses are presented in Tables 3–7.
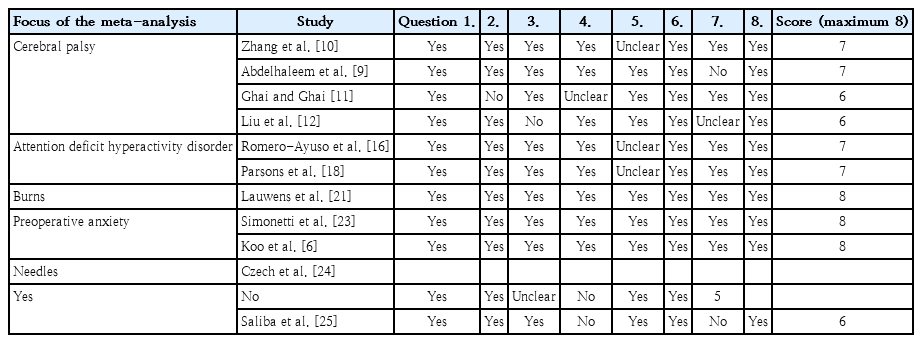
Meta-analyses rated according to the National Institutes of Health Quality Assessment of Systematic Reviews and Meta-Analyses
Of the meta-analyses selected for review, not all included pediatric populations exclusively. The meta-analysis of Koo et al. [6] was included since the pediatric data were clearly delineated, allowing its isolation and extraction; therefore, some conclusions could be drawn separately from the adult data. Data from studies that mixed adult and pediatric populations or mixed different types of distraction techniques were excluded.
Although the meta-analysis by Wu et al. [7] met the study inclusion criteria, it was rejected as it strayed from their inclusion criteria by including a passive VR study as well as featuring transcription errors regarding the numbers taken from the studies; as we assume the tables the authors presented in their paper were used for their meta-analysis, they were deemed unreliable. Therefore, the study was excluded from the analysis.
Owing to the small number of studies and the large amount of variability between them, no reliable measure of the certainty of each outcome was possible.
Discussion
1. CP patients may benefit from VR use in physical therapy
According to the Centers for Disease Control and Prevention, CP is among the most common motor disabilities in childhood, with an estimated prevalence of 1–4/1,000 births. All individuals with CP have motor function problems, resulting in struggles with posture, coordination, and balance, and often experience perception, cognition, and communication disturbances [8,9].
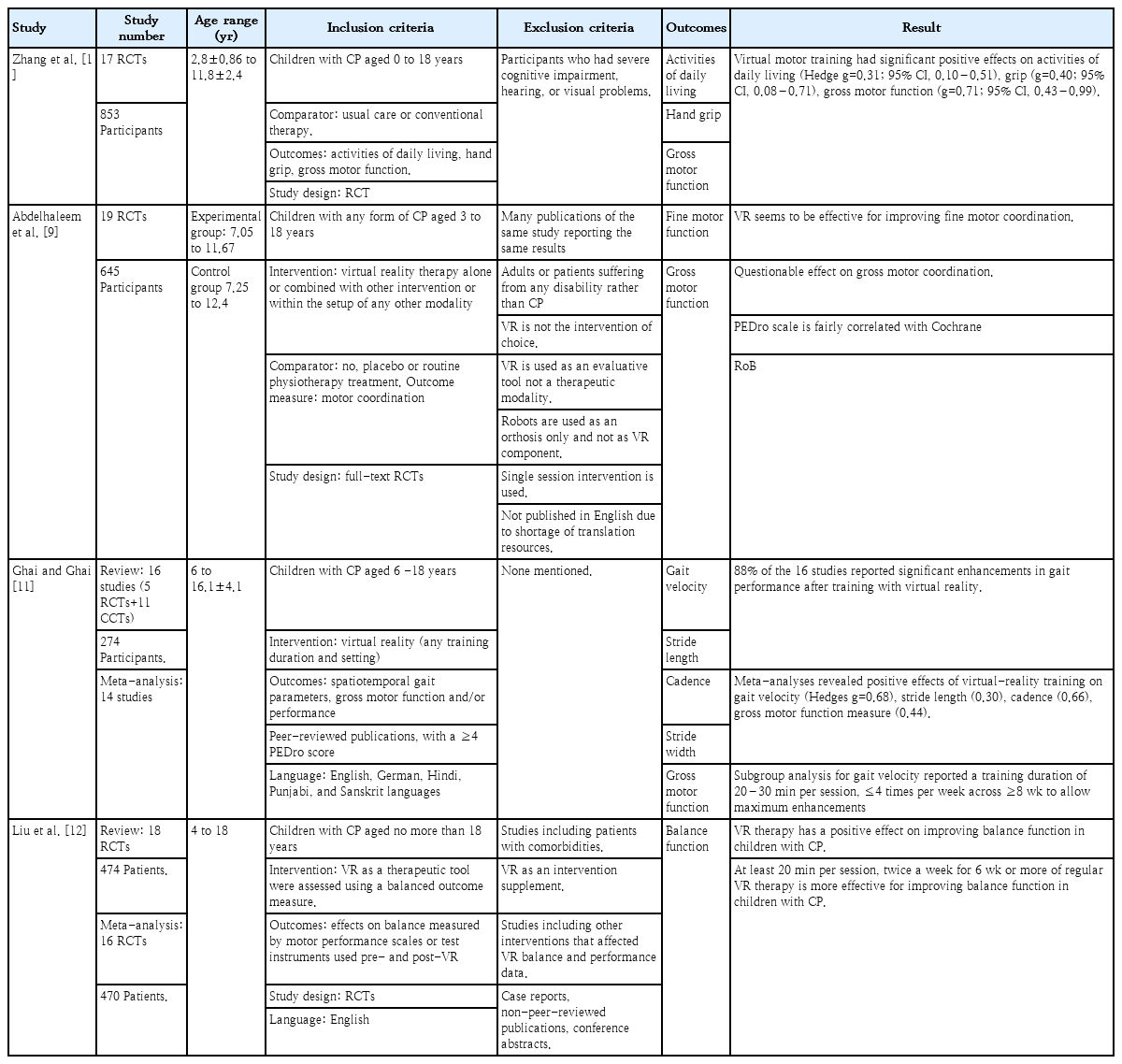
Zhang et al. [10] analyzed 17 randomized controlled trials (RCTs) incorporating 853 children with CP (aged approximately 2.8–11.8 years) that compared VR with conventional therapy or a control group to evaluate its effects on gross motor function, hand grip, and activities of daily living. The results revealed that VR had a positive impact on all 3 outcomes.
Abdelhaleem et al. [9] investigated 19 RCTs comprising 645 participants with a mean age of 7.05–11.67 years in the experimental VR group and 7.25–12.4 in the no VR control group [9]. Their meta-analysis identified moderate evidence of fine motor coordination in favor of VR therapy over usual care or no intervention; however, there evidence was conflicting regarding gross motor coordination.
Ghai and Ghai [11] included 14 studies (ages 6–16.1 years) in a meta-analysis that revealed the positive effects of VR training on gait velocity, stride length, cadence, and gross motor function in children with CP. A subgroup analysis found that a duration of 20–30 minutes per session ≤4 times per week across ≥8 weeks allowed maximum enhancements in gait velocity. However, the authors warned against cautiously interpreting this result because the subgroup analysis included only 6 studies.
Liu et al. [12], who compared 470 patients (ages 4–18 years) across 16 studies in a meta-analysis, found that VR therapy positively improves balance function in children with CP [12]. A subgroup analysis suggested that at least 20 minutes per session twice a week for 6 weeks or more of regular VR therapy is more effective at improving balance function in children with CP. However, it should be noted that 4 of the 16 studies did not support VR treatment over conventional treatment [12].
VR motor training in children with CP helps them overcome the specific challenges associated with traditional face-to-face rehabilitation: no appointment shortage, flexible training, easier progress monitoring, and increased motivation through game features, to name a few examples [8,10].
2. VR may benefit ADHD patients by increasing their attention
The use of VR in mental-health research has steadily evolved. First reserved for adults and applied mainly to the treatment of phobic disorders, its use has expanded to pediatric psychiatry. More fields are being explored, and ADHD is no exception [13,14]. This is particularly important, as ADHD is among the most common childhood and adolescent neurobehavioral disorders, with a prevalence of approximately 5.3% [15].
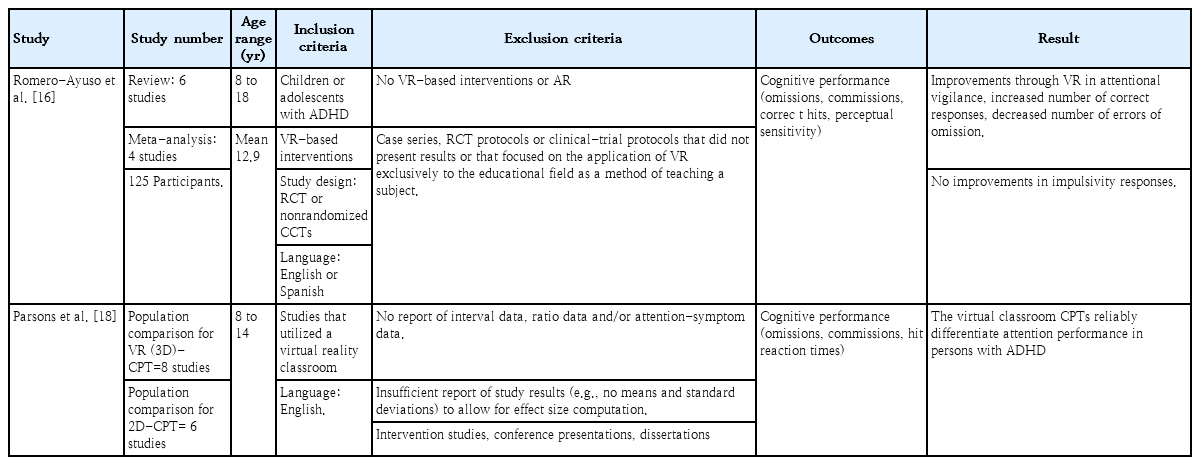
Romero-Ayuso et al. [16] performed a meta-analysis of 4 studies that included 125 diagnosed children that administered immersive VR-based interventions. Looking at 5 outcomes (omissions, commissions, correct hits, reaction time, and perceptual sensitivity), Romero-Ayuso et al. [16] reported improvements in attentional vigilance measures, which meant better cognitive performance, but no improvements in impulsive responses. The population had an average age of 12.9 years (range, 8–18 years), with 92% being male [16].
VR has also been studied as a potential aid in the diagnosing of ADHD [17,18]. Parsons et al. performed a meta-analysis to compare traditional continuous performance tests (CPTs) to VR-classroom CPTs [18]. The CPT is an assessment tool for attentional processing often used to support or rule out a diagnosis of ADHD [18]. Parsons et al. [18] hypothesized that, compared to traditional computerized 2-dimensional CPTs, 3-dimensional virtual classrooms offer a real-world dynamic simulation with distractors that mimic the conditions found in a youth classroom, thus offering more precise differentiation between persons with ADHD and typically developing controls. To remedy heterogeneity issues, the meta-analysis compared populations (i.e., control vs. ADHD) using each CPT modality. Six studies included both main comparisons, and 2 additional studies were included in the population comparison for VR-CPT [18]. The patients were 8–14 years old, and studies reported 28%–100% males [18]. The virtual classroom CPTs are relatively effective at differentiating between individuals with ADHD from a neuropsychological perspective [18]. However, general group differences were similar using traditional CPT, and the authors could not estimate the impact of the diagnostic and task reliability of virtual classroom CPTs [18].
3. Burn patients may benefit from VR during wound changes
Despite the awareness of the prevalence of burns in children and the severity of the associated pain, burn pain remains undertreated. To mitigate this issue, the medical community has investigated complementary analgesic methods to traditional pharmacological approaches for pain. Therefore, the widespread use of regional anesthesia and novel technologies such as VR have been increasingly investigated [19].
Patient immersion in interactive VR distracts them from painful stimuli and can decrease their pain perception [20].
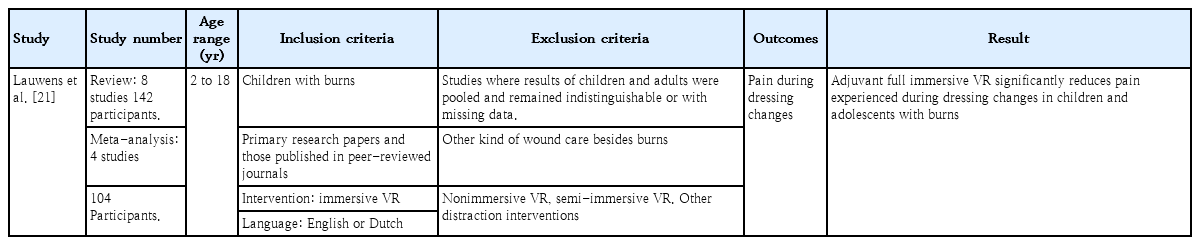
In their meta-analysis of 4 studies with 104 patients, Lauwens et al. [21] reported that VR adjuvant to standard care reduced pain during dressing changes in children and adolescents with second- and third-degree burns. However, it should be noted that the timing of VR application and self-reported pain assessment varied among studies [21].
Although we had to exclude the meta-analysis by Czech et al. [22] because its quantitative meta-analysis included both children and adults, the majority of the 13 articles examining VR and burn injuries in only children (6 months to 18 years) revealed that overall pain ratings were lower in groups of children additionally exposed to VR than in those who solely received the usual analgesics during burn care and postburn rehabilitation.
4. Preoperative anxiety may be reduced by VR use
Preoperative anxiety is a common problem affecting approximately 80% of surgical patients [6]. Preoperative anxiety can lead to worse outcomes and increased anesthesia requirements, making attempts to reduce it worthwhile [6,23]. To overcome this, VR can expose patients to a virtual operating room and surgical environment, helping dispel fears that may arise by habituating them in advance [6].
Furthermore, preoperative anesthesia involves many triggers of pediatric anxiety, including fear of the unknown, fear of potential pain, and parental separation [23]. By reducing the need for pharmacological forms of sedation, VR also reduces the potential risks [23]. VR is relatively simple and easy to implement in this use case, with no increase in healthcare costs [23].
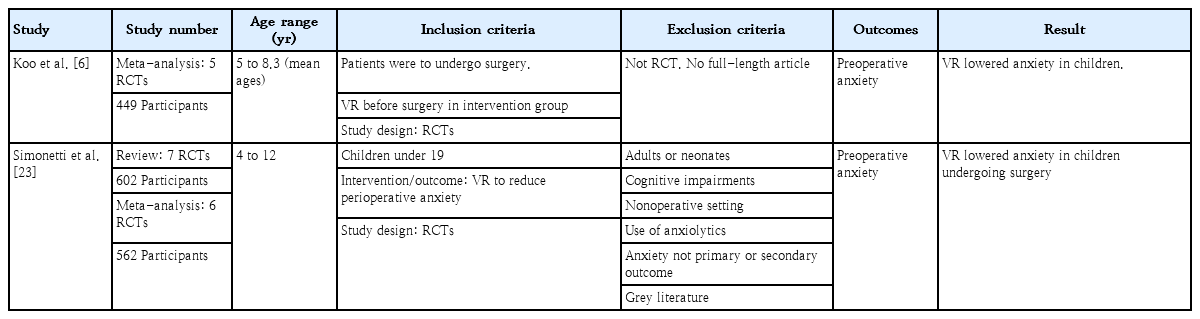
In a meta-analysis of 7 studies that included 602 patients aged 4–12 years, Simonetti et al. [23] found that VR reduced preoperative anxiety in children undergoing surgery. However, it did not improve compliance, pain, behavioral disturbances, or the emergence of delirium.
In a meta-analysis by Koo et al. [6] of 5 studies with a total of 409 patients aged 5–8 years, VR decreased preoperative anxiety in children but not adults. This is consistent with the findings of other studies, probably because children have higher baseline anxiety levels. It was concluded that the reasons for VR reducing anxiety included the ability to experience the operating environment beforehand, increasing their familiarity with it, and allowing them to dispel their imagined fears by picturing reality [6]. They also suggested that VR may be effective at causing distraction, making patients forget about their preoperative anxiety [6].
5. VR may reduce fear and anxiety about needle-involving procedures
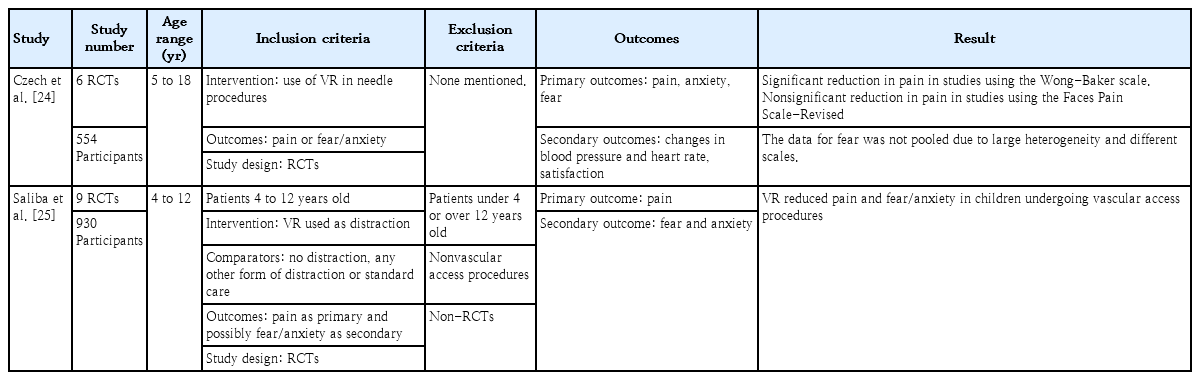
Czechet al. [24] examined the effects of VR onpainand fear/anxiety in children undergoing needle-related procedures in 7 studies. A statistically significant result was found in children regarding pain, showing that VR had a beneficial impact according to the Wong-Baker scale [24]. This positive effect was not found with the Faces Pain Scale-Revised, although the studies included in each analysis differed [24]. They could not pool data from studies that looked at fear and anxiety due to the large heterogeneity and the fact that they used different scales, making them unable to draw conclusions [24]. Their meta-analysis found no differences in patient satisfaction between the VR and standard care groups regarding patient satisfaction [24].
Saliba et al. [25] studied the effects of VR on pain and fear/anxiety in 10 studies including 930 patients aged 4–12 years who underwent needle-related procedures. They found that it reduced pain and fear/anxiety in patients undergoing needle-related procedures [25]. After examining the meta-regressions, they found that, contrary to the literature, passive cartoons seen in VR were more effective than active VR, but only for reducing fear [25]. Using meta-regressions, we also found that age did not have an effect, which contrasts with the literature.
However, this could be explained by the considerable age range in these studies [25]. In contrast to Czech et al. [24], Saliba et al. [25] did not find that the scale significantly reduced pain due to the effects of VR. They did not find a significant difference in the impact of VR on pain or fear/anxiety between phlebotomy and intravenous access placement [25]. Contrary to previous studies,they did not find that the sex of the patients significantly affected the effectiveness of VR [25].
6. Limitations
This systematic narrative review had some limitations. The heterogeneity in the results of various meta-analyses was due to differences in hardware, software, and protocols used among studies. This was echoed by all the meta-analyses, which draws attention to the fact that no standard protocol has been established and a lack of best practices prevents uniformity; thus, a direct comparison of the studies was impossible. This was further complicated by the vast array of hardware and software possibilities, with none being favored by researchers, a problem that will likely only increase as options broaden. Participant blinding is another problem, as it is impossible to do so with VR headsets, making it a likely unavoidable issue. Finally, most studies included in the meta-analyses had a limited number of participants, a fact recognized by most authors in their own analyses.
7. Recommendations
Standardized protocols and best practices must be developed and applied to address these problems. One example is the application protocol for VR glasses and the timing of the VR experience before the procedure. As it is impossible to standardize hardware and software among research groups, this is unlikely to occur anytime soon. However, developing best practices to create a standard protocol is essential for future research to make studies more comparable and increase the quality of future meta-analyses.
Conclusion
The use of VR in pediatric populations has been studied in various settings, with at least one positive result reported for patients in each category. This led us to conclude that VR is likely to be beneficial in the settings included here with little risk of associated harm.
Unfortunately, our optimism is somewhat tempered by the limitations of the current research in the field, with a need for more consensus regarding protocols and methods to reduce high study heterogeneity. However, these problems may be overcome by the agreement upon and implementation of standard practices for VR studies.
As the cost of hardware decreases and its availability increases, it has the potential to become a valuable tool in multiple routine practice settings as demonstrated by the wide variety of use cases explored.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.